What’s Killing Our Children? Child and Infant Mortality among American Indians and Alaska Natives
As an obstetric resident I once took care of a young Native American woman who had been transported by helicopter from a remote rural community because she had been assaulted by her intoxicated partner. She was early in her third trimester, and the damage to her face and extremities was dramatic but not life-threatening. However, the trauma to her abdomen resulted in a fracture of the femur of her unborn 28-week-old female fetus. Our team recognized that while we could successfully get her safely through her pregnancy, the real challenges she and her daughter faced would come upon her return home. For American Indian people, context matters and is a key determinant of health and mortality. We need to examine what’s really killing our children across a spectrum of health indicators, and public health needs to intervene at all levels. – Francisco Garcia, MD, MPH
The very vulnerable demographic group of American Indian and Alaska Native (AIAN) youth face unique and important challenges. We need to hear from native stakeholders and experts in American Indian health about the contextual factors (poverty, low educational attainment, and substance abuse) that represent a threat to native communities in this country. To begin to mitigate that threat, researchers, opinion leaders, human services providers, and the general population need to begin to understand what is killing native children [1].
In this paper we use the lens of infant and childhood mortality as a tool to recognize opportunities for action that could have an impact on this perhaps most critical indicator of the health of this population. We attempt to extract some lessons from the lived experiences of too many reservation and urban Indian communities and turn these tragic stories into useful tools for broader policy and health system change.
Public health has long used such mortality statistics to create a picture of the health of the community. In a recent article, Wong et al. (2014) used a novel technique—data linkage—to create a unique dataset matching Indian Health Service (IHS)-eligible participants with vital statistics for AIAN child and infant mortality rates by region. By reducing racial misclassification through this method, the authors present the patterns of AIAN infant and child mortality experienced by AIAN as compared to white infants and children, creating a frightening picture of problems affecting AIAN children, families, and communities.
This paper discusses AIAN infant and child death in an effort to understand the root causes of significant disparities and calls for serious efforts by public health and health care institutions for prevention and intervention to address core problems. We begin by drawing attention to the importance of understanding the problems in data for AIAN populations and the need to continuously improve data collection and analysis for the population. We conclude with opportunities for action, particularly for policy makers.
The Need to Reduce Misclassification on Death Certificates
Identification of AIAN status is an influential factor in U.S. vital statistics data and is influenced by historical, political, legal, and cultural definitions. There are 567 federally recognized tribes in the United States and 76 state-recognized tribes, as well as people who self-identify as AIAN and belong to terminated tribes or unrecognized tribes because they cannot document their family history. Racial identity is determined on birth certificates generally by the mother and is presumed to have a high rate of accuracy. In some tribes, however, citizenship follows one parent over the other. In matriarchal tribes, for example, if the father is AIAN and the mother is not, the child may not receive tribal membership.
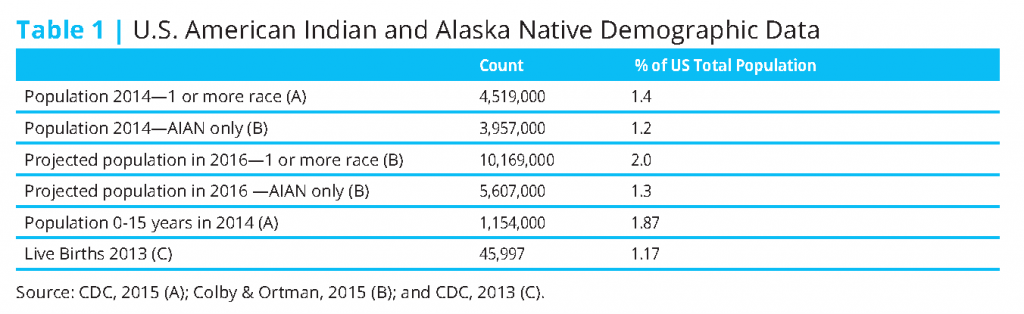
Racial identity for the purpose of the death certificate may be determined by a parent or other family member, but more likely it will be reported by a physician, coroner, or mortician, creating an increased risk for misclassification by race. Such misclassification would underestimate the deaths of the population. Espey and colleagues (Espey et al., 2014; Espey et al., 2005) have used a data linkage [2] process to reduce racial misclassification of AIAN in mortality data and cancer incidence data. Such efforts have enhanced our understanding of native health disparities and highlighted differences among the population by region. Table 1 illustrates the variability in AIAN demographics.
