Stat! An Action Plan for Replacing the Broken System of Recruitment and Retention of Underrepresented Minorities in Medicine

Above: Dr. Kristel Carrington and Dr. Forrester Lee are pictured in the catheterization laboratory at Yale New Haven Hospital. Photo by Brooke Jones. Used by permission of Crystal Emery.
Introduction
The famous quote by African American feminist Audre Lorde—“For the master’s tools will never dismantle the master’s house”—illustrates that true change will not be effected by working within the system [1]. Hence, we need a new approach to diversity within the medical system, because the structure of the current system does not facilitate change. The most recent example of this is the current effort to dismantle affirmative action policies, which will ensure that the recruitment gap widens and that the pipeline of minority students is shut down.
Multiple landmark studies [2,3,4] describe the problem and propose solutions, yet we find ourselves no closer to the goal of diversity within the medical field, specifically among practicing physicians. It is imperative that we look for new and innovative ways to bring about change. In academic medicine, the “master’s house” is the institution of the medical school. To clearly understand that house, one must first understand the foundation upon which it was built. Modern medicine has benefited from and been empowered by the gravest of atrocities committed against African American and brown people, who were considered nothing more than laboratory animals to be poked, prodded, and cut—often without benefit of anesthesia or the dignity of consent. Widely known stories of gynecologist J. Marion Sims, the U.S. Public Health Service Syphilis Study at Tuskegee, and Henrietta Lacks demonstrate that racist acts have served as building blocks for medical institutions.
The master’s house has been framed using the tools of bureaucracy, hierarchy, and hidden curricula. These tools have been designed to reinforce the ideal image of the master’s house, and they define the current metrics for “success” seen in academic medicine. The “master” is any individual, regardless of race or gender, who upholds the racism that pervades the system; the “dismantler” is any individual who actively works to tear those practices down.
Student Recruitment Barriers
Given this image—of a house built with the tools of racism, on a foundation of brutality—we can understand why we must take a new approach to addressing the racial and ethnic disparities that have thus far remained largely unchanged. Racial and ethnic disparities have persisted despite extensive efforts from institutions such as the Association of American Medical Colleges (AAMC) and the National Academy of Medicine, both of which have specific initiatives to support diversity among physicians. Other institutions have created senior leadership positions to support and recruit minority students, but these investments have not directly translated into the appropriate increase of underrepresented minority (URM) medical students and faculty in academic medicine. We must begin to ask how we can do things differently if there is truly a mission for genuine change. A paradigm shift in how recruitment and retention are carried out is necessary if any true change is to be accomplished.
It is now time for institutions and organizations to expand their support for diversity beyond the establishment of positions and programs. Rather, institutional change and cultural climate shift must occur by directly addressing URM barriers to success in medical school admissions, graduation, residency and fellowship attainment, faculty appointment, and leadership positions. We must first clarify the definition of “minority” and identify the challenges that exist within this definition. The AAMC has broadened the definition of URM in medicine to include “those racial and ethnic populations that are underrepresented in the medical profession relative to their numbers in the general population” [5]. Underrepresented racial and ethnic groups in medicine are African Americans, Hispanics, American Indians, Alaska Natives, native Hawaiians, and other Pacific Islanders. The AAMC’s definition also includes intersectionality for male and female individuals of color, with race and gender contributing distinct experiences when confronting privilege and power in academic medicine.
In 1991, Project 3000 by 2000 was developed to bolster the number of first-year URM matriculants [2]. During the course of this project, enrollment for URMs increased by 12 percent, falling significantly short of the target number [6]. Unfortunately, these efforts ended before the goal was met [7].
To increase the numbers of URM medical students, each group must be addressed individually, with specific and targeted interventions to achieve equity. Although there have been some improvements in the number of URMs in medical schools, significant gaps have emerged and continue to widen. Notably, the number of African American men in medical schools is not increasing as fast as the number of African American women. In fact, the AAMC African American Men in Medicine Initiative demonstrated that the number of African American male enrollment in medical schools in 1978 was 542, while enrollment in 2014 was 515 [8]. Additionally, little national emphasis is placed on the needs associated with Native American/American Indian medical students [9].
