Referral System Collaboration Between Public Health and Medical Systems: A Population Health Case Report
Social determinants of health, a short phrase that captures a broad array of issues, are some of the key reasons why health care reform alone will not eliminate health disparities in the United States. Social problems, such as food security, housing, and employment, account for 15 percent of premature deaths in the United States (Schroeder, 2007) and disproportionately worsen the health of socially disadvantaged groups (Marmot, 2005). The acknowledgment that social conditions affect health has helped crystalize a movement that impels public health and medical systems to inquire about and assist patients with their social problems (Commission on Social Determinants of Health, 2008). By embracing this broader role, public health and health care systems have the potential to reduce disparities and increase equity among diverse populations, and ultimately improve the health of all individuals and society as a whole.
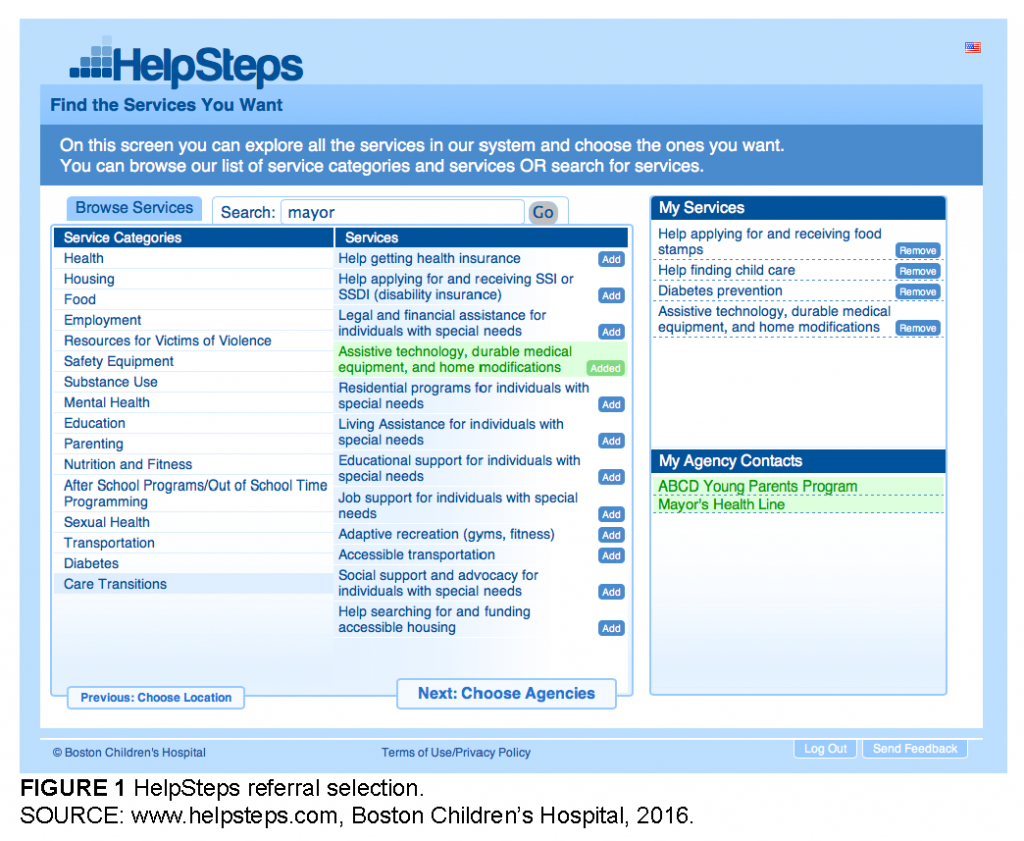
This paper will discuss collaboration between Boston Children’s Hospital and the Boston Public Health Commission to develop, evaluate, and deploy HelpSteps.com, a web-based screening and referral system for social problems that connects individuals and families to social services (see Figure 1 for a view of the HelpSteps interface). The paper will appraise the benefits of multidisciplinary collaboration and discuss the challenges of sustained implementation within the current health care environment. The future goals and the potential for radically meeting the social needs of families are discussed.
Background
Multiple barriers prevent public health officials and health care providers from asking families about their social problems, including lack of knowledge about social issues, discomfort with discussing these problems, and uncertainty about how to refer them to appropriate services. Resource listings quickly become out of date and are difficult to access.