Differences in Data
According to the 2010 U.S. vital statistics, infant mortality appears to be decreasing at dramatic rates across the United States but particularly in AIAN communities (Hamilton et al., 2013). In 1915, the total U.S. infant mortality rate was as high as 99.9/1,000 births. By 2010, the rate had dropped to 6.1/1,000. The dramatic decline can be primarily attributed to prevention and control of infectious disease through public health measures. Trends for AIAN infant mortality also appear to be declining, from 62.7/1,000 in 1955 to 8.3/1,000 in 2010; however, there is variation across states and regions of the United States, with New Mexico reporting the lowest infant mortality rate for AIAN at 5.0/1,000 and North Dakota reporting one of the highest at 16.6/1,000 (Hamilton et al., 2013).
Leading Causes of Death
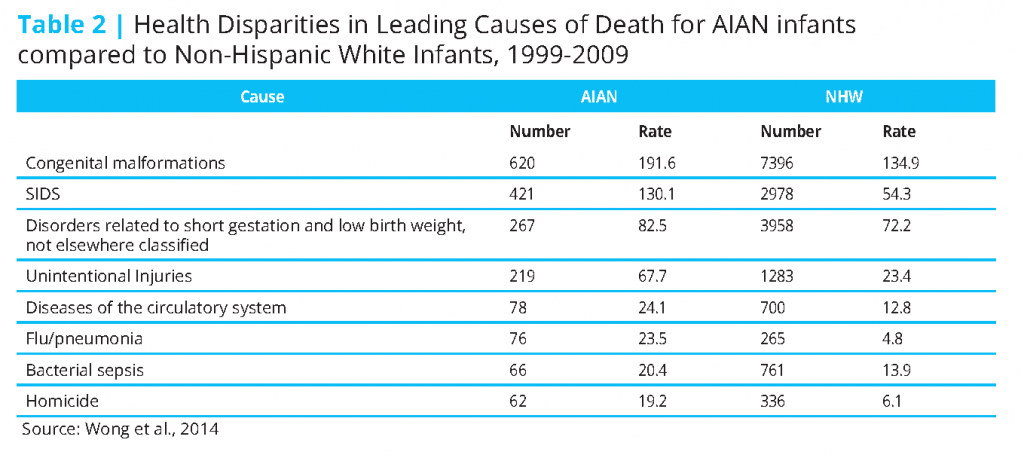
Wong et al. (2014) report disparities in the infant death rates between AIAN and whites. Infant mortality was significantly higher among AIAN across the age span as compared to non-Hispanic white mothers. The AIAN infant death rate for the period of 1999–2009 was almost double (914.3/100,000 AIAN, 567.3/100,00 white), and the postneonatal (age 28–364 days) rate (53 percent) was significantly higher than the white rate (34 percent); the neonatal (< 28 days) rate was significantly higher as well (434/100,000).
In general the leading causes of death for AIAN children less than 1 year of age can be grouped into three different diagnostic categories: congenital malformations, sudden infant death syndrome (SIDS), and unintentional injuries (Wong et. al, 2014). AIAN infants and neonates also died of medical conditions resulting from short gestation and low birth weight; maternal complications of pregnancy; complications of placenta, cord, and membranes; and bacterial sepsis. Infants also suffered from diseases of the circulatory system, influenza and pneumonia, and homicide. Neonates also died of necrotizing enterocolitis (inflammation of the intestines), respiratory distress and intrauterine hypoxia (deprivation of an adequate amount of oxygen), neonatal hemorrhage, and birth asphyxia (failure to initiate and sustain breathing at birth). After the first year of life, mortality in AIAN children shifts largely to accidental and nonaccidental trauma, including homicide and suicide, accounting for 41 percent of all deaths among AIAN children (Wong et al., 2014). All of the top 10 causes of death for this population were significantly higher than the white rates. The causes with the largest disparities between AIAN children and their white counterparts were flu/pneumonia, meningitis, and homicide (Wong et al., 2014).