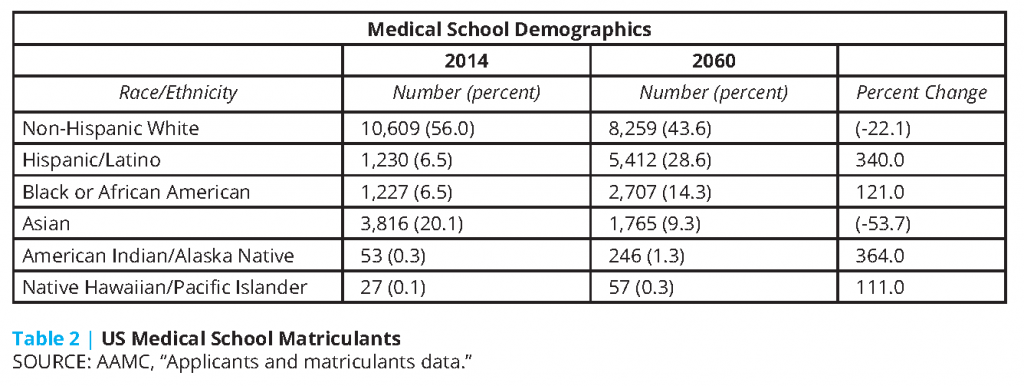
Such disparities have reached a state of emergency, and if these disparities continue, will reach a point of no recovery. These disparities have significant consequences for an increasingly diverse society—with implications not only for social justice in medicine but also for quality health care delivery and patient-centered medicine [10]. There is a need to increase the number of URMs in medical schools. However, due to the legal implications of having quotas, institutions shy away from requiring a certain number of URM medical students. Thus, there is no concrete mechanism for measuring progress and success in URM recruitment. Nevertheless, since the AAMC definition of URM in medicine bases the representation of racial and ethnic groups in medicine on their representation in the general population, we can use current and projected demographics in the United States as the metric to determine what the future composition of medical school matriculants should be.
In 2020, more than half the children in the United States will belong to a racial or ethnic minority group; by 2044, more than 50 percent of all Americans are expected to belong to a racial or ethnic minority group [11]. Clearly, if we are to achieve demographic equity in medicine, we face a staggering challenge.
Based on the AAMC’s Complexities of Physician Supply and Demand [12], there were approximately 787,500 full-time equivalent (FTE) doctors in 2015 and 850,000 projected for 2030. With a constant growth rate, 975,000 FTE doctors would be projected for 2060. If 28.6 percent of those doctors should be Hispanic/Latino (and we assume that no doctor working today will be working in 2060), there needs to be an additional 6,639 Hispanic/Latino FTE doctors per year from now until 2060 to reach that goal. For 14.3 percent of those 975,000 FTE doctors to be African American, 3,320 African American doctors must be matriculated per year from now until 2060.
If corrective measures also attempt to shore up the current national shortage of approximately 100,000 physicians per year, 1,719,474 doctors would need to be practicing in 2060, which translates to 491,769 Hispanic/Latino doctors and 245,884 African American physicians. Assuming that any physicians practicing now will have retired by 2060, that would require an average of 11,709 Hispanic/Latino and 5,854 African American graduates per year from 2018 to 2060.
By 2060, if medical school matriculants represent the racial and ethnic demographics of the general population, to continue that trend, schools would need to matriculate 8,000 URM medical school students yearly in order to continue to reflect the population. Currently, there are just over 2,500 URM medical school matriculants annually [13], a number that falls far short of what projections predict will be necessary to alleviate this issue.
Institutional Barriers
The major barriers to successful recruitment of URM medical students, according to institution admissions committee members, are lower Medical College Admission Test (MCAT) scores, lack of URM faculty, and lack of minority role models. However, no existing data define a specific MCAT score associated with superior patient care. Multiple organizations, including the AAMC and the Sullivan Commission on Diversity in the Healthcare Workforce, have recommended that medical schools reduce their dependence on standardized tests in the admissions process and instead emphasize a holistic review process. While such a process would incorporate traditional metrics of applicant quality, such as grade point average (GPA) and MCAT scores, it would also reward and recognize applicants who possess additional traits valued in a medical trainee, including compassion, empathy, commitment to service, and resiliency. AAMC data show that medical schools that implement holistic review in their applicant selection process demonstrate significant gains in the number of URM matriculants, with no sacrifice in overall class GPA or MCAT score [14].
Although MCAT scores can be directly attributed to student preparation, a lack of URM faculty and role models is a reflection of the institution. Therefore, institutions, by their own assertion, have themselves been a barrier in URM medical student recruitment.
Necessary institutional changes include an aggressive investment in minority faculty. Increasing the number of minority faculty has long been considered an institutional solution to provide both a sense of community and a source of mentorship for URM medical students. Recently, several universities made institutional investments of $50 to $100 million to recruit and retain minority faculty [15,16,17]. This commitment to faculty diversity should serve as a model for all academic medical centers.
