Why We Need Climate, Health, and Equity in All Policies
“For public health, climate change is the defining issue for the 21st century.” Margaret Chan, World Health Organization
“Social injustice is killing people on a grand scale.” WHO Commission on the Social Determinants of Health
Climate change, health equity, social and environmental justice, sustainability: These are each hugely important and complex issues in their own right. But we cannot afford to address them separately: The root causes are the same, the stakes too high, the need for action too urgent, and the opportunities for synergy too great.
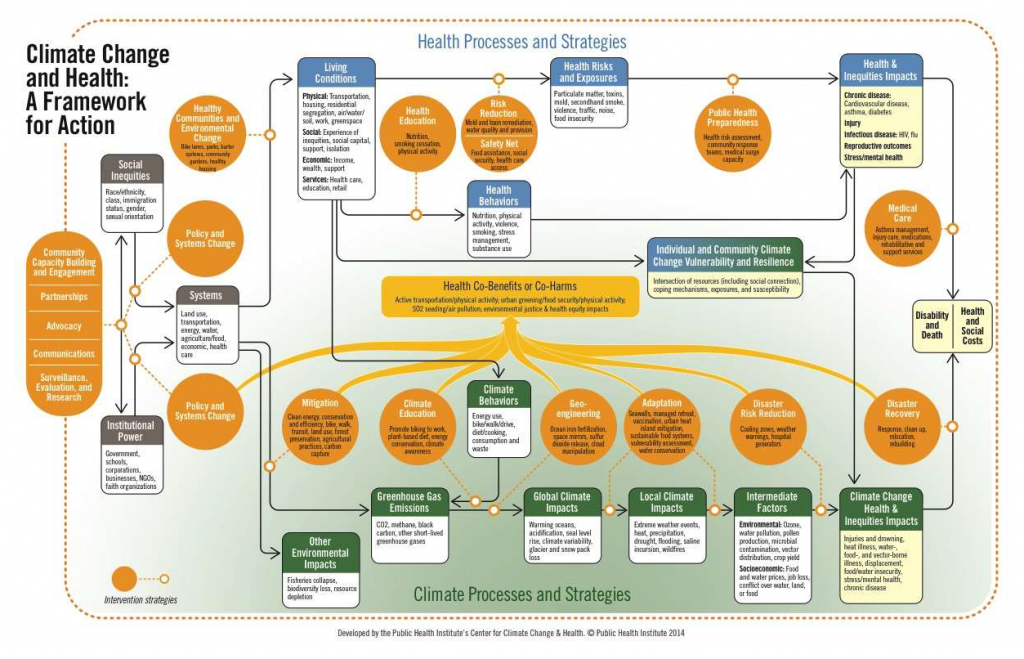
People in the United States and around the world are already experiencing the effects of climate change. These effects will increase as the global and local impacts of climate change worsen. At the same time, increasing levels of social inequality heighten persistent and unacceptable health inequities. Climate change will even further exacerbate health inequities. These processes are inextricably linked, as shown in the figure below.
The social, physical, economic, and services environments in which we live, learn, work, and play are the key determinants of health behaviors and health outcomes. Health inequities result from the “systematic and unjust distribution of social determinants or conditions that support health.”
Powerful institutions (e.g., government, corporations, schools) are largely responsible for constructing systems (for instance, transportation, land use, food and agriculture, energy, economic) that shape living conditions. These institutions both influence and are influenced by social inequities, such as class and race. The same systems that determine living conditions are also the key contributors to climate change, and to other extensive ecosystems damage (e.g., soil degradation, air pollution, water contamination, ocean dead zones).
The impacts of climate change on health and health inequities are moderated by individual and community vulnerability and resilience: two critical components of climate vulnerability are pre-existing health status and living conditions. Health inequities and the unhealthy living conditions that produce them thus serve to increase climate vulnerability. Conversely, interventions that address the social determinants of health, improve population health status, and reduce health inequities are vital strategies to increase climate resilience.
Just as there is a broad spectrum of public health interventions to prevent adverse health outcomes and reduce health inequities, there is a wide spectrum of interventions to address climate change. Many climate actions bring significant health co-benefits and promote equity, but some may have significant negative health consequences and increase health inequities. Thoughtful implementation of actions to reduce greenhouse gas emissions and adapt to climate impacts will maximize health and equity co-benefits and minimize co-harms. Just as upstream policy, systems, and environmental change strategies are most effective in improving population health, so too upstream interventions are most effective in addressing climate change. Because the root causes of climate change, ecosystems destruction, and health inequities are largely the same, interventions that act on the shared systemic causes will bring about the most significant benefits for human health and the environment.
The world’s scientists and governments have agreed that the risks of catastrophic climate change rise significantly if global temperatures increase more than 2 degrees Celsius above pre-industrial levels. We have used up about two-thirds of the IPCC established “carbon budget.” If we do not significantly reduce emissions of climate-altering pollutants very quickly, it is increasingly likely that future generations will experience catastrophic climate change, for which adaptation and disaster response will be insufficient to prevent profound human and ecological impacts. Each year of delay will increase risk and cost. As Jim Kim, President of the World Bank, said, “Climate change threatens our fragile existence on this planet.” Bold, transformative systems and socio-cultural-economic changes are urgently required.
This cannot happen without building movements that both shift social norms and gain the political power to require that the decisions of powerful institutions address health, equity, and sustainability. That is a prerequisite to protect people here and around the world from devastating climate consequences.
Public health can play an important role in this transformation if its leaders are willing to acknowledge the urgency of the problem and the transformational change required to address it. Public health can define risk, provide credible risk communication to the public and policymakers, and promote interventions with health and equity co-benefits. Many public health organizations work in the disadvantaged and impacted communities most vulnerable to climate change: This provides an opportunity to engage and partner with residents and mobilize communities and resources to fight climate change.
But public health cannot succeed alone. We must join together with those fighting for social and environmental justice and for environmental and climate sustainability in a global movement for healthy people, healthy places, and a healthy planet (see the figure below for a framework for action).
“Climate change could be ‘the biggest global health threat of the 21st century,’ but by working together, we can turn it into this century’s greatest opportunity for public health.” Nick Watts, Secretariat, Global Climate and Health Alliance
Environmental Health, Health Disparities, Health Equity, One Health, Population Health