Beyond the significant disparities in overall rates, the study team also found significant disparities in specific causes by age. SIDS was one of the top 10 causes across the three age categories, with AIAN infant rates double the rates for white infants. SIDS rates in Alaska and the Northern Plains were four times higher among AIAN infants than among white infants. Such high rates have been documented for more than 25 years (Wong et al., 2014). Of all the deaths among AIAN children, unintentional injuries accounted for 41 percent.
Causes Relevant to Prenatal Care
Birth defects such as congenital malformations, diseases of the circulatory system, and those resulting from short gestation period, low birth weight, or necrotizing enterocolitis have varied or unknown causal links and are difficult to prevent. However, education through prenatal care may be an avenue to reducing risk relative to the mother’s behavior, including alcohol and tobacco consumption, stress, and reduced exposure to environmental toxins. Prenatal care provides access to imaging and is typically the pathway for detecting potential birth defects. Despite this, prenatal care utilization is typically low in AIAN populations, as with other low-income populations (IHS, 2005; APA, 2014). The prenatal care participation rate for on-reservation women served by IHS is low (67 percent) compared to the U.S. all-races rate of 81 percent (IHS, 2005; APA, 2014). This finding is crucial because prenatal care and childbirth classes represent critical opportunities to deliver health education messages to decrease the risk of SIDS and unintentional injuries.
Causes Relevant to Mode of Delivery
Maternal complications at the time of delivery and during the puerperium [3] are exacerbated in the absence of appropriate birthing environments, access to the appropriate level of perinatal care of complications, and emergency maternal transport when that care is not readily available. Of the 1.36 percent of births that occurred outside of a medical facility in 2012, most were among American Indian women (0.81 percent), a trend that has been slowly increasing since 1990 (MacDorman et al., 2014). This may be the result of the distance women have to travel to a hospital when living in remote/rural areas, a lack of facilities, and/or a lack of insurance coverage for urban Natives, as well as cultural or historical birthing patterns.
Causes Relevant to Pediatric Care
Pediatric care also represents an opportunity to prevent or mitigate important causes of mortality for AIAN children. Pediatric encounters provide an opportunity for maternal education and support for healthy infant sleep habits to prevent SIDS and vaccinations to decrease the risks of preventable infectious diseases. Conditions such as gastritis, duodenitis (inflammation of the duodenum), and meningitis can also be diagnosed during the pediatric visit.
According to a 2011 survey of physician practice patterns within IHS, important capacity limitations exist with a limited number of pediatric providers. Pediatricians and pediatric nurse practitioners represent only about 8 percent of Indian Health Service providers; however, more than 82 percent of respondents of a survey of IHS providers reported that they are engaged in primary care, including pediatrics. The IHS patient-physician interaction ranges from 0–39 minutes, with the average time being 19 minutes. The average wait time for an appointment is approximately 2.7 days for urgent issues, compared to 2.6 days for non-IHS programs, and the average wait time for an appointment for a nonurgent health matter is 10.5 days, compared to 8 days for non-IHS physicians. IHS physicians have recognized that primary care physicians are urgently needed (IHS, 2011).
Causes Relevant to Public Health
Childbirth and parenting education for new mothers and mothers-to-be are critical to provide a healthy environment for infants and children. Likewise, population campaigns that seek to increase participation in prenatal care are important to reset cultural norms and promote broader engagement with the health care system. Other public health efforts may also impact the excess mortality that is experienced by AIAN children, including the following: (1) short gestation and low birth weight, (2) SIDS, (3) influenza and pneumonia, and (4) unintentional injury, homicide, and suicide.
Short Gestation and Low Birth Weight
In 2013 the rate of preterm births for AIAN was 13.04 per 100 live births, a slight decrease from 2012 (13.25 per 100 live births) (Hamilton et al., 2014). This rate was the second highest for all racial/ethnic categories and only lower compared to non-Hispanic black infants (16.26 per 100 live births) (Hamilton et al., 2014). The AIAN rate of low-birth-weight babies in 2013 was 7.46 per 100 live births, down from the 2012 rate of 7.61 per 100 live births, compared to the rate for non-Hispanic white infants (6.97 per 100 live births) (Hamilton et al., 2014).