To overcome these challenges, The Online Advocate, now called HelpSteps, was conceived in 2003 as a tool to help screen families for health-related social problems and connect them to local organizations best suited to meet those needs. Research confirmed that clinics screened their patients for social problems at very low rates and provided less than half of desired referrals, but the research also indicated that patients strongly desired assistance with their social needs (Fleegler et al., 2007).
The next iteration of HelpSteps expanded the screening questionnaire and developed a comprehensive referral database of social services throughout Boston. In brief, the system uses an in-depth questionnaire to evaluate families’ social needs, suggests services that may help them, allows users to read detailed descriptions of services located near their residence or other desired location, and helps users select the referrals that meet their needs (see Box 1).
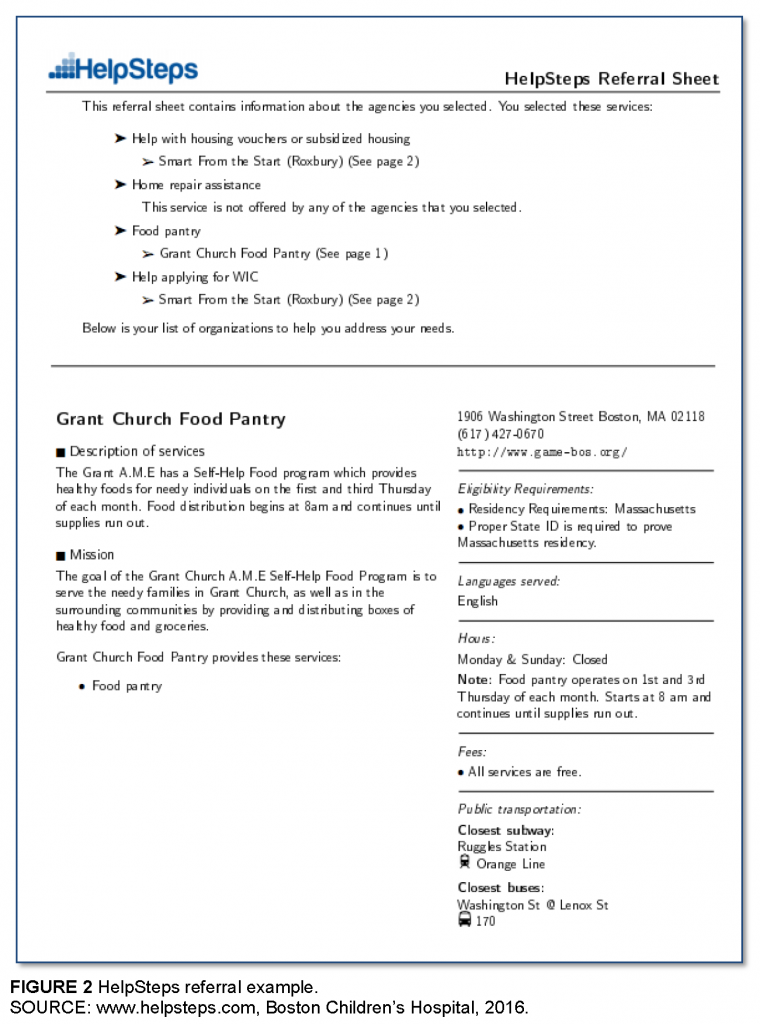
Users can skip the screening evaluation and directly select referrals as desired. Once selected, HelpSteps prints out referral sheets that the user can keep for reference; the system can send the key referral information via email and SMS text as well. The referral sheets include a brief description of the program, contact information, a list of all services provided, eligibility, fees (if any), languages served, and public transportation options (see Figure 2 for an example).
Compiling available resources involved hundreds of hours of accessing a variety of listings including binders of printed information, Rolodexes, Excel files, static websites, private databases, as well as interviewing social workers, resource specialists, and other professionals. In doing so, it became clear that there was limited collaboration among community agencies, many of which duplicated efforts by maintaining independent resource lists that were often incomplete and quickly out of date.
HelpSteps was initially implemented in clinical settings. During an 18-month period, HelpSteps was incorporated into adolescent primary care visits during an intervention study within the Boston Children’s Hospital Adolescent/Young Adult Clinic. Four hundred and one patients, 15 to 25 years old, completed HelpSteps followed by a brief meeting with the clinic resource specialist. Major findings included:
- Prevalence of social problems: 76 percent of youth screened positive for at least one major social problem; 47 percent experienced at least two or more social problems (Hassan et al., 2013).
