Understanding the Relationship Between Education and Health
It is now widely recognized that health outcomes are deeply influenced by a variety of social factors outside of health care. The dramatic differences in morbidity, mortality, and risk factors that researchers have documented within and between countries are patterned after classic social determinants of health, such as education and income (Link and Phelan, 1995; CSDH, 2008), as well as placed-based characteristics of the physical and social environment in which people live—and the macrostructural policies that shape them.
A 2013 report from the National Research Council and the Institute of Medicine cited these socioecological factors, along with unhealthy behaviors and deficiencies in the health care system, as leading explanations for the “health disadvantage” of the United States. In a comparison of 17 high-income countries, age-adjusted all-cause mortality rates for 2008 ranged from 378.0 per 100,000 in Australia to 504.9 in the United States. The report found a pervasive pattern of health disadvantages across diverse categories of illness and injury that existed across age groups, sexes, racial and ethnic groups, and social classes (NRC and IOM, 2013).
Recent attention has focused on the substantial health disparities that exist within the United States, where life expectancy varies at the state level by 7.0 years for males and 6.7 years for females (NRC and IOM, 2013) but mortality and life expectancy vary even more substantially across smaller geographic areas such as counties (University of Wisconsin Population Health Institute, 2013; Kulkarni et al., 2011) and census tracts. In many U.S. cities, life expectancy can vary by as much as 25 years across neighborhoods (Evans et al., 2012). The same dramatic geographic disparities can be seen for other outcomes, such as infant mortality, obesity, and the prevalence of diabetes and other chronic diseases.
Of the various social determinants of health that explain health disparities by geography or demographic characteristics (e.g., age, gender, race-ethnicity), the literature has always pointed prominently to education. Research-based on decades of experience in the developing world has identified educational status (especially of the mother) as a major predictor of health outcomes, and economic trends in the industrialized world have intensified the relationship between education and health. In the United States, the gradient in health outcomes by educational attainment has steepened over the last four decades (Goldman and Smith, 2011; Olshansky et al., 2012) in all regions of the United States (Montez and Berkman, 2014), producing a larger gap in health status between Americans with high and low education. Among white Americans without a high school diploma, especially women, life expectancy has decreased since the 1990s, whereas it has increased for others (Olshansky et al., 2012). Death rates are declining among the most educated Americans, accompanied by steady or increasing death rates among the least educated (Jemal et al., 2008).
What accounts for the growing health advantages that exist among people with higher educational attainment? Is it what they learn in school, such as how to live a healthy lifestyle, or the socioeconomic advantages that come from an education? Or is the cross-sectional association between education and health more complex, involving numerous contextual covariables that provide a fuller back story? Despite decades of research documenting the connections between education and health, there is still much to learn about the mechanisms that enable this connection.
Unpacking the reasons for the connections between education and health is not just an exercise in scientific inquiry; it is also essential to setting policy priorities. As increasing attention is focused on the need to address social inequity in order to address health inequities, understanding the links between broad upstream factors such as education and health outcomes becomes a critical challenge. Awareness of the importance of education might help drive investment in education and improvements in educational policy.
Conceptual Framework
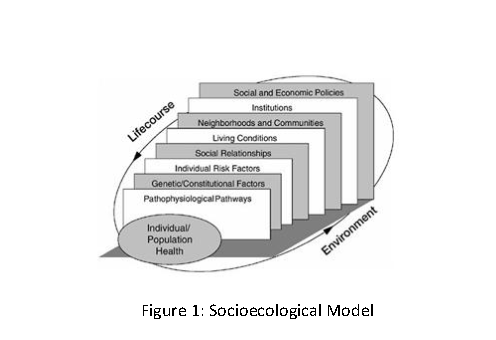
An overarching theoretical framework for the impact of social determinants on health is provided by an ecological model in which individuals and their behaviors are embedded, across the lifespan, within a framework of nested institutional contexts (IOM, 2000; see Figure 1). The individual and his or her characteristics are situated within and affected by the family and household, the community and its institutions (e.g., school, workplace, and civil institutions), and policies of the larger society. Each level brings access to opportunities, as well as constraints on actions and opportunities. Furthermore, these levels interact with one another, such that family resources, for example, may mediate or moderate the resources available within the community. Social scientists widely agree that unequal social status creates unequal access to resources and rewards. Social structure, as embodied in social position, structures individual behaviors and values and therefore affects many of the mediators in the relationship between education and health.
Education is one of the key filtering mechanisms that situate individuals within particular ecological contexts. Education is a driving force at each ecological level, from our choice of partner to our social position in the status hierarchy. The ecological model can therefore provide a context for the numerous ways in which education is linked to our life experiences, including health outcomes. It also provides a framework for understanding the ways in which educational outcomes themselves are conditioned on the many social and environmental contexts in which we live and how these, in turn, interact with our individual endowments and experiences.
Within this rich contextual framework, educational attainment (the number of years of schooling completed) is important but is far from the whole story. Educational attainment is often a key indicator in research studies, not least because it is often measured and recorded; life expectancy is compared by educational attainment because it is the only information about education recorded on death certificates. Besides such obvious measures of the quality of education as proficiency scores and understanding of mathematics, reading, science, and other core content, other dimensions of education are clearly important in the ecological context as well; cognitive development, character development, knowledge, critical thinking and problem solving are a few examples.
In addition, the relationship between years of education and health is not a purely linear function. As part of the literature attempting to clarify the functional form of the relationship between education and health, Montez et al. (2012) have documented a negative relationship between years of education and mortality risk for attainment less than high school graduation, a steep decline for high school graduates (with reduction of risk five times greater than attributable to other years of education), and a continued yet steeper negative relationship for additional years of schooling. The drop at high school graduation points to the importance of obtaining credentials in addition to the other benefits associated with educational attainment.
In this paper we review the health benefits associated with education, focusing on the primary mechanisms, both distal and proximate, by which education may be considered a driving force in health outcomes. We take a socioecological approach by presenting these concepts in a hierarchy, moving from the level of the person to the community/institution and then the larger social/policy context. Next, we turn to issues of causality that can make it difficult to draw conclusions about the relationship between education and health. These include reverse causality and selection, in which education may be impacted by ill health, and confounding, where both education and health are affected by some other causal factor(s) that may also provide important clues about the root causes of poor education and poor health.
The Health Benefits Associated with Education
Among the most obvious explanations for the association between education and health is that education itself produces benefits that later predispose the recipient to better health outcomes. We may think of these returns from education, such as higher earnings, as subsequent “downstream” benefits of education. Following the socioecological framework presented in the introduction, we describe a range of potential downstream impacts of education on health, starting with the ways individuals experience health benefits from education then going on to discuss the health-related community (or place-based) characteristics that often surround people with high or low education, and closing with the larger role of social context and social policy.
Impact at the Individual Level
Education can impart a variety of benefits that improve the health trajectory of the recipient. We discuss its role in enhancing noncognitive and cognitive skills and access to economic resources, and we highlight the impacts of these on health behaviors and health care usage. Although this section focuses specifically on the health benefits of education, we do so in full knowledge that education is also impacted by health, development, and a host of personal, community, and contextual factors.
Education Impacts a Range of Skills
Education contributes to human capital by developing a range of skills and traits, such as cognitive skills, problem-solving ability, learned effectiveness, and personal control (Mirowski and Ross, 2005). These various forms of human capital may all mediate the relationship between education and health.
Personality traits (also known as “soft” or noncognitive skills) are associated with success in later life, including employment and health. The “Big Five” personality factors include conscientiousness, openness to experience, extraversion, agreeableness, and neuroticism/emotional stability (Heckman and Kautz, 2012). Roberts et al. (2007) postulate three pathways whereby personality traits may impact mortality: through disease processes (e.g., response to stress), health-related behaviors, and reactions to illness. A review by Roberts et al. (2007) suggests that the strength of association between the “Big Five” personality traits and mortality is to that of IQ and stronger than socioeconomic status (SES). Although enduring, these skills are also mutable, and research indicates that educational interventions to strengthen these skills can be important, especially among children in disadvantaged areas, who may find it more difficult to refine these skills at home and in their social environments.
Personal control, also described in the literature in terms of locus of control, personal efficacy, personal autonomy, self-directedness, mastery, and instrumentalism (Ross and Wu, 1995), is another soft skill associated with educational attainment. According to the authors, “Because education develops one’s ability to gather and interpret information and to solve problems on many levels, it increases one’s potential to control events and outcomes in life. Moreover, through education one encounters and solves problems that are progressively more difficult, complex, and subtle, which builds problem-solving skills and confidence in the ability to solve problems” (Ross and Wu, 1995, p. 723).
Personal control can impact individuals’ attitudes and behaviors, potentially including health behaviors. Furthermore, an individual’s sense of mastery and control may mediate stress, possibly by facilitating better coping mechanisms. Lack of personal control, on the other hand, may provoke physiological responses, leading to suppression of the immune system (Ross and Wu, 1995, p. 723).
