Transportation Equity, Health, and Aging: A Novel Approach to Healthy Longevity with Benefits Across the Life Span

One of the most neglected social determinants of health is access to adequate transportation. While housing, education, social inequality (as reflected by the Gini coefficient), and income are widely recognized as important factors of well-being, it is striking that the public health discourse on transportation has overwhelmingly emphasized the negative aspects [1]. These include crashes, injury, mortality, pollution, lack of exercise, and noise. A worthy public health emphasis on active mobility through walking and cycling may have also overshadowed the central role of transportation as driver or passenger in an automobile for the majority of the US population who do not have access to effective public transportation or who have compromised personal mobility. Recent evidence points to the negative consequences of restricted personal vehicle transportation on an individual’s independence, emotional and social well-being, and life expectancy.
The public health bias towards the negative aspects of transportation issues, particularly driving, has led to observed disengagement of physicians and other clinicians in assessing and promoting medical fitness to drive and a failure to consider the transportation needs of patients when accessing health care services [2]. For those clinicians who do address fitness to drive, few supports exist. At the federal level, a standard for fitness to drive exists only for commercial drivers (Federal Motor Carrier Safety Administration 49 CFR Part 391). At the state level, regulations vary regarding medical standards for fitness to drive and requirements for mandatory reporting of impairment. Seventeen states lack medical advisory boards to guide these regulations, and thirteen states lack internal medical units to review medical evaluations and/or need for re-examination of referred drivers [23]. States without such
medical support systems rely on individual physician opinion about fitness to drive and driving impairment despite a general lack of physician knowledge of medical fitness-to-drive guidelines [3].
It is not surprising, therefore, that there has been little dialogue between the field of health care and the main disciplines involved in transportation, such as transportation planners and engineers. However, the beginnings of a rapprochement between the fields has begun, through an emerging focus on the impact of disease and disabilities on transportation mobility and driving safety. This emerging scientific foundation should replace stereotypes, opinions, and anecdotes, and should guide evidence-based transportation counseling for older drivers, young drivers, and those with medical conditions and disabilities.
Ensuring that individuals have equitable access to transportation is vital to ensuring well-being across the life span. Therefore, there is a need for a balanced perspective that can appropriately weigh actual safety risks against the real health consequences of restricting mobility, and a partnership between the fields of health care and transportation could facilitate this balance. More sophisticated, individualized approaches and modeling are becoming available and could allow for “personalized prevention” that optimizes outcomes not only for older adults but also across the life span.
Why We Need to Balance Mobility and Safety
Today’s older drivers are a relatively safe group of drivers [4]. Crash rates for drivers aged 70 and older have declined more rapidly since their peak in 1995 (including crash rates calculated per mile driven) than crash rates for other age groups. In fact, crash rates for current drivers in their 70s are comparable to those of middle-aged drivers aged 35–54 (previously considered the safest group), while rates for those in their 80s are lower than rates for drivers under age 30. The crash rates for older drivers continue to decline with the greatest reductions seen among those 80 and older. This trend in crash rates is reflected across the range of crash severity, from minor property damage to fatal crashes, which is remarkable considering the higher risk of fatality in older drivers due to increased fragility.
These data contradict the common narratives that older drivers are unsafe or that driving privileges need to be restricted based solely on age—narratives that may negatively influence health care professionals when instructing their patients on fitness to drive. However, the emphasis in health care literature and guidelines on driver safety has progressed to an awareness that a lack of transportation access and equity is likely to be a significant threat to well-being and health later in life. The historic misplaced over-emphasis on older driver safety was problematic for many reasons – it inappropriately characterized medical fitness to drive as an issue related to aging, rather than across the life span; it exposed older drivers to unnecessary and harmful screening in many jurisdictions; and was associated with premature driving cessation. Restricting driving without just cause can result in many other real health implications beyond fear of crash or driving error.
An early indicator of the challenge regarding transportation access and equity was revealed in a 2002 report that found that older men and women, ages 70–74, could expect to not be driving and instead be dependent on alternative transportation for the last 7 to 10 years of their lives, respectively [5]. Driving cessation results in depression, premature admission to assisted living facilities, and mortality, [6] and therefore could be extrapolated to this cohort of 70- to 74-year olds in terms of their future quality of life. In addition, increased life-space mobility (a standard measure of mobility and transportation) is positively associated with better health and well-being [7]. This is significant, as not driving a car is associated with restricted life-space mobility for older people: personal car travel provides independence while dependence on others (as a passenger) is associated with life-space restriction [8].