While the recruitment of minority faculty is necessary, institutions must also make an investment in developing minority faculty members once they are hired. Turnover for minority medical faculty remains higher than that for white faculty. Minority faculty members are paid less and are less likely to be promoted than their white counterparts [18]. Institutions must make a commitment to the success of junior minority faculty, including provision of resources for scholarly work and dedicated mentorship. Institutions should also provide these faculty protected time away from clinical activities and committee work to ensure academic success and to reduce what has been coined the “minority tax” (i.e. the additional burden placed on minority faculty and staff to support URM students).
Promoting a climate of diversity and inclusion in academic medical centers will also be essential to retaining minority faculty. Several studies have shown that medical students and minority faculty routinely experience discrimination in academic medical schools [19,20]. This discrimination is directly associated with minority physician turnover in academic medicine. Institutions must be more proactive about addressing the climate of their institutions. Interventions include longitudinal bias training, responsive reporting mechanisms, routine surveys of minority physicians concerning diversity and inclusion and the work climate, and dissemination of this data to the whole institution.
Minority-serving institutions Morehouse College, Howard University, Charles R. Drew University of Medicine and Science, and Meharry Medical College are consistently among the top medical schools graduating the highest proportion of primary care doctors, minority physicians, and doctors who work in underserved areas [21]. There is a need for policy changes that will provide greater support to historically African American medical schools, Hispanic-serving institutions, and minority physicians-in-training. But mainstream academia must open more of their doors – the burden cannot fall solely on Historically Black Colleges and Universities. On a national level, this is important not just to bolster physician diversity but also to address the shortage our nation faces of primary care physicians and physicians in underserved areas.
Building a Pipeline for a New Paradigm
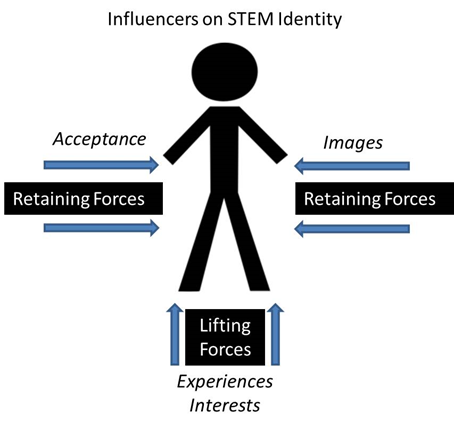
We propose a new model of student recruitment that focuses on student STEM identity formation through early pipeline interventions (see Figure 1). This model recognizes there are “retaining” and “lifting” forces that impact a student’s ultimate academic and professional success.
Figure 1 | Influencers on STEM Identity
We propose a new model of student recruitment that focuses on student STEM identity formation through early pipeline interventions (see Figure 1). This model recognizes there are “retaining” and “lifting” forces that impact a student’s ultimate academic and professional success.
Institutional structures and systems that uphold racism and disparity throughout the URM educational pipeline must be dismantled. As early as middle school, students’ pathways into science and health exploration are forming and their identity formation impacting achievement and career aspiration have begun. One study showed that URM and white middle school students display similar interests in career aspirations in health and medicine, but career aspiration did not necessarily match educational requirements, particularly for Hispanic/Latino students [22]. Data have demonstrated that efforts to address the URM pipeline must begin earlier than high school [23,24,25,26]. Attitudes formed in middle school have a drastic impact on students’ self-efficacy, which in turn impacts students’ academic performance and career aspirations. What is needed now are tools that provide innovative, outside-the-box solutions to prevent “pipeline leakage” or when minority students fall away from pursuing STEM careers—and funding for those solutions.
The lack of minority physicians is not only a crisis in academic medical schools; it is a crisis that originates with the self-efficacy of the elementary or middle school student in the formative years of developing a “medicine identity.” Building a health career or medicine identity has been demonstrated as important for understanding medicine-related outcomes, including engagement, interest, learning, motivation, persistence, and commitment. J. Steinke defines the intersection of the science identities with developmental and identity theories to describe how and when external influencers (media, social, and communal) impact the medical identity for adolescents [27].
The Joint Working Group on Improving Underrepresented Minorities Persistence in Science, Technology, Engineering, and Mathematics (convened by the National Institute of General Medical Sciences and the Howard Hughes Medical Institute) reviews current data and proposes deliberation about why academic pathways leak more for URMs than for white or Asian medical students. Its members suggest expanding efforts to remove institutional barriers and to focus on interventions that “lift” students [28].