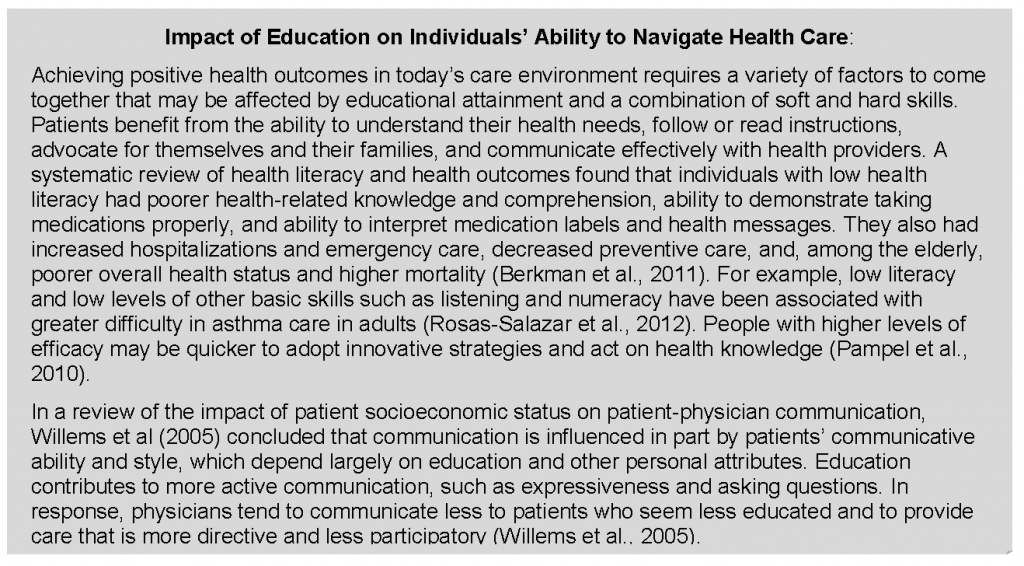
In addition to its impact on soft skills, education has the potential to impart skills in reading, mathematics, and science/health literacy that could contribute to an individual’s health. Learners of English as a second language are helped to overcome language barriers that can interfere with understanding of health needs. Education may also improve a range of other skills, such as cognitive ability, literacy, reaction time, and problem-solving. Pathways from these skills to health outcomes may be indirect, via attainment of better socioeconomic circumstances or behavior, but they may also apply directly in understanding the increasingly complex choices individuals face in understanding health priorities and medical care needs. Skills such as higher cognitive ability and health literacy may also lead directly to improved health outcomes because of an enhanced “ability to comprehend and execute complex treatment regimens” and better disease self-management (Maitra, 2010). A strong education may be important in both navigating health care and making choices about lifestyle and personal health behaviors. Cutler and Lleras-Muney (2010) report that increased cognitive ability resulting from education contributes significantly to the education gradient in health behaviors.
Education Increases Economic and Social Resources
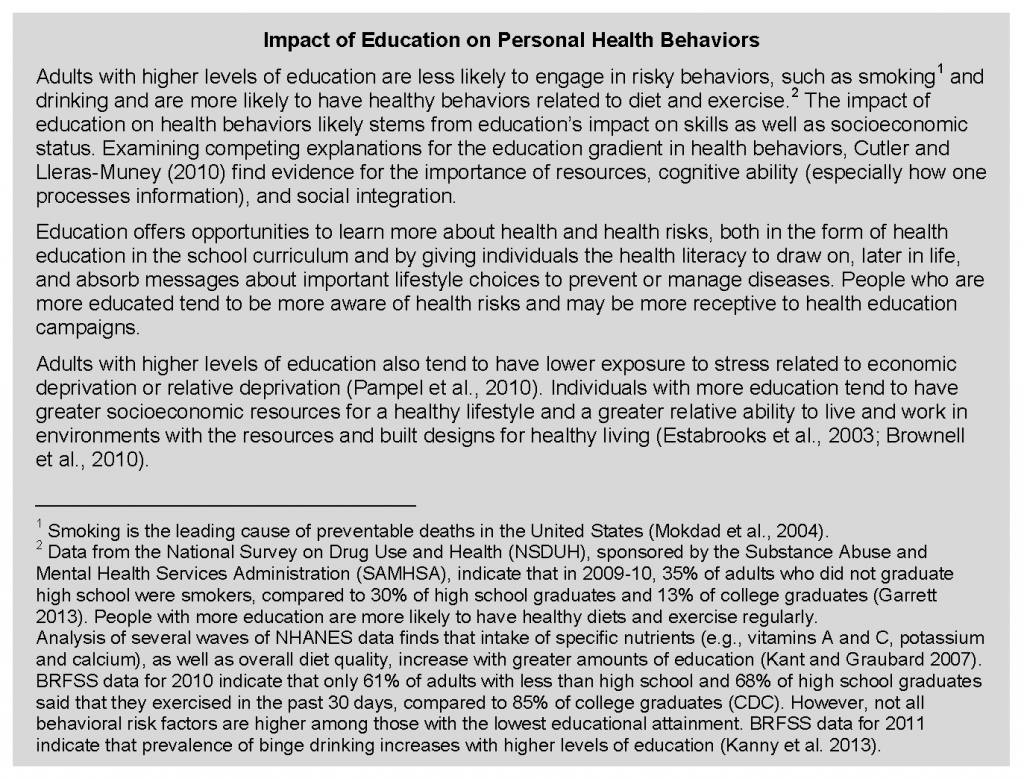
A large part of the impact of education on health flows through the attainment of economic resources, such as earnings and wealth, as well social resources such as access to social networks and support. Adults with more education are less likely to experience unemployment and economic hardship and will have greater access to a variety of important material, financial and social resources. Link and Phelan (1995) point out that the specific mechanisms linking SES to health have changed over time but that SES remains a fundamental social cause of disease because it involves “access to resources that can be used to avoid risks or to minimize the consequences of disease once it occurs” (p. 87).
Economic Resources
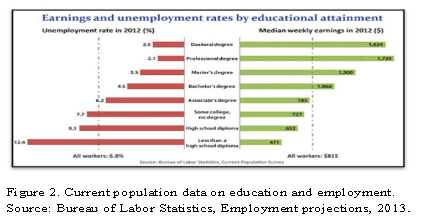
Adults with a higher education—especially in today’s knowledge economy—have conspicuous advantages in gaining employment and finding desirable jobs (see Figure 2). Advanced degrees give workers an advantage in obtaining rewarding jobs that offer not only higher salaries and job satisfaction but other health-related benefits, such as health insurance coverage, (Adults with health insurance in the United States use more physician services and have better health outcomes compared to uninsured or inconsistently insured adults [NRC, 2009; Freeman et al., 2008; Hadley, 2003]) worksite health promotion programs, and worksite policies that protect occupational safety. An inadequate education markedly increases the risk of unemployment. (In 2012, unemployment was 12.4 percent among adults who did not graduate high school, compared to 8.3 percent among adults with a high school diploma and 4.5 percent among college graduates [BLS, 2013]. 5 A body of evidence links unemployment to adverse health outcomes. For example, a higher percentage of employed persons reported in 2010 that they were in excellent or very good health [62.7 percent] than did persons who were unemployed for less than 1 year [49.2 percent] or unemployed for more than 1 year (39.7 percent). The unemployed also reported more physically and mentally unhealthy days in the past 30 days [Athar et al., 2013]).
Income and wealth are leading predictors of health status (CSDH, 2008; Braveman et al., 2010), and accumulated financial strain has been shown to impact health above and beyond the effects of income and wealth (Shippee et al., 2012). In today’s society, economic resources are inextricably linked to education. In 2012, the median wage for college graduates was more than twice that of high school dropouts and more than one and a half times higher than high school graduates (BLS, 2013). Weekly earnings rise dramatically for Americans with a college or advanced degree. A higher education has an even greater effect on lifetime earnings, a pattern that is true for men and women, for blacks and whites, and for Hispanics and non-Hispanics. (According to 2006–2008 data, the lifetime earnings of a Hispanic male are $870,275 for those with less than a ninth-grade education but $2,777,200 for those with a doctoral degree. The corresponding lifetime earnings for a non-Hispanic white male are $1,056,523 and $3,403,123 [Julian and Kominski, 2011]). Economic vulnerability can affect health through a cascade effect on the ability to acquire resources that are important to health: food, stable housing, transportation, insurance, and health care (Braveman, et al., 2011). People with low income are more likely to be uninsured and to be vulnerable to the rising costs of health care, which insurance carriers are increasingly shifting to patients through higher copayments, deductibles, and premiums (In 2012, one-fourth [24.9 percent] of people in households with annual income less than $25,000 had no health insurance coverage, compared to 21.4 percent of people in households with income ranging from $25,000 to $49,999; the figure was 15.0 percent in households with income ranging from $50,000 to $74,999 and 7.9 percent with income of $75,000 or more [DeNavas-Walt et al., 2013]). Individuals with higher incomes have more resources to purchase healthy foods, to afford the time and expenses associated with regular physical activity, to have easy transportation to health care facilities or work locations, and to afford health care expenses. (According to 2010 Behavioral Risk Factor Surveillance System [BRFSS] data, 27 percent of adults with less than a high school education reported not being able to see a physician because of cost, compared to 18 percent and 8 percent of high school and college graduates, respectively [CDC, 2014]). Accordingly, the costs of a healthy lifestyle pose more of a barrier for people with less education. The health implications of these financial barriers to health care are well documented: the uninsured are less likely to receive preventive care or help with disease management (HHS, 2013, p. 9-1), and they have a higher risk of death (IOM, 2003a).