Premature births and low-birth-weight infants are related to adolescent maternity (Martin et al., 2007). For AIAN populations the elevated rates of teen pregnancy are an important causal factor that contribute to this important source of morbidity. Teen pregnancy prevention programs that encompass education, clinical services, and peer support are a cornerstone service for public health. Not only do such initiatives have an impact on the preterm and low-birth-weight infants but also children in these categories may be at the greatest risk for SIDS.
Sudden Infant Death Syndrome
The overall AIAN death rate for SIDS among infants is more than double that for the non-Hispanic white population (MacDorman and Mathews, 2011). This disparity cannot be explained by economic status, maternal age, birth weight, or prenatal care; however, there is a correlation with maternal behaviors that may be more common in AIAN communities, including smoking, cosleeping associated with inadequate housing, excessive clothing of the infant, and maternal alcohol use (Trachtenberg et al., 2012; Bureau of the Census, 2003; Blum et al., 1992; Grossman et al., 1997; May, 1994). Despite these underlying contextual challenges, education campaigns have been effective in decreasing SIDS through improving infant sleep practices (Healthy Child Care America, 2014). In recent years the number of babies who died of SIDS and who had been sleeping on their stomachs at the time of death decreased by 35.3 percent (Trachtenberg et al., 2012).
Vaccine-Preventable Illness
AIAN children had significantly higher death rates caused by vaccine-preventable influenza and pneumonia across all age groups. Disparities persist despite an overall decline, with the highest rates of illness in the Southwest and Alaska Native communities. This may be exacerbated by crowded living conditions in reservations or rural villages (Bureau of the Census, 2003).
Flu and pneumonia are easily prevented through adequate vaccination programs, and the IHS began a vigorous immunization program for Haemophilus type B (to prevent meningitis) and pneumococcal pneumonia. Overall, however, AIAN youth have lower vaccine rates in comparison to non-Hispanic whites.
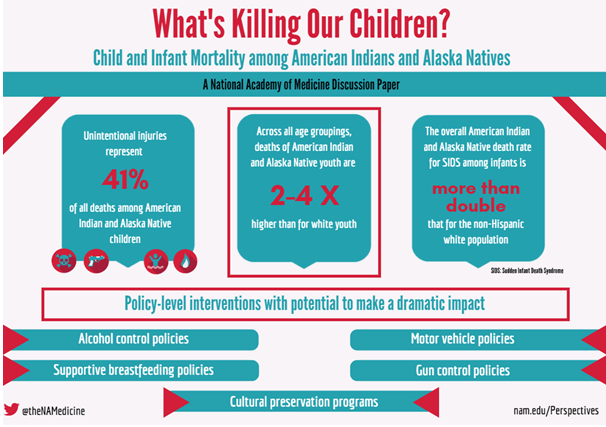
Unintentional Injuries and Suicide
Perhaps most remarkable is the finding that unintentional injuries represent 41 percent of all deaths among AIAN children and are the leading cause for all age groups (after the first year). Deaths from unintentional injuries include drowning, fire, poisoning, and firearm-related deaths, and these rates are significantly higher for AIAN youth in all age groups (Wong et al., 2014). Death rates from unintentional injuries were highest in Alaska, the Northern Plains, and the Southwest, with most attributed to motor vehicle crashes. Across all age groupings, deaths of AIAN youth were two to four times higher than for white youth.
The effectiveness of automobile safety programs such child safety seats, seat-belt usage, and drunk driver prevention should be examined because automobile accidents continue to be the leading cause of death in this category. Of AIAN youth surveyed, 44 percent report never wearing a seat belt, and 38 percent report drinking and driving (Blum et al., 1992), common behaviors among drivers in rural communities (Grossman et al., 1997).
The second leading cause of death for AIAN youth and young adults aged 10–34 was suicide. Not only is suicide completion more common among AIAN children but also reported attempts at self-harm are significantly higher, with 21.6 percent of AIAN females and 11.8 percent of AIAN males reporting at least one suicide attempt (Blum et al., 1992).
Opportunities for Action
Linking health disparities directly to causal factors is challenging. Nonetheless, several potential factors lend themselves to public health action, including prevention and public health interventions such as immunizations and prenatal care. Table 3 illustrates the ages at which targeted interventions could impact child and infant mortality.