This improved understanding of the importance of transportation in health, the broadening of the health care perspective to include improving both mobility and safety across the life span, and the emergence of an improved evidence base can encourage physicians to engage proactively with medical fitness-to-drive issues among their patients.
New Insights into Driver Behavior Across the Life Span
The research findings described above regarding older drivers demonstrate that transportation access and safety are dynamic fields of research with great impact on quality of life. Further, as with all of medicine, age is a weak indicator of performance. For older drivers, their safe driving occurs in the context of not only an increasing burden of age-related disease and disability but also the natural age-related decline in certain aspects of the nervous system, such as reduced visual acuity and slower reaction times. This finding is counterintuitive, given that safe driving requires excellent planning, situational awareness, appropriate response times and an accurate in-the-moment assessment of personal fitness to drive. These recent findings on age and driving point to the complexity of modeling driving behavior simply based on age. The findings also help advance progress from simplistic models related to disease labels or traditional neuropsychological tests to a more sophisticated understanding of overall driver safety and a nuanced approach that requires the experience of a trained clinician [9].
This recent prioritization of transportation technology and counseling for older drivers can benefit from a synergistic discussion of transportation issues for drivers across the entire life span and for those with disabilities. For example, the authors of this manuscript feel that the emerging literature on crash risk among those with neurodevelopmental conditions (including attention deficit hyperactivity disorder, or ADHD) could be leveraged for older populations, among whom behavior, insight, and prudence are key elements of safe driving that can be managed through medication, with resultant reductions in crash risk [10]. Regarding the quantification of actual driver risk, that of ADHD is most notable. Recent evidence from research with adolescents with ADHD reveals that while the crash risk associated with ADHD is greater than that of their neurotypical peers, it is manageable [11]. The authors
of this manuscript understand that, as with many challenges, safety risk is related more to performance than to a certain age or diagnosis.
Understanding the Changes and Transitions in Transportation Mobility: A Life Span Approach
To support well-being across a person’s life, health care and transportation professionals need to understand and interrogate the changes and transitions in transportation mobility throughout the life span.
When caring for an emerging adult, a key task of that person’s physician is to guide families toward positive development, which includes physical, social, and cognitive development, along with new skill acquisition, leading to eventual autonomy. Transportation mobility (ideally) parallels and enables this development as children emerge from full dependence on parents for mobility, to gradual increases in privileges (with associated modeling, training, and monitoring), to full, independent responsibility for transportation mobility and safety. While there is a health benefit to active mobility—such as walking and cycling—that should be encouraged, in many countries driving remains a key mode of transportation. The challenge during adolescence is ensuring that these novice drivers make safe decisions, manage their passengers, and avoid the hazards of the road while continuing to develop new competencies and capabilities. Unfortunately, in developed and developing countries, traffic injuries remain one of the leading causes of death and acquired disability from infancy through young adulthood. Novice drivers, in particular, have the highest lifetime risk of crashing, largely due to inadequate skills, insufficient experience, and distraction, making a more robust discussion of traffic safety (beyond safety belt use and impaired driving) a critical priority for adolescent health supervision [12].
In addition to inexperience, alcohol and substance abuse increase crash risk. Most medical conditions contribute little to crash risk, especially when compared with risky personality [13]. Three main categories of conditions known to increase crash risk are 1) those that impair attention to the road and judgment (e.g., alcohol and substance abuse, dementia, and neurodevelopmental disorders); 2) physical disabilities, such as hemiplegia, visual impairment, or bradykinesia; and 3) conditions associated with reduced consciousness, such as syncope, epilepsy, and sleep apnea. However, there is reassuring evidence that a systematic, supportive, physician-driven approach to medical fitness to drive is associated with a significant reduction in crashes even among these affected drivers [14]. A patient can present with a combination of these factors—for example, having Parkinson’s disease or a stroke—and individualized clinical assessment is important in addition to supportive guidelines. Even the complex phenomenon of risky behavior may respond to brief training interventions [15].
In the latter phase of life, transportation mobility becomes particularly important as active mobility is reduced and can compromise use of public transportation [16]. One US cross-sectional study confirmed the gendered decline in daily trips and personal driving with advancing age, demonstrating that while older women had fewer daily trips as a driver, they were more likely to travel as a passenger and underwent longer journeys than did older men. There are still many knowledge gaps related to the transition from driving to not driving, with known contributing factors including health, confidence, comfort, and input from family and peers.