Social Resources
Educational attainment is associated with greater social support, including social networks that provide financial, psychological, and emotional support. Social support includes networks of communication and reciprocity. Individuals in a social network can relay information, define norms for behavior, and act as modeling agents. Those individuals with higher levels of education may also have higher levels of involvement with civic groups and organizations. Conversely, low social support (i.e., not participating in organizations, having few friends, being unmarried, or having lower-quality relationships) is associated with higher mortality rates (Kaplan et al., 1994; Seeman, 1996) and poor mental health (Seeman, 1996). Berkman et al. (2000) linked social integration to health outcomes in a causal chain that begins with the macrosocial and ends with psychobiological processes. They propose several mechanisms through which social integration affects health: social support, social influence, social engagement/attachment, and access to goods and resources (Berkman et al., 2000, p. 846). Social connection can be an important buffer to the negative health consequences of health stressors. Marriage imparts benefits in longevity, but weaker network ties can also have important health effects, such as the effects of peers on behavior (Smith and Christakis, 2008). The effect of social networks on smoking cessation is a well-known example (Christakis and Fowler, 2008).
Impact at the Community Level
Individuals with more education benefit not only from the resources that schooling brings to them and their families but also from health-related characteristics of the environments in which they tend to live, work, and study. Although there are many methodological challenges in estimating community-level effects on individuals (Kawachi and Berkman, 2003; Kawachi and Subramanian, 2007), communities may confer a range of benefits or risks that can impact health. In the midst of growing recognition that “place matters” to health, many studies have tried to estimate neighborhood effects on outcomes such as child/youth educational attainment, behavioral/well-being outcomes, or health status and mortality. (For example, Ross and Mirowsky (2008), using multilevel analysis of survey data from Illinois, addressed the question of whether community SES impacts health above and beyond the contributions of individual SES measures. They found that individual-level indicators of SES explained most of the variation in physical functioning (about 60 percent) but that neighborhood-level measures had a significant influence as well.) Given the wide range of methodologies and data sources utilized, findings are not uniform among such studies, but there is general agreement that a relatively modest neighborhood effect exists independent of individual and family-level factors (Kawachi and Berkman, 2003; Leventhal and Brooks-Gunn, 2000; Steptoe and Feldman, 2001). (Kawachi and Berkman (2003) call attention to the methodological difficulties of estimating neighborhood effects while controlling for individual SES, when some neighborhood effects may operate via their impact on individual outcomes, thus “adjusting away the variation of interest” (p. 9). Winkleby et al. (2006) examined the interaction between neighborhood SES and individual SES and found that low SES individuals living in higher SES neighborhoods had higher mortality rates compared to low SES individuals living in low or moderate SES neighborhoods.)) Effects that appear to occur at the neighborhood level may represent aggregated individual characteristics (compositional effects), neighborhood variability (contextual effects), or local manifestations of larger-scale processes (e.g., higher-level planning or regulatory decisions) (Shankardass and Dunn, 2011). Furthermore, it is important to recognize the dynamic interaction that occurs between the individual and the environment (Rhodes et al., 2011) and conceptions of space as “relational geographies” (Conceptualization of space as a “relational geography” emphasizes aspects such as networks rather than boundaries, social rather than physical distance, mobility of populations, and dynamic characteristics of places (Cummins et al., 2007)) (Cummins et al., 2007).
At one level, community characteristics matter because access to resources that are important to health is contingent on community-level resources and institutions. Macintyre and Ellaway (2003) categorize these as physical features, services, sociocultural features, reputation, and availability of healthy environments at home, work, and play. Theories about the mechanisms by which social environments affect the health of individuals also focus on community characteristics such as social disorganization, social control, social capital, and collective efficacy (Sampson, 2003). Kawachi et al. (2013) note that communities with higher social capital tend to be more resilient in the face of disasters and are better able to employ informal control mechanisms to prevent crime.
Through a combination of resources and characteristics, communities expose individuals to varying levels of risk versus safety (e.g., crime, unemployment, poverty, and exposure to physical hazards) and provide different levels of resources (e.g., food supply, green space, economic resources, and health care). One notable resource that differs among communities is the quality of education available. Low-income neighborhoods often have fewer good schools, not least because public schools tend to be poorly resourced by low property taxes and cannot offer attractive teacher salaries or properly maintain buildings, supplies, and school safety. Adverse community factors can compound the difficulty that children face in obtaining a good education while also compromising their health trajectory.
Below we touch on several additional community characteristics that have been linked to health outcomes, including food access, spaces and facilities for physical activity, access to health care, community economic resources, crime and violence, and environmental exposure to toxins.
- Food access. Unhealthy eating habits are linked to numerous acute and chronic health problems, such as diabetes, hypertension, obesity, heart disease, and stroke as well as higher mortality rates, but access to healthier foods tends to be limited in neighborhoods with lower median incomes and lower levels of educational attainment. In one study, access (Defined as at least one healthier food retailer within the census tract or within one-half mile of tract boundaries) to healthier food outlets was 1.4 times less likely in census tracts with fewer college-educated adults (less than 27 percent of the population) than in tracts with a higher proportion of college-educated persons; these differences varied by region and were highest in the South and lowest in the West and Northeast (Grimmet al., 2013). Conversely, low-income neighborhoods often have an oversupply of fast-food restaurants, convenience stores, bodegas, liquor stores, and other outlets that sell little fresh produce but promote inexpensive calorie-dense foods and beverages.
- Spaces and facilities for physical activity. People with higher education and income are more likely to live in neighborhoods that provide green space (e.g., parks), sidewalks, and other places that enable residents to walk and cycle to work and shopping, exercise, and outside play. Lower-income neighborhoods and those with higher proportions of nonwhite residents are also less likely to have commercial exercise facilities (Powell et al., 2006). The health benefits of green space have been documented in urban environments, especially for lower-income, young, and elderly populations (Maas et al., 2006). A longitudinal study in Great Britain found immediate, positive mental health effects of moving to urban areas with more green space (Alcock et al., 2014).
- Access to health care. Because of the maldistribution of health care providers in the United States (HHS, 1998), access to clinicians and facilities tends to be in shortest supply in rural and low-income areas. Thus, apart from whether residents have the health insurance coverage and resources to afford health care, they may struggle to find local primary care providers, specialists, and hospitals that provide quality health care services.
- Community economic resources. The lack of jobs in low-income communities can exacerbate the economic hardship that is common for people with less education, who are more likely to live in communities with a weak economic base that is unattractive to businesses, employers, and investors and are thereby often caught in a self-perpetuating cycle of economic decline and marginalization.
- Crime and violence. Community crime rates can impact health through the direct effects of violent crimes on victims, such as trauma and high youth mortality rates. Crime can also affect health indirectly, such as through fear of crime (Stafford et al., 2007) or the cumulative stress of living in unsafe neighborhoods. The high incarceration rates of residents in some communities can have deleterious effects on social networks, social capital, and social control, further compromising public health and safety (Clear, 2007). The 2006 and 2007 rounds of the American Community Survey found that, among young male high school drop-outs, nearly 1 in 10 was institutionalized on a given day in 2006–2007 versus fewer than 1 of 33 high school graduates (Sum et al., 2009).
- Environmental exposure to toxins. People of color and those with less education are more likely to live in neighborhoods that are near highways, factories, bus depots, power plants, and other sources of air and water pollution. A large body of research on environmental justice has documented the disparate exposure of low-income and minority neighborhoods to hazardous waste, pesticides, and industrial chemicals (Bullard et al., 2011; Calnan and Johnson, 1985). This exposure to toxins is perhaps the most undiscriminating place-based characteristic because residents’ personal socioeconomic advantages (e.g., education, income) offer no protection against the adverse health consequences of inhalation or ingestion of such toxins.
The Larger Social Context and Social Policy
Health inequities are driven, in large part, by the social context in which people are born, live, and work, that is, the social policies that shape resources, institutions, and laws; the economic system through which material and financial resources are created and distributed; and the social norms that govern interactions. The conditions in which people live—for example, the built environment, public transportation, urban design, crime rates, food deserts, and the location of polluting factories—are determined by macrostructural policies and the cultural values that shape them. Formulation of effective analyses and solutions to problems affecting health must address factors that go beyond the level of the individual and proximal risk factors (O’Campo and Dunn, 2011). These influences have been recognized by organizations concerned with health outcomes locally, nationally, and internationally. The World Health Organization calls for improved living and working conditions, social protection policy supportive of all, reduced inequality, and strengthened governance and civil society (CSDH, 2008). Healthy People 2020 has many policy objectives for health, including improved environmental conditions (e.g., air/water quality and exposure to hazards), violence prevention, poverty reduction, and increased rates of postsecondary education. (See http://www.healthypeople.gov/2020/topicsobjectives2020/default.aspx.) The Place Matters team in Alameda County, California, has identified five policy areas to impact health outcomes locally: economics, education, criminal justice, housing, and land use and transportation (Alameda County Public Health Department, n.d.).