In addition to targeting specific interventions at specific age groups, public health initiatives should also target key points along the socioecological framework, including not only opportunities for individual education but also policy-level interventions that have the potential to make a dramatic impact. These interventions include alcohol control policies, supportive breastfeeding policies, motor vehicle policies, gun control policies, and cultural preservation programs. Each is discussed in turn below.
Alcohol Control Policies
As discussed earlier in this paper, mortality among 1–19 year olds is due to unintentional injuries. Although underlying causes for unintentional injuries are likely multifactorial, there is evidence of links to substance abuse (Hingson et al., 2009). May (1994) estimates that in reservation states, alcohol is an underlying cause in 65 percent of the motor-vehicle-related deaths, 75 percent of suicides, and 80 percent of homicides. The Guide to Community Preventive Services (2016) identifies eight community policies found to be effective reduction strategies: (1) increasing alcohol taxes, (2) holding alcohol retailers liable for injuries or deaths caused by intoxicated and underage patrons, (3) controlling the number of alcohol outlets in a community, (4) providing counseling services through electronic screening and brief intervention methods, (5) enforcing minimum drinking-age laws, (6) limiting the privatization of retail alcohol, (7) limiting the number of days of sales, and (8) limiting the hours of sales. However, even reservations that ban alcohol are often surrounded by alcohol shops in bordering communities, making the ban ineffective. Therefore, policies have to go beyond the tribal government and extend to adjoining county and state governments. Public health practitioners can make a significant impact by building partnerships with neighboring public health and other governmental agencies.
Supportive Breastfeeding Policies
Breastfeeding is a protective factor in SIDS and may be especially important for small-gestational-age infants. Public health interventions are critical to creating a supportive cultural environment for breastfeeding. Such actions include individual-level interventions, such as lactation education, and policy-level interventions, such as the availability of lactation rooms, social support, and policies that facilitate good lactation practices during the first year. The CDC also recommends developing written policies within hospitals and other delivery sites that address (1) ensuring mothers get adequate prenatal and postnatal care and education, (2) training staff and providing skills training for the mothers, (3) encouraging breast milk for the baby in the hospital unless otherwise medically indicated, (4) allowing for mother and child to be in the same room for 24 hours, and (5) other breastfeeding-promoting behaviors (CDC, 2013). The CDC also recommends the development of written policies for worksites, policies that would include providing mothers with a private place to breastfeed or express milk, allowing for a flexible schedule for maternity leave, and providing on-site child care (CDC, 2013).
Motor Vehicle Policies
Child seat-belt and car-seat safety programs and policies have been shown to reduce deaths from unintentional injuries caused by motor vehicle accidents. Community education programs in seat-belt safety and car-seat installation often improve adherence and lend support to such laws (Ebel et al., 2003). Programs that provide free infant and child car seats, such as those through the IHS or the CDC, are particularly important in Indian country for those who cannot otherwise afford one or enough for all the children in the family.
The CDC Community Preventive Services Task Force also recommends that laws be put in place, enhanced, or strengthened to improve safety, including (1) zero tolerance for alcohol-impaired driving for youth/inexperienced drivers, (2) intoxicated-driver blood alcohol level limits set at 0.08 percent, (3) minimum age for alcohol drinking, and (4) enhanced motorcycle helmet use requirements. The task force recommends community-mobilized, multicomponent programs, which may include ignition control devices that prevent a vehicle from starting unless the driver meets a preset blood alcohol content level, sobriety checkpoints, and mass media campaigns (Shults et al., 2001).
Rural and remote reservation roads should be given particular consideration. These roads often have just two lanes with inadequate lighting, paving, or signage and do not have shoulders, medians, pedestrian or bicycle lanes or crossings, rumble strips, traffic control devices for speed management, or rail guards. Such conditions can be trying in good weather and are particularly hazardous in inclement weather. Wildlife and free-ranging cattle or horses may also pose additional hazards where visibility is low and road conditions are inadequate. The design and implementation of road infrastructure and motor vehicle safety programs would benefit from using a community-engaged model.