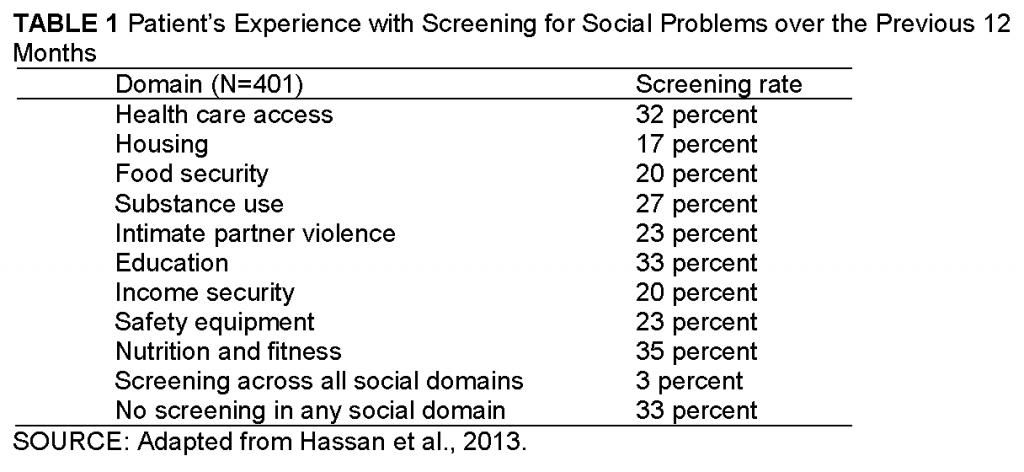
- Baseline screening rates: Screening for health-related social problems by any health care provider over the prior year averaged 25 percent across social domains (Table 1) (Hassan et al., 2013).
- Referral need: 78 percent self-selected at least one referral for an unmet social need; overall more than 1,500 referrals were selected (Hassan et al., 2015).
- Resolution of social problems: Nearly half of patients who selected referral services successfully addressed their priority problem (Hassan et al., 2015).
- Screening appropriateness: 84 percent found it acceptable to screen and help with social problems as part of the medical visit (Hassan et al., 2013; Wylie et al., 2012).
In the young adult clinic, the relationship of social problems and health outcomes was strong. The presence of even one social problem was associated with diminished self-rated health (β = 0.68 points on a 5-point scale (Kreatsoulas et al., 2015). Among patients with asthma, the greater the burden of social problems the poorer their asthma control (Hassan et al., 2011).
In 2011, HelpSteps was implemented in the Boston Children’s Hospital Primary Care Center both to help families and to examine the associations between families’ health-related social problems and childhood obesity. Three hundred forty families used HelpSteps and were followed over a year. Consistent with findings from other sites, the majority of families experienced at least one major social problem over the past 12 months. Half of families reported household problems, and 31 percent reported household food insecurity. Over the previous 12 months, 18 percent of parents reported an inability to fill necessary prescriptions and 10 percent reported physical or verbal abuse by an intimate partner.
Cumulative burden of health-related social problems was associated with increasing body mass index (BMI) among 3- to 10-year-old children. Child BMI z-scores increased by 0.17 (95 percent confidence interval [CI] 0.09–0.26) for each additional social problem. After adjustment for age, race/ethnicity, and sex, parents with four or more health-related social problems were more than twice as likely to have a clinically obese 3- to 10-year-old child than parents with no social problems (adjusted odds ratio [AOR] 2.4, 95 percent CI 1.3–4.5) (Bottino et al., 2013).
Household food insecurity was independently associated with childhood obesity among families. After adjustment, families with household food insecurity were 2.6 times more likely to have a clinically obese 3- to 10-year-old child (AOR 2.6, 95 percent CI 1.5–4.4).
Public Health Collaboration
In the late 1990s, the Boston Public Health Commission (BPHC) and the Action for Boston Community Development (ABCD, Inc.) had collaborated to develop an online resource database of social services, which had stalled by 2003. At this time, HelpSteps committed to reviving and enhancing the referral system, and Gerry Thomas, Director of Community Initiatives at BPHC, took the bold step of providing HelpSteps access to the entire original database and partnering with Boston Children’s Hospital to develop one central site to screen and provide families referrals to social services in the greater Boston area.