Decisions made by society, voters, and policy makers—both within and outside of government—exert deep influences on education itself, as well as on the institutions and resources that populate the socioecological framework linking education and health. For example, in other societies, the adverse health consequences of poverty are often buffered by social services that act to safeguard the health of children, young parents, and other vulnerable groups. Bradley et al. (2011) found that while most OECD (Organisation for Economic Co-operation and Development) countries spent more on social services than on health expenditures, the converse was true in the United States. (The average ratio of social to health expenditures in OECD countries from 1995 to 2005 was 2.0; the ratio in the U.S. was 0.91. [Bradley et al. 2011]). Likewise, economic policies have a large influence on the employment and wealth-building opportunities of workers. Major economic and technological shifts of the last few decades have favored “nontradable” service jobs in sectors such as government and health care while manufacturing jobs have moved to less developed countries in large numbers. Remaining jobs in the “tradable” sectors such as technology and finance increasingly require advanced skill sets (Spence and Hlatshwayo, 2011). These employment trends provide a critical context in the relationship between education and health—those unable to acquire the necessary education to be competitive in an increasingly restrictive job environment are vulnerable to long-term economic hardship. Educational opportunities, however, are not equally distributed in the United States. Public school funding, largely dependent on local property taxes, varies widely both within and between states. The best-funded school systems in the United States have per pupil expenditures almost four times the per pupil expenditures in the lowest spending schools. (In 2011, total state per pupil education expenditures ranged from $6,200 to $16,700; among the 100 largest school systems in the United States, per pupil funding ranges from $5,400 to almost $20,000 [Census Bureau, 2013]). Although early studies failed to find a strong relationship between school funding amounts and student achievement, more recent meta-analysis has confirmed the importance of school funding for individual achievement (Greenwald et al., 1996).
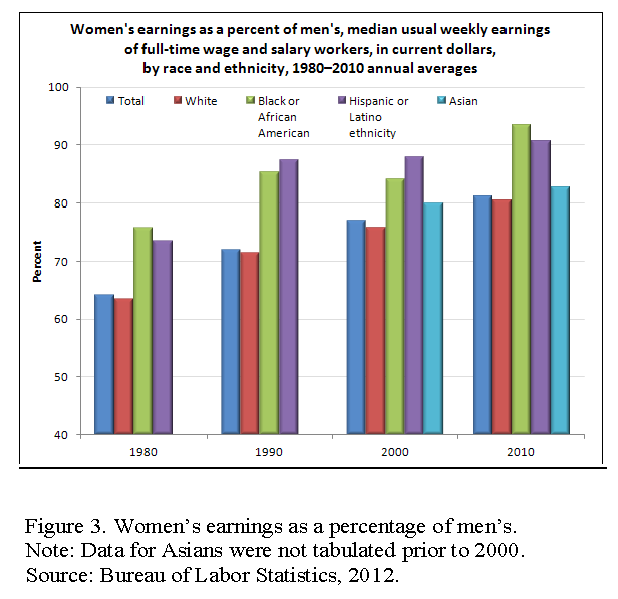
Inequality by gender, race, ethnicity, sexual orientation, and disability affect risks and opportunities for people throughout the world. Figure 3 (See Women’s earnings as percent of men’s in 2010. http://www.bls.gov/opub/ted/2012/ted_20120110.htm) shows persistent gender and race disparities in earnings. Ridgeway (2014) calls attention to the cultural as well as the material dimensions of inequality: “Cultural status beliefs work their effects on inequality primarily at the social-relational level by shaping people’s expectations for themselves and others and their consequent actions in social contexts” (p. 3). Social status hierarchies based on “categories” of difference solidify and perpetuate differentials in power and control of resources—thus leading to material inequalities. Indeed, income inequalities in the United States are significant and have become more pronounced, with wages at the lower or middle of the income distribution stagnating or falling while those at the top continue to rise. This division has continued during recovery from the Great Recession, during the first three years of which 95 percent of income gains accrued to the top 1 percent of earners (Saez, 2013). The Census Bureau reports that the Gini coefficient, which measures income inequality, has risen from 0.394 in 1970 to 0.469 in 2010; the share of household income earned by the bottom quintile was 3.3 percent in 2010, compared to 50.2 percent among the top quintile. (Table A-3: Selected Measures of Household Income Dispersion: 1967 to 2010. https://www.census.gov/hhes/www/income/data/historical/inequality/IE-1.pdf)
Historical, economic, and cultural factors play a central role in opportunities, values, and behaviors. The continuing racial residential segregation and increasing economic segregation of urban landscapes affect the life chances of those living in concentrated poverty “irrespective of personal traits, individual motivations, or private achievements” (Massey and Denton, 1993, p.3). Massey and Denton argue that residential segregation and “hypersegregation” expose residents to higher levels of social problems. Wilson (1987) links historical and economic factors in his description of the racial division of labor resulting from “decades, even centuries, of discrimination and prejudice” with the result that “because those in the low-wage sector of the economy are more adversely affected by impersonal economic shifts in advanced industrial society, the racial division of labor is reinforced” (p. 12).
Reverse Causality and Selection
Education’s association with health may reflect not only the health benefits of education but also a selection phenomenon caused by the detrimental effects of illness on educational success. Basch (2011) identifies five causal pathways by which health may impact motivation and ability to learn— sensory perceptions, cognition, school connectedness and engagement, absenteeism, and temporary or permanent dropping out (p. 596). For example, chronic health conditions can impact children’s development and educational performance (Taras and Potts-Datema, 2005). Such children are more likely to have absences for medical reasons and to be distracted by health concerns. Nonetheless, research evidence demonstrating that poor health has a causal relationship with educational outcomes is incomplete (Currie, 2009), and findings of the overall effects range from about 1.4 years reduced attainment (Estimated for 16-year-old white males from 1979 youth cohort of the National Longitudinal Surveys of Youth (NLSY) using a dynamic programming model of joint decisions of young men on schooling, work, health expenditure, and savings (Gan and Gong, 2007)) (Gan and Gong 2007) to about half a year (Goldman and Smith 2011), but there are notable exceptions. For example, evidence across countries and time periods demonstrate the harmful effect of low birth weight on education (Currie, 2009; Eide and Showalter, 2011). Disease, malnutrition, and prenatal and childhood exposures to toxins can also impact physical and cognitive development and educational achievement (Pridmore, 2007).
The extent to which reverse causality contributes to the association between education and health requires further study, but longitudinal data—the most compelling evidence to resolve the controversy—tend to suggest that most of the association is attributable to the downstream benefits of education. Eide and Showalter (2011) reviewed studies incorporating a range of methodologies that attempted to examine causal links between education and health outcomes. Studies of natural experiments in the United States (e.g., changes in compulsory school laws) generally found evidence for a causal link with mortality. Twin studies found evidence for causal links between years of schooling and self-reported health, the probability of being overweight (among men but not women), and the effects on college attendance on preventive health care later in life. Link and Phelan (1995) also discussed research attempting to show the direction of causality using quasi-experimental approaches, longitudinal designs, and analyses of risk factors that cannot be attributed to individual illness (e.g., plant closings). They concluded that these studies “demonstrated a substantial causal role for social conditions as causes of illness” (p. 83).
Conditions Throughout the Life Course That Affect Both Health and Education
A third way that education can be linked to health is when education acts as a proxy for factors throughout the life course—most notably in early childhood—that affect both education and health. For example, as noted earlier, the social and economic environment facing individuals and households and the stresses and allostatic load induced by material deprivation can affect success in school (and work) while also inducing biological changes and unhealthy behaviors that can increase the risk of disease. Although this can occur throughout the life course, increasing attention is being placed on the role of these factors on children before they reach school age.
Early Childhood Experiences
The education community has long understood the connections between early life experiences and educational success. It is well established that school readiness is enhanced by positive early childhood conditions—for example, fetal well-being and social-emotional development (Denhem, 2006), family socioeconomic status, (Children’s birth weight, developmental outcomes, health status (e.g., obesity and specific health conditions), disability, and success in school are strongly linked to parents’ education and family income and assets (Williams Shanks and Robinson, 2013; Chapman et al., 2008; Currie, 2009)) neighborhood socioeconomic status (Jencks and Mayer, 1990; Mayer and Jencks, 1989), and early childhood education (Barnett and Belfield, 2006) — but some of these same exposures also appear to be vital to the health and development of children and their future risk of adopting unhealthy behaviors and initiating adult disease processes.