Gun Control Policies
Gun control laws may reduce suicide completion rates and violent injuries. Violence prevention programs across the lifespan, from childhood bullying to domestic violence, are key to preventing fatal unintentional and intentional injuries. Although limited, research has shown that gun control initiatives can be effective in violence prevention. These initiatives include the following (1) physician-patient discussions on firearm and ammunition storage (Albright and Burge, 2003); (2) limitations and bans on assault weapons and large-capacity magazines (Law Center to Prevent Gun Violence, 2016a,b); (3) consumer product regulations on the safety of guns and other weapons (Johns Hopkins Center for Gun Policy and Research, 2012); and (4) regulation and inspection of retail firearm dealers (Webster et al., 2009).
Cultural Preservation Programs
Family and community connectedness, spirituality, cultural identity, and other cultural norms have been found to be protective factors and to be as effective in improving health as reducing risk factors (Borowsky et al., 1999; Resnick et al., 1993; Mohatt et al., 2007). Programs that combine risk-factor reduction and cultural preservation will make a greater impact at the individual and community level in reducing a number of health concerns, including suicide, alcohol and substance abuse, sexual-risk behaviors, homicide, and bullying and other violent behavior.
Summary
Multiple factors underlie the negative health outcomes in infant and child mortality rates among AIAN. These factors include social, behavioral, and environmental ones that affect the mother and the child, such as domestic violence and stress, nutrition, tobacco and alcohol use, pollution, and environmental degradation. Factors such as maternal self-care, positive behavioral practices, primary health care access and utilization, and infant care issues are complex and difficult to address. But tribal and public health agencies can make a dramatic impact by using programs, policies, and services and advocating for laws known to effectively lower such disparities. A socioecological approach that encompasses environmental and sociocultural, as well as behavioral, approaches is required. This effort includes involving community or tribal agencies from economics, housing, labor, education, culture, transportation, justice, behavioral health, social services, and medicine. Developing public health entities on reservations to coordinate with state, county, and municipal health departments will enhance tribal efforts and improve access to resources.
Notes
- For the purposes of this paper, “children” are defined as those aged birth–18 years.
- Data linking is a process to improve racial classification by linking one dataset (IHS records) to another data set (vital records) and identifying those that appear to have been misclassified.
- The time during which physiologic changes women experience while pregnant revert back to normal (CDC, 2007).
Download the graphic below and share it on social media!
References
- Albright, T. L., and S. K. Burge. 2003. Improving firearm storage habits: Impact of brief office counseling by family physicians. Journal of the American Board of Family Practice 16(1):40–46. https://doi.org/10.3122/jabfm.16.1.40
- APA (American Psychological Association). 2014. Fact sheet: Women and socioeconomic status. Available at: http://www.apa.org/pi/ses/resources/publications/factsheetwomen.aspx (accessed February 1, 2017).
- Blum, R. W., B. Harmon, L. Harris, L. Bergeisen, and M. D. Resnick. 1992. American Indian–Alaska Native youth health. JAMA 267(12):1637–1644. https://doi.org/10.1001/jama.1992.03480120075036
- Borowsky, I. W., M. D. Resnick, M. Ireland, and R. W. Blum. 1999. Suicide attempts among American Indian and Alaska Native youth: Risk and protective factors. Archives of Pediatrics and Adolescent Medicine 153(6):573–580. https://doi.org/10.1001/archpedi.153.6.573
- Bureau of the Census. 2003. 2000 census of populations and housing, characteristics of American Indian/Alaska Natives by tribe and language. Available at: https://www.census.gov/prod/cen2000/phc-5-pt1.pdf (accessed August 14, 2020).
- CDC, 2007. Maternal Mortality and Related Concepts. Hyattsville: U.S. Department of Health and Human Services. Available at: https://www.cdc.gov/nchs/data/series/sr_03/sr03_033.pdf (accessed January 31, 2017).
- CDC. 2013. Strategies to prevent obesity and other chronic diseases: The CDC guide to strategies to support breastfeeding mothers and babies. Atlanta: U.S. Department of Health and Human Services. Available at: http://
www.cdc.gov/breastfeeding/resources/guide.htm (accessed January 31, 2017). - CDC. 2015. Health, United States 2015. Atlanta: U.S. Department of Health and Human Services. Available at: http://www.cdc.gov/nchs/data/hus/hus15.pdf (accessed January 31, 2017).