The Mayor’s Health Line (MHL), a program of the Boston Public Health Commission, is Boston’s health and social service referral line. MHL provides free, confidential, and multilingual services to Boston’s residents. MHL staff helps people over the phone and in person, offering walk-in services and hosting workshops and outreach events throughout the city. MHL assists over 10,000 individuals and families annually. Individuals and families served by the MHL reflect the ethnic, racial, cultural, and economic diversity of the city.
MHL staff are certified navigators, trained by the MA Health Connector to help residents shop and apply for health care insurance through the state marketplace. As Boston’s health and social service referral line, MHL fields calls from people who need both health and social services. As navigators and SHINE (Serving the Health Insurance Needs of Everyone) counselors, MHL has a consistent stream of residents looking to apply for MassHealth, Medicare, and subsidized and unsubsidized insurance plans through the state marketplace. MHL staff screen all applicants to determine if they require or want health or social services in addition to health insurance, thereby providing wraparound services. MHL staff use HelpSteps to connect clients who require additional services to a robust list of social and health services that are tailored to meet the clients’ unique health needs.
Beyond MHL, the Boston Public Health Commission has several programs, including violence prevention, homeless services, and asthma management, that provide direct client services. In an effort to ensure that clients across BPHC programs are consistently connected to appropriate health and social services, the commission’s leadership endorses and promotes HelpSteps as the database for health and social services. To standardize the use of HelpSteps across all commission programs, new hire orientation now includes HelpSteps. MHL provides additional training to BPHC employees and promotes HelpSteps to community-based organizations including 10 to 15 in-person information sessions annually, reaching over 150 health and social service providers in the community.
To ensure the quality and accuracy of the 1,700 agencies included in the database, members of the MHL staff continually update the HelpSteps database. A powerful product of this collaboration allows MHL to focus on maintaining the integrity of the referral database while the HelpSteps team focuses on software development and enhancement.
Annual access of HelpSteps has grown nearly four-fold from 2011 to 2015, from a total of 1,104 users to 4,167. Among these users, over 12,000 services are selected annually, with the greatest numbers of resources requested being health, housing, food, and employment resources (see Table 2). Over a 6-month period at BPHC, 2,197 individuals were screened and provided referral assistance.
Boston Public Health Commission expanded the use of HelpSteps through Centers for Disease Control and Prevention (CDC) REACH (Racial and Ethnic Approaches to Community Health) funding. Boston REACH: Partners in Health & Housing, is a 3-year BPHC initiative (2014–2017) to improve the health of Boston residents living in Boston Housing Authority (BHA) developments and BHAAdministered Rental Assisted/Section 8 housing. Boston REACH’s goal is to improve access to and consumption of healthy food and beverages, increase linkages to community health care resources, and enhance the quality of and access to smoke-free housing.
REACH grant activities include bringing HelpSteps directly to housing residents as a tool to link them to health care resources. Through the REACH grant, BPHC recruited resident health advocates (RHA) and youth health ambassadors (YHA), residents of the public housing, who are hired to help achieve the grant’s objectives: connecting public housing residents to community health care resources. MHL staff trained RHAs and YHAs in HelpSteps. Through the grant, the RHAs and YHAs were given tablets to access HelpSteps as a resource. To connect with residents, RHAs and YHAs attend public housing leadership meetings and resource fairs. They bring their tablets to the leadership meetings and resource fairs, and use HelpSteps to find health and social services for residents.
Project REACH plans to introduce HelpSteps to navigators, community health workers, and other nonlicensed health personnel. The plan is to integrate HelpSteps into participating community health centers operating procedures as a way to link patients to much-needed health and social services.