Below are several examples from the literature of early childhood experiences that influence health.
- Low birth weight affects not only educational outcomes but also health and disability (Avchen et al., 2001).
- Nurturing relationships beginning at birth, the quality of the home environment, and access to stimulation provide a necessary foundation for children to grow and thrive (Heckman, 2006). One example of this is the importance of child-directed speech during infancy for language skills (Weisleder and Fernald, 2013). The effects of stress can be reduced when children have a responsive and supportive caregiver available to help cope with stress and provide a protective effect (Shonkoff and Garner, 2012).
- Unstable home and community life, such as economic factors, family transitions, housing instability, and school settings, can harm child development and later outcomes (Sandstromand Huerta, 2013). In one study, (Data were based on research by the National Poverty Center on the basis of the Michigan Recession and Recovery Study (MRRS) of adults ages 19–64 in southeastern Michigan. The researchers examined the relationship between various forms of housing instability and health, controlling for prior health problems and sociodemographic characteristics) homelessness and struggles with mortgage payments and foreclosure were predictive of self-rated health, and these combined with other categories (e. g., moved for cost in past 3 years, behind on rent) also predicted mental health problems (Burgard et al., 2012).
- Family and neighborhood socioeconomic status not only affect education but also predict developmental and health trajectories as children grow and develop (Case et al., 2002; Duncan et al.,1994). Duration and timing of childhood poverty are important. Longitudinal studies indicate that the largest effects of poverty on child outcomes are during early childhood development, when children experience poverty for multiple years, and when they live in extreme poverty (Brooks-Gunn and Duncan 1997). Guo (1998) also found that timing of poverty during early adolescence is important for adolescent achievement.
Biological Pathways
A growing body of research suggests that the similar root causes that lead children to poor educational outcomes and poor health outcomes may not operate via separate pathways but may relate to the biology of brain development and the pathological effects of early childhood exposure to stress and adverse childhood events (ACEs). Children in low SES households are more likely to experience multiple stressors that can harm health and development (Evans and Kim, 2010), mediated by chronic stress (Evans et al., 2011). These disruptions, along the pathways listed below, can thereby shape educational, economic, and health outcomes decades and generations later (NRC and IOM, 2000).
- Neuroanatomy and neuroplasticity: Infants and toddlers exposed to toxic stress, social exclusion and bias, persistent poverty, and trauma may experience changes in brain architecture and development that affect cognition, the ability to learn new skills, behavioral and stress regulation, executive function, and the capacity to adapt to future adversity (Hackman, 2010; Gottesman and Hanson, 2005).
- Endocrine disruption: Early life stressors also appear to cause physiological increases in allostatic load that promote stress-related diseases later in life (Shonkoff and Garner, 2012). Such stressors may, for example, disrupt the hypothalamic-pituitary-adrenal axis of the endocrine system and stimulating overproduction of stress-related hormones that are thought to adversely affect end organs and lead later in life to heart disease and other adult health problems (McEwen, 2012).
- Immune dysregulation: The release of interleukins and other immune reactant proteins is thought to create conditions of chronic inflammation that may increase the risk of heart disease and other chronic diseases later in life (McEwen, 2012).
- Epigenetic changes: Chronic stress is thought to affect methylation of DNA and cause epigenetic changes that “turn on” expression of genes that may cause cancer and other diseases (Zhang and Meaney, 2010).
Enhanced understanding of these biological pathways is shedding light on research, first reported in the 1990s, that called attention to the correlation between adult disease rates and a history of childhood exposure to ACEs. In a seminal study on the subject, the Adverse Childhood Experiences study, Felitti et al. (1998) surveyed more than 13,000 adult patients at Kaiser Permanente and asked whether they recalled exposure to seven categories of ACEs: psychological, physical, or sexual abuse; violence against the mother; living in a household with members who are substance abusers; mentally ill or suicidal; or imprisonment (Felitti et al., 1998). More than half the adults recalled ACEs as children, and those with greater trauma were more likely to report unhealthy behaviors as adults (e.g., smoking, physical inactivity, alcoholism, drug abuse, multiple sexual partners) and to have a history of depression or a suicide attempt. The researchers reported a dose-response relationship: those who recalled four categories of ACEs faced significant odds ratios for adult diseases, including ischemic heart disease (2.2), cancer (1.9), stroke (2.4), chronic lung disease (3.9), and diabetes (1.6).
The ACE study and subsequent studies with similar results relied on retrospective designs that faced the limitation of recall bias (relying on the memory of adults); recollections of ACEs were vulnerable to the criticism that sick adults might have skewed perceptions of their childhood experiences. Nevertheless, prospective studies that documented ACEs contemporaneously during childhood have also documented higher rates of disease when the children were followed into adulthood. The Centers for Disease Control and Prevention maintains a website that is cataloguing the burgeoning research on ACEs (CDC, 2014), and increasing attention is shifting toward strategies for policy and clinical practice to help ameliorate childhood exposure to ACEs and to buffer their adverse biological and psychosocial effects.
The building evidence that stress and other contextual factors can have effects on both education and health throughout the life course—as in the lasting effects on development, behavior, learning, and health of children—adds important insights for understanding the correlation between education and health. As discussed earlier in this paper, reverse causality plays some role in the association, and a much larger influence comes from the downstream benefits of education (e.g., greater socioeconomic resources and personal skills), but the upstream influence of adverse experiences on the young child also cannot be ignored. The effects of ACEs on the developing brain and on behavior can affect performance in school and explain setbacks in education—but it can also affect health outcomes. Thus, the correlation between reduced education and illness may have as much to do with the seeds of illness that are planted before children ever reach school age than with the consequences of education itself. They end up with fewer years of education and greater illness, but an important way to improve their health is to address the root causes that expose children to stress in the first place.
References
- Alameda County Public Health Department. n.d. Place matters. Available at: www.acphd.org/media/114473/placematters_overview.pdf (accessed April 10, 2014).
- Alcock, I., M. P. White, B. W. Wheeler, L. E. Fleming, and M. H. Depledge. 2014, Longitudinal effects on mental health of moving to greener and less green urban areas. Environmental Science and Technology 48(2):1247–1255. https://doi.org/10.1021/es403688w
- Athar, H. M., M. H. Chang, R. A. Hahn, E. Walker, and P. Yoon. 2013. Unemployment—United States, 2006 and 2010. CDC health disparities and inequalities report—United States, Centers for Disease Control. Morbidity and Mortality Weekly Report 62(3):27–32. Available at: http://www.cdc.gov/mmwr/pdf/other/su6203.pdf (accessed February 7, 2014).
- Avchen, R. N., G. Scott, and C. A. Mason. 2001. Birth weight and school-age disabilities: A population-based study. American Journal of Epidemiology 154(10):895–901. https://doi.org/10.1093/aje/154.10.895
- Barnett, W. S., and C. R. Belfield. Early childhood development and social mobility. 2006. The Future of Children 16(2):73–98. https://doi.org/10.1353/foc.2006.0011
- Basch, C. E. 2011. Healthier students are better learners: A missing link in school reforms to close the achievement gap. Journal of School Health 81(10):593–598. Available at: https://healthyschoolscampaign.org/wp-content/uploads/2017/03/A-Missing-Link-in-School-Reforms-to-Close-the-Achievement-Gap.pdf (accessed May 26, 2020).
- Berkman, L. F., T. Glass, I. Brissette, T. E. Seeman. 2000. From social integration to health: Durkheim in the new millennium. Social Science and Medicine 51:843–857. https://doi.org/10.1016/s0277-9536(00)00065-4
- Berkman, N. D., S. L. Sheridan, K. E. Donahue, D. J. Halpern, and K. Crotty. 2011. Low health literacy and health outcomes: An updated systematic review. Annals of Internal Medicine 155(2):97–107. https://doi.org/10.7326/0003-4819-155-2-201107190-00005
- BLS (Bureau of Labor Statistics). 2013. Employment projections. Available at: http://www.bls.gov/emp/ep_chart_001.htm (accessed February 7, 2014).
- BLS. Women’s earnings as a percent of men’s in 2010. 2012. Available at: http://www.bls.gov/opub/ted/2012/ted_20120110.htm (accessed June 3, 2014).
- Boote, J., R. Telford, and C. Cooper. 2002. Consumer involvement in health research: A review and research agenda. Health Policy 61:213–236. https://doi.org/10.1016/s0168-8510(01)00214-7
- Bradley E. H., B. R. Elkins, J. Herrin, and B. Elbel. 2011. Health and social services expenditures: Associations with health outcomes. BMJ Quality and Safety 20:826–831. https://doi.org/10.1136/bmjqs.2010.048363.
- Braveman, P., S. Egerter, and C. Barclay. 2011. Issue Brief Series: Exploring the Social Determinants of Health: Income, Wealth, and Health. Princeton, NJ, Robert Wood Johnson Foundation. Available at: https://www.rwjf.org/en/library/research/2011/04/how-social-factors-shape-health1.html (accessed May 26, 2020).