- Colby, Sandra L. and Jennifer M. Ortman. 2015. Projections of the Size and Composition of the U.S. Population: 2014 to 2060, Current Population Reports, U.S. Census Bureau, Washington, DC, 2014. Available at: https://www.census.gov/content/dam/Census/library/publications/2015/demo/p25-1143.pdf (accessed August 14, 2020).
- Ebel, B.E., T.D. Koepsell, E.E. Bennett, and F.P. Rivara. 2003. Use of child booster seats in motor vehicles following a community campaign. JAMA 289(7):879-884. https://doi.org/10.1001/jama.289.7.879
- Espey, D. K., M. A. Jim, T. B. Richards, C. Begay, D. Haverkamp, and D. Roberts. 2014. Methods for improving the quality and completeness of mortality data for American Indians and Alaska Natives. American Journal of Public Health 104(Suppl 3):S286–S294. https://doi.org/10.2105/AJPH.2013.301716
- Espey, D., R. Paisano, and N. Cobb. 2005. Regional patterns and trends in cancer mortality among American Indians and Alaska Natives, 1990–2001. Cancer 103(5):1045–1053. https://doi.org/10.1002/cncr.20876
- Grossman, D. C., J. R. Sugarman, C. Fox, and J. Moran. 1997. Motor-vehicle crash-injury risk factors among American Indians. Accident Analysis and Prevention 29(3):313–319. https://doi.org/10.1016/S0001-4575(96)00085-1
- Guide to Community Preventive Services. 2016. Preventing excessive alcohol consumption. Available at: www.thecommunityguide.org/alcohol/index.html (accessed February 1, 2017).
- Hamilton, B. E., D. L. Hoyert, J. A. Martin, D. M. Strobino, and B. Guyer. 2013. Annual summary of vital statistics: 2010–2011. Pediatrics 131(3):548–558. https://doi.org/10.1542/peds.2012-3769
- Hamilton, B. E., J. A. Martin, M. J. K. Osterman, and S. C. Curtin. 2014. Births: Preliminary data for 2013. Centers for Disease Control and Prevention, National Vital Statistic Reports. Available at: http://www.cdc.gov/nchs/data/nvsr/nvsr63/nvsr63_02.pdf (accessed February 1, 2017).
- Healthy Child Care America. 2014. HCCA safe sleep campaign. Available at: http://www.healthychildcare.org/sids.html (February 1, 2017).
- Hingson, R.W., E.M. Edwards, T. Heeren, and D. Rosenbloom. 2009. Age of drinking onset and injuries, motor vehicle crashes, and physical fights after drinking and when not drinking. Alcoholism: Clinical and Experimental Research 33(5):783-790. https://doi.org/10.1111/j.1530-0277.2009.00896.x
- IHS. 2005. Regional differences in Indian health, 1998–1999. Available at: http://hdl.handle.net/1928/27348 (accessed January 31, 2017).
- IHS. 2011. 2011 survey of physician practice patterns and satisfaction. Available at: http://www.npaihb.org/images/resources_docs/QBM%20Handouts/2013/April/8%20-%20IHS%20%20Physician%20Survey%20Final.pdf (accessed January 31, 2017).
- Johns Hopkins Center for Gun Policy and Research. 2012. The case for gun policy reforms in America. Available at: http://www.jhsph.edu/research/centers-and-institutes/johns-hopkins-center-for-gun-policy-and-research/ publications/WhitePaper020514_CaseforGunPolicyReforms.pdf (accessed January 31, 2017).
- Law Center to Prevent Gun Violence. 2016a. Assault weapons policy summary. Available at: http://smartgunlaws.org/assault-weapons-policy-summary (accessed January 31, 2017).
- Law Center to Prevent Gun Violence. 2016b. Large capacity magazines policy summary. Available at: http://smartgunlaws.org/large-capacity-ammunition-magazines-policy-summary (accessed January 31, 2017).
- MacDorman, M. F., and T. J. Mathews. 2011. Understanding racial and ethnic disparities in U.S. infant mortality rates. National Center for Health Statistics Data Brief. Hyattsville, MD: National Center for Health Statistics. Available at: https://www.sedgwickcounty.org/media/30051/understanding-racial-and-ethnic-disparities-in-us-infant-mortality-rates.pdf (accessed August 14, 2020).