Images and experiences influence a student’s acceptance and interest in STEM careers (see Figure 1) and could serve as a tool to promote physician workforce diversity. Positive media images help promote acceptance of STEM fields as attainable career choices for individuals historically marginalized in these fields. Such images are considered retaining forces that keep students interested and on the career pathway. Elevating a professional medical career as a positive image and URM students as part of the “in group” helps to prevent leakage along the medical pipeline that has been observed in marginalized communities. Additionally, engaging in formal and informal medical learning experiences constitute lifting forces that help to promote a student’s matriculation. Taken together, these factors strengthen and influence the development of a medicine identity in students.
The biases affecting a student’s decision to enter medical fields are reinforced by friends, parents, peers, and the media, and these parties have lasting effects on the educational and career paths these students take. Research has identified parents and community members as untapped resources for increasing medical profession motivation in adolescents. Identity theory formation ideals can be applied to this important pipeline problem [17].
Self-Perception
Achievement gaps between URM students and their white peers in college-level STEM classrooms are persistent across many white-majority institutions of higher education. Attempts to reduce this phenomenon of underperformance by increasing nontraditional classroom structure and active learning have been partially successful [28]. A values study addressed “the hypothesis that the achievement gap between white and URM students in an undergraduate biology course has a psychological and emotional component arising from stereotype” [28] threats, which refer to the risk of confirming negative stereotypes about an individual’s racial, ethnic, gender, or cultural group. Specifically, in three iterations of an intensive active-learning college biology course, an intervention was introduced containing values affirmation exercises that counter stereotype threat by reinforcing the student’s feelings of integrity and self-worth. “On average, this exercise reduced the achievement gap between URM and white students who entered the course with the same incoming grade point average” [29]. This outcome suggests that achievement gaps resulting from the URM students’ underperformance could be mitigated by removing psychological and emotional impediments of performance through short psychosocial interventions [29].
In 10 communities around the country hosting Changing the Face of STEM (CFS) initiative projects, (University of New Mexico School of Medicine; University of North Carolina Chapel Hill; Wellesley College, MA; Yale School of Medicine, New Haven, CT; YMCA Atlanta, GA; Training to Reign Ministries, Albemarle, NC; Capitol Region Education Council, Hartford, CT; Charles R. Drew School of Medicine, Los Angeles, CA; Rush Hospital, Chicago, IL; and multiple events in New York City, NY with more than 3,000 college and high school participants, URU The Right to Be targeted participants from groups and demographics typically underrepresented in medicine and engaged them in powerful, meaningful conversations regarding the obstacles both students and professionals face or faced in their academic and career pursuits. The goal of the CFS pipeline model is to effectively break down the internalized racism, sexism, and other “isms” that many young people have unconsciously internalized. Each audience of 300 or more included a variety of stakeholders, including high school and college students, representatives from professional and academic medical institutions, and local community members. For example, the event held in Hartford, CT, brought together over 500 high school girls. The project successfully created powerful, meaningful conversations regarding the obstacles both students and professionals face in their academic and career pursuits. One of the major obstacles mentioned—as a past and present challenge—was the pervasive negative stereotyping of people within marginalized groups regarding their capabilities. Analyses of hundreds of post-event surveys demonstrate that seeing positive images of African American women inspired and encouraged participants to continue on their journeys toward higher education and resulted in positive changes in their belief systems about what is possible as they pursue their post-secondary education and careers.

Above: Dr. Claudia Thomas, the first black woman orthopedic surgeon, with young scholars Kierra Guest, Mikieya Randall, Coletta Morton, Yazmine James, and Kaylah Guest. Photo by Michael Benson. Used by permission of Crystal Emery.
Conclusion
To date, the majority of interventions to increase URM participation in medicine have been undertaken within the existing systems and structures of academic medicine. These efforts have seen only marginal success and do not come close to meeting the needs of future URM physicians in the changing demographics of the United States. To address the urgent need for a diverse physician workforce, we must use innovative tools. We believe an approach that integrates medical identity and medical experiences through media allow URMs to identify early with the field of medicine and to see the medical profession as a legitimate professional option. Medicine identity and medical experiences through media helps to create a personal medicine identity which will result in a higher likelihood of retention within the medical pipeline.