- Braveman, P. A., C. Cubbin, S. Egerter, D. R. Williams, and E. Pamuk. 2010. Socioeconomic disparities in health in the United States: What the patterns tell us. American Journal of Public Health 100(Suppl. 1):S186–S196. https://doi.org/10.2105/AJPH.2009.166082
- Brooks-Gunn, J., and G. J. Duncan. 1997. The effects of poverty on children. The Future of Children: Children and Poverty 7:55–71. Available at: https://pubmed.ncbi.nlm.nih.gov/9299837/ (accessed May 26, 2020).
- Brotaneka, J. M., C. E. Seeley, and G. Flores. 2008. The importance of cultural competency in general pediatrics. Current Opinion in Pediatrics 20:711–718. https://doi.org/10.1097/MOP.0b013e328317efff
- Brownell, K. D., R. Kersh, D. S. Ludwig, R. C. Post, R. M. Puhl, M. B. Schwartz, and W. C. Willett. 2010. Personal responsibility and obesity: A constructive approach to a controversial issue. Health Affairs 29(3):379–387. https://doi.org/10.1377/hlthaff.2009.0739
- Bullard, R. D., G. S. Johnson, and A. O. Torres. 2011. Environmental health and racial equity in the United States: Building environmentally just, sustainable and livable communities. Washington, DC: American Public Health Association. Available at: https://hefn.org/learn/resource/environmental_health_and_racial_equity_in_the_united_states_building_environmentally (accessed May 26, 2020).
- Burgard, S., K. Seefeldt, and S. Zelner. 2012. Housing instability and health: Findings from the Michigan Recession and Recovery Study. Population Studies Center Research Report 12-749. Ann Arbor, MI: University of Michigan Institute for Social Research. Available at: http://www.psc.isr.umich.edu/pubs/pdf/rr12-749.pdf (accessed February 26, 2014).
- Calnan, M. and Johnson, B. 1985. Health, health risks, and inequalities: An exploratory study of women’s perceptions. Sociology of Health and Illness (7): 55-75. https://doi.org/10.1111/1467-9566.ep10831360
- Case, A., D. Lubotsky, and C. Paxson. 2002. Economic status and health in childhood: The origins of the gradient. American Economic Review 92:1308–1334. https://doi.org/10.1257/000282802762024520
- CDC (Centers for Disease Control). 2014. Behavioral Risk Factor Surveillance System, 2010 BRFSS data. Office of Surveillance, Epidemiology, and Laboratory Services. Available at: http://www.cdc.gov/brfss/data_tools.htm (accessed February 14, 2014).
- Chapman, D. A., K. G. Scott, and T. L. Stanton-Chapman. 2008. Public health approach to the study of mental retardation. American Journal on Mental Retardation 113(2):102–116. Available at: http://meridian.allenpress.com/ajidd/article-pdf/113/2/102/2027787/0895-8017(2008)113[102_phatts]2_0_co_2.pdf (accessed May 28, 2020).
- Christakis, N. A., and J. H. Fowler. 2008. The collective dynamics of smoking in a large social network. New England Journal of Medicine 358:2249–2258. https://doi.org/10.1056/NEJMsa0706154
- Clear, T. R. 2007. Impact of incarceration on community public safety and public health. In Public health behind bars: From prisons to communities, edited by R. B Greifinger, J. A. Bick, and J. Goldenson. New York: Springer. Pp. 13–24.
- CSDH (Commission on Social Determinants of Health). 2008. Closing the gap in a generation: Health equity through action on the social determinants of health. Geneva, Switzerland: World Health Organization, Commission on Social Determinants of Health. Available at: http://www.who.int/social_determinants/thecommission/finalreport/en/ (accessed April 11, 2014).
- Cummins, S., S. Curtis, A. V. Diez-Roux, and S. Macintyre. 2007. Understanding and representing “place” in health research: A relational approach. Social Science and Medicine 65:1825–1838. https://doi.org/10.1016/j.socscimed.2007.05.036
- Currie, J. 2009. Healthy, wealthy, and wise: Socioeconomic status, poor health in childhood, and human capital development. Journal of Economic Literature 47(1):87–122. https://doi.org/10.1257/jel.47.1.87
- Cutler, D. M., and A. Lleras-Muney. 2010. Understanding differences in health behaviors by education. Journal of Health Economics 29(1):1–28. https://doi.org/10.1016/j.jhealeco.2009.10.003
- DeNavas-Walt, C., B. D. Proctor, and J. C. Smith. 2013. Income, poverty, and health insurance coverage in the United States: Current population reports. U.S. Department of Commerce, Economics and Statistics Administration, U.S. Census Bureau. September. Available at: http://www.census.gov/hhes/www/hlthins/ (accessed May 23, 2014).
- Denhem, S. A. 2006. Social-emotional competence as support for school readiness: What is it and how do we assess it? Early Education and Development 17(1):57–89. https://doi.org/10.1207/s15566935eed1701_4
- Duncan, G. J., J. Brooks-Gunn, and P. K. Klebanov. 1994. Economic deprivation and early childhood development. Child Development 65:296–318. https://doi.org/10.2307/1131385
- Eide, R. E., and M. H. Showalter. 2011. Estimating the relation between health and education: What do we know and what do we need to know? Economics of Education Review 30(5):778–791. Available at: http://www.sciencedirect.com/science/article/pii/S0272775711000525 (accessed May 28, 2020).
- Estabrooks, P. A., R. E. Lee, and N. C. Gyurcsik. 2003. Resources for physical activity participation: Does availability and accessibility differ by neighborhood socioeconomic status? Annals of Behavioral Medicine 25(2):100–104. https://doi.org/10.1207/S15324796ABM2502_05
- Evans, B. F., E. Zimmerman, S. H. Woolf, and A. D. Haley. 2012. Social determinants of health and crime in post-Katrina Orleans Parish. Richmond: Virginia Commonwealth University Center on Human Needs.
- Evans, G. W., J. Brooks-Gunn, and P. K. Klebanov. 2011. Stressing out the poor: Chronic physiological stress and the income-achievement gap. Community Investments 23(2):22–27. Available at: https://inequality.stanford.edu/sites/default/files/PathwaysWinter11_Evans.pdf (accessed May 28, 2020).
- Evans, G. W., and P. Kim. 2010. Multiple risk exposure as a potential explanatory mechanism for the socioeconomic status-health gradient. Annals of the New York Academy of Sciences 186(1):174–189. https://doi.org/10.1111/j.1749-6632.2009.05336.x
- Felitti, V. J., R. F. Anda, D. Nordenberg, D. F. Williamson, A. M.Spitz, V. Edwards, M. P. Koss, and J. S. Marks. 1998. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The Adverse Childhood Experiences (ACE) study. American Journal of Preventive Medicine 14(4):245–258. https://doi.org/10.1016/s0749-3797(98)00017-8
- Freeman, J. D., S. Kadiyala, J. F. Bell, and D. P. Martin. 2008. The causal effect of health insurance on utilization and outcomes in adults: A systematic review of U.S. studies. Medical Care 46(10):1023–1032. https://doi.org/10.1097/MLR.0b013e318185c913
- Gan, L., and G. Gong. 2007. Estimating interdependence between health and education in a dynamic model. NBER Working Paper No. 12830, Cambridge, MA. Available at: http://www.nber.org/papers/w12830 (accessed April 2, 2014).
- Garrett, B. E., S. R. Dube, C. Winder, and R. S. Caraballo. 2013. Cigarette smoking—United States, 2006–2008 and 2009–2010. DC health disparities and inequalities report—United States, 2013. Centers for Disease Control. Morbidity and Mortality Weekly Report 62(3):81–84. Available at: http://www.cdc.gov/mmwr/pdf/other/su6203.pdf (accessed February 7, 2014).
- Gaston, G. B. 2013. African-Americans’ perceptions of health care provider cultural competence that promote HIV medical self-care and antiretroviral medication adherence. AIDS Care 25(9):1159–1165.
Available at: http://www.tandfonline.com/doi/abs/10.1080/09540121.2012.752783#preview (accessed, May 23, 2014). - Goldman, D., and J. P. Smith. 2011. The increasing value of education to health. Social Science and Medicine 72:1728–1737. https://doi.org/10.1016/j.socscimed.2011.02.047
- Gottesman, I. I., and D. R. Hanson. 2005. Human development: Biological and genetic processes. Annual Review of Psychology 56:263-286. https://doi.org/10.1146/annurev.psych.56.091103.070208
- Greenwald, R., L. V. Hedges, and R. D. Laine. 1996. The effect of school resources on student achievement. Review of Educational Research 66(3):361–396. https://doi.org/10.2307/1170528
- Grimm, K. A., L. V. Moore, and K. S. Scanlon. 2013. Access to health food retailers—Unites States, 2011. CDC health disparities and inequalities report—United States, 2013. Centers for Disease Control. Morbidity and Mortality Weekly Report 62(3):20–26. Available at: http://www.cdc.gov/mmwr/pdf/other/su6203.pdf (accessed February 7, 2014).