A further area of interest is the heterogeneity of transportation needs and abilities with increasing variability within populations in later life: as gerontologists say, we are born copies but die as originals. One overview of existing research suggested segmenting older peoples’ transportation profiles into four generic segments: 1) an active, car-oriented segment; 2) a car-dependent segment, restricted in mobility; 3) a mobile, multimodal segment; and 4) a segment depending on public transportation and other transportation services [17]. Longitudinal studies on aging serve as an important source of data for exploring driving and transportation mobility, though, to date, many such studies have not included substantial data on driving.
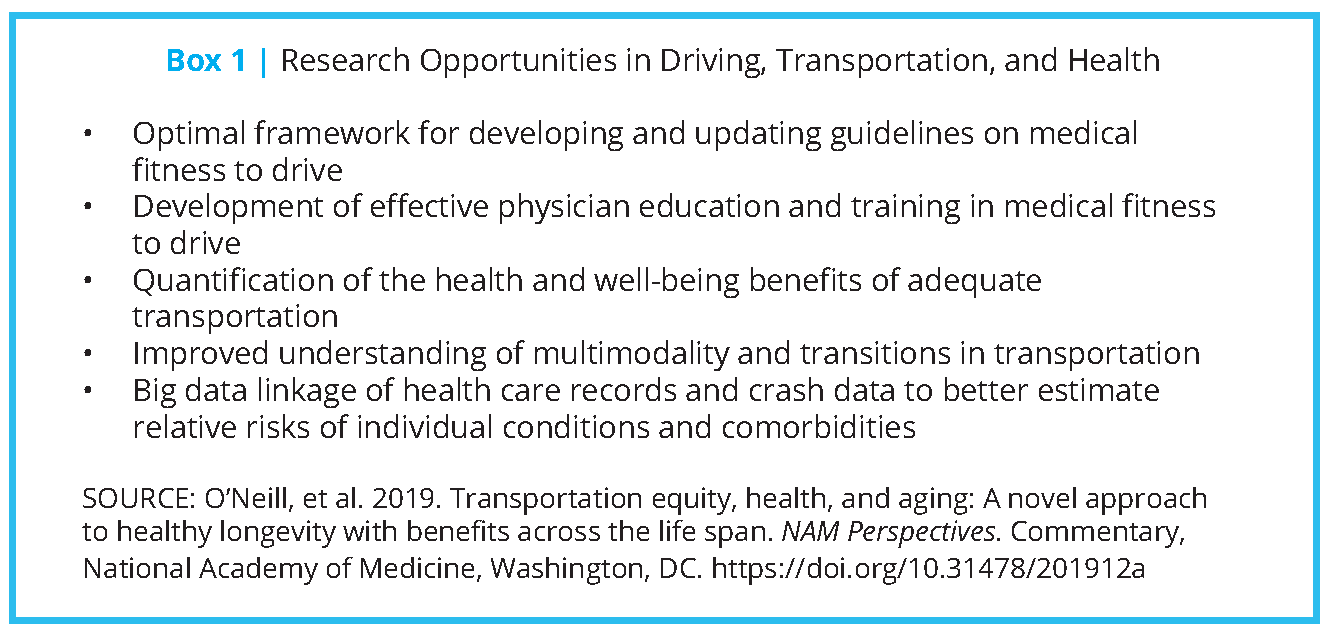
One proposed solution for providing transportation access involves coordinating alternative modes of transportation (e.g., para and public transit), but these options are more realistic in jurisdictions with denser populations, typically found outside the United States. Therefore, the United States largely will need to rely on medical and paraprofessional therapeutic programs to meet the transportation needs of patients with impairment. However, the development of evidence-based and integrated medical fitness to drive policies, procedures, and practice remains underexplored (see Box 1).
Opportunity for Joint Work between Health Care and Transportation Communities
These challenges pose an opportunity for collaborative work between the health care and transportation communities. A helpful starting point is the 1998 conference and update report from the Transportation Research Board (TRB) of the National Academies of Sciences, Engineering, and Medicine on transportation for an aging society [18]. Comprehensive in scope in terms of modalities and indicating an important bidirectional relationship between health care and transportation, the report noted that engagement of health care systems has been underdeveloped.