Discussion
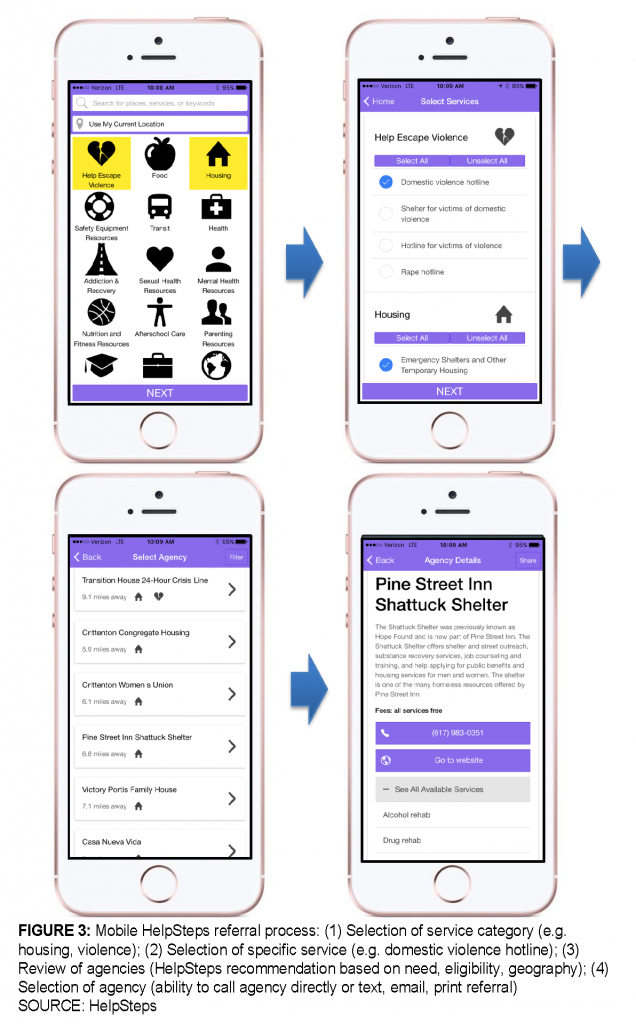
Sustained implementation of screening and referral for social needs is difficult to achieve. Despite users’ positive feedback, case managers frequently resort to either institutional knowledge or other established mechanisms for referring families to social services, rather than using HelpSteps. Part of this reluctance includes limited access to computers and the challenge of changing old habits. A new mobile interface (see Figure 3) will allow individuals to use smartphones and tablets to readily access the system. BPHC will field test the mobile system with clients across the city as part of the rollout process.
A major part of HelpSteps’ value is in the accuracy, quality, and quantity of information in the tool’s database. The annual updating process is labor intensive: each of the 1,700 agencies is called, and it can take 5 to 10 minutes to update the agency’s information; new agencies take 10 to 15 minutes to be entered into the system. A constant struggle is to find a process that is efficient and yet protects the data’s integrity. New automated reminders encourage social service agencies to update their own information, while dedicated interns at BPHC and Boston Children’s Hospital work to maintain the system.
One promising model for community expansion involves developing formal partnerships with public health organizations that want to provide access to HelpSteps to their clients. This approach proved successful when HelpSteps was included in the grant application and program work plans for the Healthier Roxbury Coalition (Healthier Roxbury Coalition, 2015). The coalition sought to improve the well-being of community members living with Type 2 diabetes by linking hospitals, health centers, and community programs. As part of this collaboration, HelpSteps added a new service category—diabetes—that includes multiple community resources focused on diabetes care, thus enhancing and streamlining the referral process.
The best models for deploying within the health care system involve direct partnership and a commitment on behalf of a clinic to provide assistance to their patients. As an example, an internal medicine and pediatric transition medicine program has recently partnered with HelpSteps (Sharma et al., 2014). Through their efforts, over 100 resources related to young adults with special health care needs were added to HelpSteps. Under the direction of their director they are mapping out the best approach to rolling out HelpSteps to all of the patients within their clinic. BPHC, in addition to playing a founding and maintenance role, also provides support in applying for grants in collaboration with organizations such as the Transitions Program, bringing the dimension of powerful partnership to grant applications.
Investing in social interventions makes sense. By helping families with social needs, medical and public health systems can influence both short- and long-term health outcomes, improve patient satisfaction, and reduce health care costs. Early data suggest that patients who receive help with their social problems have improved asthma management, better nutrition, and are better able to care for themselves. What changes are required to truly expand both screening and assisting families with their social problems?
- Implement payment models that provide financial incentives to health care systems and medical providers to incorporate social interventions into their care model.
- Integrate traditional medical care with other supports. Maximize and expand existing resources such as on-site social workers and/or resource specialists. Expand resource specialists’ scope of care to broadly assess social determinants of health and link families to community organizations that provide wraparound services to address a broad range of needs.
- Develop and maintain high-quality, up-to-date databases of local resources that can be shared among organizations. HelpSteps has recently connected with Open Referrals, a Code for America initiative, to establish a national model for this type of care (Code for America, 2015).
- Create data collection and monitoring systems that can track referral usage, especially to ensure that high-risk patients follow up on referrals to community resources.