- Guo, G. 1998. The timing of influences of cumulative poverty on children’s cognitive ability and achievement. Social Forces 77(1):257–287. https://doi.org/10.2307/3006017
- Hackman, D. A., M. J. Farah, and M. J. Meaney. 2010. Socioeconomic status and the brain: Mechanistic insights from human and animal research. Nature Reviews Neuroscience 11: 651-659. https://doi.org/10.1038/nrn2897
- Hadley, J. 2003. Sicker and poorer—the consequences of being uninsured: A review of the research on the relationship between health insurance, medical care use, health, work, and income. Medical Care Research and Review 60(Suppl. 2):S3–S75. https://doi.org/10.1177/1077558703254101
- Heckman, J. J. 2006. Skill formation and the economics of investing in disadvantaged children. Science 312:1900–1902. Available at: http://jenni.uchicago.edu/papers/Heckman_Science_v312_2006.pdf (accessed May 28, 2020).
- Heckman, J. J., and T. Kautz. 2012. Hard evidence on soft skills. Labour Economics 19:451–464. https://doi.org/10.1016/j.labeco.2012.05.014
- HHS (Health and Human Services). 1998. Council on graduate medical education tenth report: Physician distribution and health care challenges in rural and inner-city areas. Public Health Service, Health Resources and Services Administration. Available at: http://www.hrsa.gov/advisorycommittees/bhpradvisory/cogme/Reports/tenthreport.pdf (accessed February 14, 2014).
- HHS. 2013. National healthcare quality report 2012. Agency for Healthcare Research and Quality, Rockville, MD. Available at: http://www.ahrq.gov/research/findings/nhqrdr/nhqr12/nhqr12_prov.pdf (accessed February 14, 2014).
- Institute of Medicine. 2000. Promoting Health: Intervention Strategies from Social and Behavioral Research. Washington, DC: The National Academies Press. https://doi.org/10.17226/9939
- Institute of Medicine. 2003. Hidden Costs, Value Lost: Uninsurance in America. Washington, DC: The National Academies Press. https://doi.org/10.17226/10719
- Institute of Medicine. 2003. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: The National Academies Press. https://doi.org/10.17226/12875
- Jemal, A., E. Ward, R. N. Anderson, T. Murray, and M. J. Thun. 2008. Widening of socioeconomic inequalities in U.S. death rates, 1993–2001. PLoS ONE 3(5):1–8. https://doi.org/10.1371/journal.pone.0002181
-
National Research Council. 1990. Inner-City Poverty in the United States. Washington, DC: The National Academies Press. https://doi.org/10.17226/1539
- Julian, T. A., and R. A. Kominski. 2011. Education and synthetic work-life earnings estimates. American Community Survey Reports, ACS-14. U.S. Census Bureau, Washington, DC. Available at: https://www.census.gov/library/publications/2011/acs/acs-14.html (accessed May 28, 2020).
- Kanny, D., Y. Liu, R. D. Brewer, and H. Lu. 2013. Binge drinking–United States, 2011. CDC health disparities and inequalities report—United States, 2013. Centers for Disease Control. Morbidity and Mortality Weekly Report 62(3):77–80. Available at: http://www.cdc.gov/mmwr/pdf/other/su6203.pdf (accessed February 7, 2014).
- Kant, A. K., and B. I. Graubard. 2007. Secular trends in the association of socio-economic position with self-reported dietary attributes and biomarkers in the U.S. population: National Health and Nutrition Examination Survey (NHANES) 1971–1975 to NHANES 1999–2002. Public Health Nutrition 10(2):158–167. https://doi.org/10.1093/ajcn/84.5.1215
- Kaplan, G. A., T. W. Wilson, R. D. Cohen, J. Kauhanen, M. Wu, and J. T. Salonen. 1994. Social functioning and overall mortality: Prospective evidence from the Kuopio Ischemic Heart Disease Risk Factor Study. Epidemiology 5(5):495–500. Available at: https://pubmed.ncbi.nlm.nih.gov/7986863/ (accessed May 28, 2020).
- Karlamangla, A. S., H. S. Burton, and T. E. Seeman. 2006. Reduction in allostatic load in older adults is associated with lower all-cause mortality risk: MacArthur studies of successful aging. Psychosomatic Medicine 68:500–507. https://doi.org/10.1097/01.psy.0000221270.93985.82
- Kawachi, I., and L. F. Berkman. 2003. Neighborhoods and health. New York: Oxford University Press.
- Kawachi, I., and S. V. Subramanian. 2007. Neighbourhood influences on health. Journal of Epidemiology and Community Health 61(1):3–4. https://doi.org/10.1136/jech.2005.045203
- Kawachi, I., S. Takao, and S. V. Subramanian, eds. 2013. Global perspectives on social capital and health. New York: Springer.
- Krueger, P. M., and V. Chang. 2008. Being poor and coping with stress: Health behaviors and the risk of death. American Journal of Public Health 98:889–896. https://doi.org/10.2105/AJPH.2007.114454
- Kulkarni, S. C., A. Levin-Rector, M. Ezzati, and C. J. Murray. 2011. Falling behind: life expectancy in U.S. counties from 2000 to 2007 in an international context. Population Health Metrics 9(1):16. https://doi.org/10.1186/1478-7954-9-16
- Leventhal, T., and J. Brooks-Gunn. 2000. The neighborhood they live in: The effects of neighborhood residence on child and adolescent outcomes. Psychological Bulletin 126(2):309–337. https://doi.org/10.1037/0033-2909.126.2.309
- Link, B. G., and J. Phelan. 1995. Social conditions as fundamental causes of disease. Journal of Health and Social Behavior 36:80–94. https://doi.org/10.1177/0022146510383498
- Maas, J., R. A., Verheij, P. P. Groenewegan, S. de Vries, and P. Spreeuwenberg. 2006 Green space, urbanity, and health: How strong is the relation? Journal of Epidemiology and Community Health 60:587–592. https://doi.org/10.1136/jech.2005.043125
- Macintyre, S., and A. Ellaway A. 2003. Neighborhoods and health: An overview. In Neighborhoods and health, edited by I. Kawachi and L. F. Berkman. New York: Oxford University Press. Pp. 20–42.
- Maitra, S. 2010. Can patient self-management explain the health gradient? Goldman and Smith’s “Can patient self-management help explain the SES health gradient?” (2002) revisited. Social Science and Medicine 70:802–812. https://doi.org/10.1016/j.socscimed.2009.08.043
- Massey, D. S., and N. A. Denton. 1993. American apartheid: Segregation and the making of the underclass. Cambridge, MA: Harvard University Press.
- Mayer, S. E., and C. Jencks. 1989. Growing up in poor neighborhoods: How much does it matter? Science 243(4897):1441–1445. https://doi.org/10.1126/science.243.4897.1441
- McEwen, B.S. 2012. Brain on stress: How the social environment gets under the skin. Proceedings of the National Academy of Sciences 109(2):17180-17185. https://doi.org/10.1073/pnas.1121254109
- McEwen, B. S., and E. Stellar. 1993. Stress and the individual: Mechanisms leading to disease. Archives of Internal Medicine 153(18):2093–2101. Available at: https://pubmed.ncbi.nlm.nih.gov/8379800/ (accessed May 28, 2020).
- Mirowsky, J., and C. E. Ross. 2005. Education, learned effectiveness and health. London Review of Education 3(3):205–220. Available at: https://eric.ed.gov/?id=EJ821180 (accessed May 28, 2020).
- Mistry K. B., C. S. Minkovitz, A. W. Riley, S. B. Johnson, H. A. Grason, L. C. Dubay, and B. Guyer.. 2012. A new framework for childhood health promotion: the role of policies and programs in building capacity and foundations of early childhood health. American Journal of Public Health 102: 1688-1696. https://doi.org/10.2105/AJPH.2012.300687
- Mokdad, A. H., J. S. Marks, D. F. Stroup, and J. L. Gerberdin. 2004. Actual causes of death in the United States 2000. Journal of American Medical Association 291(10):1238–1245. https://doi.org/10.1001/jama.291.10.1238
- Montez, J. K., and L. F. Berkman. 2014. Trends in the educational gradient of mortality among U.S. adults aged 45 to 84 years: Bringing regional context into the explanation. American Journal of Public Health 104(1):e82–e90. https://doi.org/10.2105/AJPH.2013.301526
- Montez, J. K., R. A. Hummer, and M. D. Hayward. 2012. Educational attainment and adult mortality in the United States: A systematic assessment of functional form. Demography 45:315–336. https://doi.org/10.1007/s13524-011-0082-8
- Institute of Medicine. 2009. America’s Uninsured Crisis: Consequences for Health and Health Care. Washington, DC: The National Academies Press. https://doi.org/10.17226/12511
- Institute of Medicine and National Research Council. 2000. From Neurons to Neighborhoods: The Science of Early Childhood Development. Washington, DC: The National Academies Press. https://doi.org/10.17226/9824
- Institute of Medicine and National Research Council. 2013. U.S. Health in International Perspective: Shorter Lives, Poorer Health. Washington, DC: The National Academies Press. https://doi.org/10.17226/13497
- O’Campo, P., and J. R. Dunn, eds. 2011. Rethinking social epidemiology. Dordrecht: Springer. Available at: http://www.cdc.gov/nchs/data/databriefs/db82.pdf (accessed May 23, 2014).