A key response is the emerging discipline of traffic medicine, the body of knowledge underpinning assessment and management of medical conditions relevant to driving with an emphasis on maintaining mobility as well as safety. Canada, Australia, Ireland, and the United Kingdom have enacted national approaches involving health care professional bodies and licensing authorities charged with developing and updating guidelines, providing models that the United States could adopt. By contrast, in the United States, medical fitness to drive receives scant attention in medical school curricula and postgraduate training, and the regulatory framework for fitness-to-drive guidelines is a patchwork of approaches (or lack thereof) across the states. The result is no collective, evidence-based approach to medical fitness to drive for the medical profession in the United States.
Several initiatives point to the possibilities inherent in a joint approach. Those possibilities include the development of expert panels to advise licensing authorities: one such panel arising from TRB was a salient exemplar of how an evidence-based approach regarding older drivers can help to avoid unnecessary and potentially harmful screening of older drivers [19]. International consortia are also developing to review the quality of existing guidelines on medical fitness to drive against standard criteria [20]. Such work has led to a methodology for developing and updating guidelines for medical fitness to drive for key age-related conditions, such as dementia.
Opportunities to Learn from International Experience
There is also a significant opportunity to learn from international experience and, in particular, from the European Union. The E.U. has enacted Europe-wide regulations on medical fitness to drive for drivers of both personal automobiles and trucks, substantiated by a series of evidence-based reports by expert panels of clinicians who address conditions including diabetes, epilepsy, vision, obstructive sleep apnea, and cardiovascular disease. This effort has fostered fruitful debate and discussion within the medical profession, and the development of traffic medicine.
An exemplar in engaging clinicians on medical fitness to drive is the progress noted in Ireland. Prior to the European Union directives, there was no standard in place within the medical profession or licensing authorities to advise on medical fitness to drive. Prompted by the 2009 directive on diabetes, epilepsy, and vision [21], a National Office for Traffic Medicine (https://www.rcpi. ie/traffic-medicine) was established in 2011 by the National Driver Licensing Authority and the Royal College of Physicians of Ireland.
Aided by a working group representing over 30 medical and health care disciplines, patient advocacy groups, police, the national Department of Motor Vehicles established the Licensing Authority, a program to develop and oversee an annual update of guidelines on medical fitness to drive, promote undergraduate and postgraduate education in traffic medicine, and develop a driving-focused research platform within Irish health care. Innovative elements include a postgraduate certificate in traffic medicine, a public outreach program to increase awareness of medical fitness to drive, and an essay competition for medical students in traffic medicine.
The results of this approach are encouraging and include a very high level of awareness of the guidelines among Irish general practitioners, as well as high levels of confidence in assessing medical fitness to drive following the development of the program.
Developing Awareness and Basic Competencies among Physicians
The success of the Irish collaborative project points to a significant opportunity for US academic leadership in health care and transportation. Two key components of mainstreaming clinician ownership of medical fitness to drive include (i) developing universal awareness and basic competencies among physicians to recognize transportation mobility as a health behavior essential to well-being and (ii) supporting continued safe mobility for all patients, regardless of medical condition or disability, across the life span. Building on the existing literature on older drivers reflects the wisdom inherent in the aphorism of the celebrated gerontologist Professor Bernard Isaacs: “If you design for the old, you include the young: if you design for the young, you exclude the old.” An exploration of supporting medical fitness to drive can benefit drivers with relevant medical conditions and disabilities across the life span.
A 2003 American Medical Association guide on older drivers contained many of the elements necessary for informing medical fitness to drive across all ages and was successful in promoting knowledge and confidence among geriatric medicine trainees. The American Geriatrics Society, in collaboration with the National Highway Traffic Safety Administration, have subsequently maintained the guide, which provides an established evidence base for developing physician guidance involving the entire life span [22]. A further impetus for a life span approach arises from a major study of implementing routine advice on medical fitness to drive in emergency departments in Ontario: this effort resulted in a 45 percent reduction in crash incidence, and the reduction was most notable in younger and middle-aged cohorts [14].
Moving to a Mutually Beneficial Future in Transportation and Health
All stakeholders stand to gain from joint work between the health care and transportation fields with a focus on road safety for all. Transportation mobility and the ensuing well-being will likely be enhanced by a salutogenic and supportive approach to medical fitness to drive. Guidelines and education will support physicians in their interactions with their patients regarding driving decisions, providing them with pragmatic yet increasingly evidence-based recommendations. Research and commercial possibilities will arise from using novel technological approaches for not only assessment but also training, monitoring, and efficacy enhancements to transportation. These solutions may also extend to engaging with alternative transportation modalities and the increasing automation of cars (although they represent progress, they will always require optimization of the human-machine interface, the defining characteristic of traffic medicine).