Financial and moral imperatives compel health care providers and public health systems to work together to address these challenges. Improving health outcomes while at the same time reducing expenditures requires directly addressing the social determinants of health. Sharing successes and challenges in addressing social determinants, building sustainable partnerships, and investing in feasible, innovative, and generalizable solutions that connect people with social service resources are necessary steps towards helping everyone lead healthy, productive lives.
Download the graphic below and share it on social media!
References
- Boston Children’s Hospital. 2016. HelpSteps. Available at: http://www.helpsteps.com (accessed March 10, 2016).
- Bottino, C., E. T. Rhodes, E. Manz-Reisinger, G. Marmon, A. Pikcilingis, K. T. Haagen, L. Tsopelas, J. Mudd, L. M. Wenren, A. T. Geanacopoulos, C. Kreatsolulas, J. Cox, and E. W. Fleegler. 2013. Cumulative burden of health-related social problems associated with increasing body mass index among 3-10 year olds. Presented at the Annual Meeting of the Pediatric Academic Societies. Washington, D.C.
- Code for America. 2015. Open referral. Available at: https://www.codeforamerica.org/our-work/dataformats/openreferral/ (accessed February 18, 2016).
- Commission on Social Determinants of Health. 2008. Closing the gap in a generation: Health equity through action on the social determinants of health. Final Report of the Commission on Social Determinants of Health. Geneva, Switzerland: World Health Organization. Available at: https://www.who.int/social_determinants/final_report/csdh_finalreport_2008.pdf (accessed July 20, 2020).
- Fleegler, E. W., T. A. Lieu, P. H. Wise, and S. Muret-Wagstaff. 2007. Families’ health-related social problems and missed referral opportunities. Pediatrics 119(6):1332-1341. https://doi.org/10.1542/peds.2006-1505
- Hassan, A., E. A. Blood, A. Pikcilingis, E. G. Krull, L. McNickles, G. Marmon, S. Wylie, E. R. Woods, and E. W. Fleegler. 2013. Youths’ health-related social problems: Concerns often overlooked during the medical visit. Journal of Adolescent Health 53(2):265-271. https://doi.org/10.1016/j.jadohealth.2013.02.024
- Hassan, A., E. A. Scherer, A. Pikcilingis, E. Krull, L. McNickles, G. Marmon, E. R. Woods, and E. W. Fleegler. 2015. Improving social determinants of health: Effectiveness of a web-based intervention. American Journal of Preventive Medicine 49(6):822-831. https://doi.org/10.1016/j.amepre.2015.04.023
- Hassan, A., A. Pikcilingis, G. Marmon, S. Wylie, E. R. Woods, and E. W. Fleegler. 2011. Association of health-related social problems and asthma in adolescents. Presented at the Annual Meeting of the Pediatric Academic Societies. Denver, CO.
- Healthier Roxbury Coalition. 2015. Roxbury rising against diabetes: Building a healthy community. In Healthier Roxbury Resource Guide. Boston, MA: Healthier Roxbury Coalition.
- Kreatsoulas, C., A. Hassan, S. V. Subramanian, and E. W. Fleegler. 2015. Social disparities among youth and the impact on their health. Adolescent Health, Medicine and Therapeutics 6:37-45. https://doi.org/10.2147/AHMT.S64903
- Marmot, M. 2005. Social determinants of health inequalities. Lancet 365(9464):1099-1104. Available at: https://www.who.int/social_determinants/strategy/Marmot-Social%20determinants%20of%20health%20inqualities.pdf (accessed July 20, 2020).
- Schroeder, S. A. 2007. Shattuck lecture. We can do better–Improving the health of the American people. New England Journal of Medicine 357(12):1221-1228. https://doi.org/10.1056/NEJMsa073350
- Sharma, N., K. O’Hare, R. C. Antonelli, and G. S. Sawicki. 2014. Transition care: Future directions in education, health policy, and outcomes research. Academic Pediatrics 14(2):120-127. https://doi.org/10.1016/j.acap.2013.11.007
- Wylie, S. A., A. Hassan, E. G. Krull, A. B. Pikcilingis, H. L. Corliss, E. R. Woods, and E. W. Fleegler. 2012. Assessing and referring adolescents’ health-related social problems: Qualitative evaluation of a novel web-based approach. Journal of Telemedicine and Telecare 18(7):392-398. https://doi.org/10.1258/jtt.2012.120214