- MacDorman, M. F., T. J. Mathews, and E. Declerq. 2014. Trends in out-of-hospital births in the United States, 1990–2012. Hyattsville, MD: National Center for Health Statistics. Available at: https://pubmed.ncbi.nlm.nih.gov/24594003/ (accessed August 14, 2020).
- Martin J. A., B. E. Hamilton, P.D. Sutton, S. J. Ventura, F. Menacker, S. Kirmeyer, and M. L. Munson. Births: Final data for 2005. 2007. National Vital Statistics Reports 56(6), Hyattsville, MD: National Center for Health Statistics. Available at: https://pubmed.ncbi.nlm.nih.gov/18277471/ (accessed August 14, 2020).
- Mathews, T. J., M. F. MacDorman, and M. E.Thoma. Infant mortality statistics from the 2013 period linked birth/infant death data set. 2015. National Vital Statistics Reports 64(9). Hyattsville, MD: National Center for Health Statistics. Available at: https://pubmed.ncbi.nlm.nih.gov/26270610/ (accessed August 14, 2020).
- May, P. 1994. The epidemiology of alcohol abuse among American Indians: The mythical and real properties. American Indian Culture and Research Journal 18(2):121–143. https://doi.org/10.17953/aicr.18.2.q8j5786253540887
- Mohatt, G. V., R. Plaetke, J. Klejka, B. Luick, C. Lardon, A. Bersamin, S. Hopkins, et al. 2007. The Center for Alaska Native Health Research Study: A community-based participatory research study of obesity and chronic disease-related protective and risk factors. International Journal of Circumpolar Health 66(1):8–18. https://doi.org/10.3402/ijch.v66i1.18219
- NCHS (National Center for Health Statistics). 2016. Health, United States, 2015: With Special Feature on Racial and Ethnic Health Disparities. Hyattsville, MD.: Centers for Disease Control and Prevention. NCHS. National Vital Statistics Reports. 2015. V64, (9). Available at: https://www.cdc.gov/nchs/data/hus/hus15.pdf (accessed August 14, 2020).
- National Vital Statistics Reports: Table 4. Live births, infant, neonatal, and postneonatal deaths, and mortality rates, by race and Hispanic origin of mother and birthweight: United States, 2013 linked file, and percent change in birthweight-specific infant mortality, 2005 and 2013 linked file—s Con. p20. Available at: http://www.cdc.gov/nchs/data/nvsr/nvsr64/nvsr64_09.pdf (accessed January 31, 2017).
- Resnick, M. D., L. J. Harris, and R. W. Blum. 1993. The impact of caring and connectedness on adolescent health and well-being. Journal of Paediatrics and Child Health 29(Suppl 1):S3–S9. https://doi.org/10.1111/j.1440-1754.1993.tb02257.x
- Shults, R. A., R. W. Elder, D. A. Sleet, J. L. Nichols, M. O. Alao, V. G. Carande-Kulis, S. Zaza, D. M. Sosin, R. S. Thompson, and the Task Force on Community Preventive Services. 2001. Reviews of evidence regarding
interventions to reduce alcohol-impaired driving. American Journal of Preventive Medicine 21(4S):66-88. https://doi.org/10.1016/s0749-3797(01)00381-6 - Trachtenberg, F. L., E. A. Haas, H. C. Kinney, C. Stanley, and H. F. Krous. 2012. Risk factor changes for sudden infant death syndrome after initiation of Back-to-Sleep campaign. Pediatrics 129(4):630–638. https://doi.org/10.1542/peds.2011-1419
- Webster D. W., J. S. Vernick, and M. T. Bulzacchelli. 2009. Effects of state-level firearm seller accountability policies on firearms trafficking. Journal of Urban Health 86(4):525–537. https://doi.org/10.1007/s11524-009-9351-x
- Wong, C. A., F. C. Gachupin, R. C. Holman, M. F. MacDorman, J. E. Cheek, S. Holve, and R. J. Singleton. 2014. American Indian and Alaska Native infant and pediatric mortality, United States, 1999–2009. American
Journal of Public Health 104(Suppl 3): S320–S328. https://doi.org/10.2105/AJPH.2013.301598