Join the conversation!
![]() Tweet this! Ensuring equitable access to transportation is vital to ensuring well-being across the life span. This #NAMPerspectives details the need for collaboration between health care & transportation to ensure that aging populations remain independent: https://doi.org/10.31478/201912a
Tweet this! Ensuring equitable access to transportation is vital to ensuring well-being across the life span. This #NAMPerspectives details the need for collaboration between health care & transportation to ensure that aging populations remain independent: https://doi.org/10.31478/201912a
![]() Tweet this! According to the authors of a #NAMPerspectives commentary, adequate transportation is one of the most neglected social determinants of health. Read abt how a partnership between health care & transportation could result in better outcomes for all: https://doi.org/10.31478/201912a
Tweet this! According to the authors of a #NAMPerspectives commentary, adequate transportation is one of the most neglected social determinants of health. Read abt how a partnership between health care & transportation could result in better outcomes for all: https://doi.org/10.31478/201912a
![]() Tweet this! The authors of this #NAMPerspectives argue that restricting driving in an aging population without just cause can result in negative consequences on independence, well-being, and life expectancy. Learn more about supporting transportation options: https://doi.org/10.31478/201912a
Tweet this! The authors of this #NAMPerspectives argue that restricting driving in an aging population without just cause can result in negative consequences on independence, well-being, and life expectancy. Learn more about supporting transportation options: https://doi.org/10.31478/201912a
Download the graphics below and share them on social media!

References
- Litman, T. 2013. Transportation and public health. Annual Review of Public Health 34(1): 217-233. https://doi.org/10.1146/annurev-publhealth-031912-114502
- Shanahan, E. M., R. M. Sladek, and P. Phillips. 2007. Medical aspects of fitness to drive: What do public hospital doctors know and think? Internal Medicine Journal 37(6): 372-376. https://doi.org/10.1111/j.1445-5994.2007.01337.x
- Brooks, J. O., A. Dickerson, M. C. Crisler, W. C. Logan, R. W. Beeco, and J. C. Witte. 2011. Physician knowledge, assessment, and reporting of older driver fitness. Occupational Therapy in Health Care 25(4): 213-224. https://doi.org/10.3109/07380577.2011.607227
- Cicchino, J. B., and A. T. McCartt. 2014. Trends in older driver crash involvement rates and survivability in the United States: An update. Accident Analysis and Prevention 72: 44-54. https://doi.org/10.1016/j.aap.2014.06.011
- Foley, D. J., H. K. Heimovitz, J. M. Guralnik, and D. B. Brock. 2002. Driving life expectancy of persons aged 70 years and older in the United States. American Journal of Public Health 92(8): 1284-1289. https://doi.org/10.2105/ajph.92.8.1284
- Chihuri, S., T. J. Mielenz, C. J. DiMaggio, M. E. Betz, C. DiGuiseppi, V. C. Jones, and G. Li. 2016. Driving Cessation and health outcomes in older adults. Journal of the American Geriatrics Society 64(2): 332-341. https://doi.org/10.1111/jgs.13931
- Rantakokko, M., E. Portegijs, A. Viljanen, S. Iwarsson, and T. Rantanen. 2013. Life-space mobility and quality of life in community-dwelling older people. Journal of the American Geriatrics Society 61(10): 1830-1832. https://doi.org/10.1111/jgs.12473
- Tsuji, T., M. Rantakokko, E. Portegijs, A. Viljanen, and T. Rantanen. 2018. The effect of body mass index, lower extremity performance, and use of a private car on incident life-space restriction: a two-year follow-up study. BMC Geriatrics 18(1): 271. https://doi.org/10.1186/s12877-018-0956-3
- Fuller, R. 2005. Towards a general theory of driver behaviour. Accident Analysis and Prevention 37(3): 461-472. Available at: http://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.458.4050&rep=rep1&type=pdf (accessed September 2, 2020).