However, focusing solely on the student is not sufficient. Institutions must create environments that are more inclusive of URM students and faculty. Individuals representing these institutions must also make personal changes and use their privilege and voice to speak out against localized issues of inequity. Only then will we have the opportunity to dismantle the systems within academic medicine that have upheld inequity, creating a chance to develop a new paradigm of equity using new tools. You have the power to create a new paradigm. The real question is—are you willing to take the courageous actions required?
Join the conversation!
![]() Tweet this! We need more diversity in medicine. Our newest #NAMPerspectives describes how we can get there: https://doi.org/10.31478/201809a
Tweet this! We need more diversity in medicine. Our newest #NAMPerspectives describes how we can get there: https://doi.org/10.31478/201809a
![]() Tweet this! Institutional changes, like eliminating standardized testing scores and conducting intentional recruitment of minority faculty to serve as role models, can make significant change in increasing diversity in the field of medicine: https://doi.org/10.31478/201809a #NAMPerspectives
Tweet this! Institutional changes, like eliminating standardized testing scores and conducting intentional recruitment of minority faculty to serve as role models, can make significant change in increasing diversity in the field of medicine: https://doi.org/10.31478/201809a #NAMPerspectives
![]() Tweet this! Exposing underrepresented minority youth to positive experiences in medicine early in their lives can significantly change their career trajectories and aspirations. Our newest #NAMPerspectives describes how to bolster a diverse pipeline: https://doi.org/10.31478/201809a
Tweet this! Exposing underrepresented minority youth to positive experiences in medicine early in their lives can significantly change their career trajectories and aspirations. Our newest #NAMPerspectives describes how to bolster a diverse pipeline: https://doi.org/10.31478/201809a
Download the graphics below and share them on social media!
References
- Lorde, A. 2007. The master’s tools will never dismantle the master’s house. In Sister outsider: Essays and speeches, reprint edition. Berkeley, CA: Crossing Press. Pp. 110-114.
- Nickens, H. W., T. P. Ready, and R. G. Petersdorf. 1994. Project 3000 by 2000 — Racial and ethnic diversity in U.S. medical schools. New England Journal of Medicine 331(7):472-476. https://doi.org/10.1056/NEJM199408183310712
- Sullivan, L. W. 2004. Missing persons: Minorities in the health professions, a report of the Sullivan Commission on Diversity in the Healthcare Workforce. Durham, NC: Duke University School of Medicine. Available at: http://health-equity.lib.umd.edu/40 (accessed July 15, 2018).
- Cohen, J. J., B. A. Gabriel, and C. Terrell. 2002. The case for diversity in the health care workforce. Health Affairs 21(5):90-102. https://doi.org/10.1377/hlthaff.21.5.90
- Association of American Medical Colleges (AAMC). n.d. Underrepresented in medicine definition. Available at: https://www.aamc.org/initiatives/urm (accessed April 17, 2018).
- Terrell, C., and J. Beaudreau. 2003. 3000 by 2000 and beyond: Next steps for promoting diversity in the health professions. Journal of Dental Education 67(9):1048-1052. https://doi.org/10.1002/j.0022-0337.2003.67.9.tb03691.x
- Ready, T. 2001. The impact of affirmative action on medical education and the nation’s health. Cambridge, MA: Harvard Education Publishing Group. Pp. 205-219.
- Association of American Medical Colleges. 2015. Altering the course: Black males in medicine. Washington, DC. Available at: https://members.aamc.org/eweb/upload/Altering%20the%20Course%20-%20Black%20Males%20in%20Medicine%20AAMC.pdf (accessed July 15, 2018).
- Sanchez, J. P., N. Poll-Hunter, N. Stern, A. N. Garcia, and C. Brewster. 2016. Balancing two cultures: American Indian/Alaskan Native medical students’ perceptions of academic medicine careers. Journal of Community Health 41(4):870-80. https://doi.org/10.1007/s10900-016-0166-x
- Marrast, L. M., L. Zallman, S. Woolhandler, D. H. Bor, and D. McCormick. 2014. Minority physicians’ role in the care of the underserved patients: Diversifying the physician workforce may be key in addressing health disparities. JAMA 174(2):289-291. https://doi.org/10.1001/jamainternmed.2013.12756
- S. L., and J. M. Ortman. 2015. Projections of the size and composition of the U.S. population: 2014 to 2060. Washington, DC: US Census Bureau. Available at: https://www.census.gov/content/dam/Census/library/publications/2015/demo/p25-1143.pdf. (accessed August 29, 2018).