- Chang, Z., P. D. Quinn, K. Hur, R. D. Gibbons, A. Sjolander, H. Larsson, and B. M. D’Onofrio. 2017. Association Between medication use for attention-deficit/hyperactivity disorder and risk of motor vehicle crashes. JAMA Psychiatry 74(6): 597-603. https://doi.org/10.1001/jamapsychiatry.2017.0659
- Curry, A. E., K. B. Metzger, M. R. Pfeiff er, M. R. Elliott, F. K. Winston, and T. J. Power. 2017. Motor vehicle crash risk among adolescents and young adults with attention-deficit/hyperactivity disorder. JAMA Pediatrics 171(8): 756-763. https://doi.org/10.1001/jamapediatrics.2017.0910
- Weiss, J. C., J. O’Neil, J. T. Shope, K. G. O’Connor, and R. A. Levin. 2012. Paediatrician knowledge, attitudes, and counselling patterns on teen driving. Injury Prevention 18(1): 10-15. https://doi.org/10.1136/ip.2010.031112
- Charlton, J., S. Koppel, M. Odell, A. Devlin, J. Langford, M. O’Hare, C. Kopinathan, D. Andrea, G. Smith, B. Khodr, J. Edquist, C. Muir, and M. Scully. 2010. Influence of chronic illness on crash involvement of motor vehicle drivers, 2nd ed. Report No. 300. Melbourne, Australia: Monash University, Accident Research Centre.
- Redelmeier, D. A., C. J. Yarnell, D. Thiruchelvam, and R. N. Tibshirani. 2012. Physicians’ warnings for unfit drivers and the risk of trauma from road crashes. The New England Journal of Medicine 367(13): 1228-1236. https://doi.org/10.1056/NEJMsa1114310
- Eensoo, D., M. Paaver, M. Vaht, H. M. Loit, and J. Harro. 2018. Risky driving and the persistent effect of a randomized intervention focusing on impulsivity: The role of the serotonin transporter promoter polymorphism. Accident Analysis and Prevention 113: 19-24. https://doi.org/10.1016/j.aap.2018.01.021
- Hjorthol, R. 2013. Transport resources, mobility and unmet transport needs in old age. Ageing and Society 33: 1190-1211. https://doi.org/10.1017/S0144686X12000517
- Haustein, S., and A. Siren. 2015. Older people’s mobility: Segments, factors, trends. Transport Reviews 35(4): 466-487. https://doi.org/10.1080/01441647.2015.1017867
- Committee for the Safe Mobility of Older People. 2004. Transportation in an aging society: A decade of experience. Washington, DC: Transportation Research Board. Available at: https://trid.trb.org/view/702068 (accessed September 2, 2020).
- Langford, J., K. Braitman, J. Charlton, J. Eberhard, D. O’Neill, L. Staplin, and J. Stutts. 2008. TRB workshop 2007: Licensing authorities’ options for managing older driver safety—Practical advice from the researchers. Traffic Injury Prevention 9(4): 278-281. https://doi.org/10.1080/15389580801895210
- Rapoport, M. J., J. N. Chee, D. B. Carr, F. Molnar, G. Naglie, J. Dow, R. Marottoli, S. Mitchell, M. Tant, N. Herrmann, K. L. Lanctôt, J. P. Taylor, P. C. Donaghy, S. Classen, D. O’Neill. 2018. An international approach to enhancing a national guideline on driving and dementia. Current Psychiatry Reports 20(3): 16. https://doi.org/10.1007/s11920-018-0879-x
- Commission of the European Committees. 2009. Commission directive 2009/112/EC of 25 August 2009 amending council directive 91/439/EEC on driving licences. Available at: https://eur-lex.europa.eu/legal-content/EN/TXT/?qid=1421681203518&uri=CELEX:32009L0112 (accessed November 18, 2019).
- American Geriatrics Society and A. Pomidor. 2016. Clinician’s guide to assessing and counseling older drivers, 3rd ed. Report No. DOT HS 812 228. Washington, DC: National Highway Traffic Safety Administration. Available at: https://www.nhtsa.gov/sites/nhtsa.dot.gov/files/812228_cliniciansguidetoolderdrivers.pdf (accessed September 2, 2020).
- Lococo, K. H., J. Stutts, K. J. Sifrit, and L. Staplin. 2017. Medical review practices for driver licensing, Volume 3: Guidelines and processes in the United States (Report No. DOT HS 812 402). Washington, DC: National Highway Traffic Safety Administration. Available at: https://www.nhtsa.gov/sites/nhtsa.dot.gov/files/documents/812402_medicalreviewdriverlicense.pdf (accessed September 2, 2020).