- Association of American Medical Colleges. 2018. Complexities of physician supply and demand projections. Washington, DC. Available at: https://www.aamc.org/data/workforce (accessed July 15, 2018).
- Association of American Medical Colleges. N.d. Applicants and matriculants data. Available at: https://www.aamc.org/data/facts/applicantmatriculant (accessed July 15, 2018).
- Urban Universities for Health. 2014. Holistic admissions in the health professions: Finding from a national survey. Washington, DC.
- Eversley, M. 2017. Columbia makes $100 million investment in diversity. Diverse Issues in Higher Education, December 6. Available at: http://diverseeducation.com/article/105976 (accessed February 15, 2018).
- Friedersdorf, C. 2015. Brown University’s $100 million inclusivity plan. The Atlantic, November 24. Available at: https://www.theatlantic.com/politics/archive/2015/11/brown-universitys-100-million-plan-to-be-more-inclusive/416886 (accessed February 15, 2018).
- Flaherty, C. 2017. Yale gives update on $50M faculty diversity initiative. Inside Higher Ed, October 13. Available at: https://www.insidehighered.com/quicktakes/2017/10/13/yale-gives-update-50m-faculty-diversity-initiative (accessed February 15, 2018).
- Nunez-Smith, M., M. M. Ciarleglio, T. Sandoval-Schaefer, J. Elumn, L. Castillo-Page, P. Peduzzi, and E. H. Bradley. 2012. Institutional variation in the promotion of racial/ethnic minority faculty at US medical schools. American Journal of Public Health 102:852-858. https://doi.org/10.2105/AJPH.2011.300552
- Nunez-Smith, M., N. Pilgrim, M. Wynia, M. M. Desai, C. Bright, H. M. Krumholz, and E. H. Bradley. 2009. Health care workplace discrimination and physician turnover. Journal of the National Medical Association 101:1274-1282. https://doi.org/10.1016/s0027-9684(15)31139-1
- Baldwin, D. C., R. Daugherty, and E. J. Eckenfels. 1991. Student perceptions of mistreatment and harassment during medical school: A survey of ten United States schools. Western Journal of Medicine 155:140-145. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1002944/ (accessed September 1, 2020).
- Mullan, F. 2017. Social mission in health professions education: Beyond Flexner. JAMA 318:122-123. https://doi.org/10.1001/jama.2017.7286
- Perry, B. L., E. Martinez, E. Morris, T. C. Link, and C. Leukefeld. 2016. Misalignment of career and educational aspirations in middle school: Differences across race, ethnicity and socioeconomic status. Social Science 5(35). https://doi.org/10.3390/socsci5030035
- Falco, L. D. 2017. The school counselor and STEM career development. Journal of Career Development 44(4):359-374. https://doi.org/10.1177/0894845316656445
- Christensen, R., and G. Knezek. 2017. Relationship of middle school student STEM interest to career intent. Journal of Education in Science, Environment and Health 3(1):1-13. Available at: https://files.eric.ed.gov/fulltext/EJ1125793.pdf (accessed September 1, 2020).
- Aschbacher, P. R., M. Ing, and S. M. Tsai. 2014. Is science me? Exploring middle school students’ STE-M career aspirations. Journal of Science Education Technology 23:735-743. https://doi.org/10.1007/s10956-014-9504-x
- Tang, M., W. Pan, and M. D. Newmeyer. 2008. Factors influencing high school students’ career aspirations. Professional School Counseling 11(5):285-295. https://doi.org/10.1177/2156759X0801100502
- Steinke, J. 2017. Adolescent girls’ STEM identity formation and media images of STEM professionals: Considering the influence of contextual cues. Frontiers in Psychology 8:716. https://doi.org/10.3389/fpsyg.2017.00716
- Estrada, M., M. Burnett, A. G. Campbell, P. B. Campbell, W. F. Denetclaw, C. G. Gutiérrez, S. Hurtado, G. H. John, J. Matsui, R. McGee, C. M. Okpodu, T. J. Robinson, M. F. Summers, M. Werner-Washburne, and M. Zavala. 2016. Improving underrepresented minority student persistence in STEM. CBE—Life Sciences Education 15(3). https://doi.org/10.1187/cbe.16-01-0038
- Jordt, H., S. L. Eddy, R. Brazil, I. Lau, C. Mann, S. E. Brownell, K. King, and S. Freeman. 2017. Values affirmation intervention reduces achievement gap between underrepresented minority and white students in introductory biology classes. CBE—Life Sciences Education 16(3). https://doi.org/10.1187/cbe.16-12-0351