- Olshansky, S. J., T. Atonucci, L. Berkman, R. H. Binstock, A. Boersch-Supan, J. T. Cacioppo, B. A. Carnes, L. L. Carstensen, L. P. Fried, D. P. Goldman, J. Jackson, M. Kohli, J. Rother, Y. Zheng, and J. Rowe. 2012. Differences in life expectancy due to race and educational differences are widening, and many may not catch up. Health Affairs 31:1803-1813. https://doi.org/10.1377/hlthaff.2011.0746
- Pampel, F. C., P. M. Krueger, and J. T. Denney. 2010. Socioeconomic disparities in health behaviors. Annual Review of Sociology 36:349–370. https://doi.org/10.1146/annurev.soc.012809.102529
- Pearlin, L. I. 1989. The sociological study of stress. Journal of Health and Social Behavior 30(3):241–256. https://doi.org/10.2307/2136956
- Powell, L. M., S. Slater, F. J. Chaloupka, and D. Harper. 2006. Availability of physical activity-related facilities and neighborhood demographic and socioeconomic characteristics: A national study. American Journal of Public Health 96:1676–1680. https://doi.org/10.2105/AJPH.2005.065573
- Pridmore, P. 2007. Impact of health on education access and achievement: A cross-national review of the research evidence. Create Pathways to Access Research Monograph No. 2. Consortium for Research on Educational Access, Transitions and Equity. Institute of Education, University of London. Available at: http://files.eric.ed.gov/fulltext/ED508614.pdf (accessed April 29, 2014).
- Rhodes, T., K Wagner, S. A. Strathdee, K. Shannon, P. Davidson, and P. Bourgois. 2011. Structural violence and structural vulnerability within the risk environment: Theoretical and methodological perspectives for a social epidemiology of HIV risk among injection drug users and sex workers. In Rethinking social epidemiology, edited by P. O’Campo and J. R. Dunn. Dordrecht: Springer. Pp 205–230.
- Ridgeway, C. L. 2014. Why status matters for inequality. American Sociological Review 79(1):1–16. Available at: https://www.asanet.org/sites/default/files/savvy/journals/ASR/Feb14ASRFeature.pdf (accessed May 28, 2020).
- Roberts, B. W., N. R. Kuncel, R. Shiner, A. Caspi, and L. R. Goldberg. 2007. The power of personality: The comparative validity of personality traits, socioeconomic status, and cognitive ability for predicting important life outcomes. Perspectives on Psychological Science 2(4):313–345. https://doi.org/10.1111/j.1745-6916.2007.00047.x
- Rosas-Salazar, C., A. J. Apter, G. Canino, and J. C. Celedon. 2008. Neighborhood socioeconomic status and health: Context or composition? City and Community 7(2):163–179. https://doi.org/10.1111/j.1540-6040.2008.00251.x
- Rosas-Salazar, C., A. J. Apter, G. Canino, and J. C. Celedon. 2012. Health literacy and asthma. Journal of Allergy and Clinical Immunology 129(4):935–942. https://doi.org/10.1016/j.jaci.2012.01.040
- Ross, C. E., and C. L. Wu. 1995. The links between education and health. American Sociological Review 60(5):719–745. https://doi.org/10.2307/2096319
- Saez, E. 2013. Striking it richer: The evolution of top incomes in the United States (updated with 2012 preliminary estimates). Available at: http://elsa.berkeley.edu/~saez/saez-UStopincomes-2012.pdf (accessed May 23, 2014).
- Sampson, R. J. 2003. Neighborhood-level context and health: Lessons from sociology. In Neighborhoods and health, edited by I. Kawachi and L. F. Berkman. New York: Oxford University Press. Pp. 132–146.
- Sandstrom, H., and S. Huerta. 2013. The negative effects of instability on child development: A research synthesis. Low-Income Working Families Discussion Paper 3. Washington, DC: Urban Institute. Available at: https://www.urban.org/sites/default/files/publication/32706/412899-The-Negative-Effects-of-Instability-on-Child-Development-A-Research-Synthesis.PDF (accessed May 28, 2020).
- Seeman, T. E. 1996. Social ties and health: The benefits of social integration. Annals of Epidemiology 6(5):442–451. https://doi.org/10.1016/s1047-2797(96)00095-6
- Seeman, T. E., B. H. Singer, J. W. Rowe, R. I. Horwitz, and B. S. McEwen. 1997. Price of adaptation: Allostatic load and its health consequences. Archives of Internal Medicine 157:2259–2268. Available at: https://pubmed.ncbi.nlm.nih.gov/9343003/ (accessed May 28, 2020).
- Shankardass, K., and J. R. Dunn. 2011. How goes the neighbourhood? Rethinking neighbourhoods and health research in social epidemiology. In Rethinking social epidemiology, edited by P. O’Campo and J. R. Dunn. Dordrecht: Springer. Pp 137–156.
- Shippee, T. P., L. R. Wilkinson, and K. F. Ferraro. 2012. Accumulated financial strain and women’s health over three decades. Journals of Gerontology Series B: Psychological Sciences and Social Sciences I 67(5):585–594, https://doi.org/10.1093/geronb/gbs056
- Shonkoff, J. P., and A. S. Garner. 2012. The lifelong effects of early childhood toxic stress. Pediatrics 129(1):e232–e246. https://doi.org/10.1542/peds.2011-2663
- Shonkoff J. P., W. T. Boyce, and B. S. McEwen. 2009. Neuroscience, molecular biology, and the childhood roots of health disparities: building a new framework for health promotion and disease prevention. JAMA 301(21): 2252-2259. https://doi.org/10.1001/jama.2009.754
- Smith, K. P., and N. A. Christakis. 2008. Social networks and health. Annual Review of Sociology 34:405–429. Available at: http://www.pinniped.net/smith2008.pdf (accessed May 28, 2020).
- Spence, M., and S. Hlatshwayo. 2011. The evolving structure of the American economy and the employment challenge. New York: Council on Foreign Relations. Available at: http://www.cfr.org/industrialpolicy/evolving-structure-american-economy-employment-challenge/p24366 (accessed April 9, 2014).
- Stafford, M., T. Chandola, and M. Marmot. 2007. Association between fear of crime and mental health and physical functioning. American Journal of Public Health 97:2076–2081. https://doi.org/10.2105/AJPH.2006.097154
- Steptoe, A., and P. J. Feldman. 2001. Neighborhood problems as sources of chronic stress: Development of a measure of neighborhood problems and associations with socioeconomic status and health. Annals of Behavioral Medicine 23:177–185. https://doi.org/10.1207/S15324796ABM2303_5
- Sum, A., I. Khatiwada, J. McLaughlin, and S. Palma. 2009. The consequences of dropping out of high school: Joblessness and jailing for high school dropouts and the high cost for taxpayers. Boston: Center for Labor Market Studies, Northeastern University. Available at: https://www.issuelab.org/resource/the-consequences-of-dropping-out-of-high-school-joblessness-and-jailing-for-high-school-dropouts-and-the-high-cost-for-taxpayers.html (accessed May 28, 2020).
- Taras, H., and W. Potts-Datema. 2005. Chronic health conditions may also impact children’s development and educational performance. Journal of School Health 75(7):255–266. https://doi.org/10.1111/j.1746-1561.2005.00034.x
- Thoits, P. A. 2010. Stress and health: Major findings and policy implications. Journal of Health and Social Behavior 51(Suppl.):S41–S53. https://doi.org/10.1177/0022146510383499
- University of Wisconsin Population Health Institute. County Health Rankings 2013. Available at: www.countyhealthrankings.org (accessed June 3, 2014).
- U.S. Census Bureau. 2012. American Community Survey, 2009–2011. Detailed tables using American FactFinder. Available at: http://factfinder.census.gov/home (accessed December 12, 2012).
- U.S. Census Bureau. 2013. Public education finances: 2011. G11-ASPEF. Washington, DC: Government Printing Office. Available at: https://www2.census.gov/govs/school/11f33pub.pdf (accessed May 28, 2020).
- Weisleder, A., and A. Fernald. 2013. Talking to Children Matters: Early language experience strengthens processing and builds vocabulary. Psychological Science 24(11):2143–2152. https://doi.org/10.1177/0956797613488145
- Willems, S., S. De Maesschalck, M. Deveugele, A. Derese, and J. De Maeseneer. 2005. Socio-economic status of the patient and doctor-patient communication: Does it make a difference? Patient Education and Counseling 56:139–146. https://doi.org/10.1016/j.pec.2004.02.011
- Williams, D. R., and S. A. Mohammed. 2009. Discrimination and racial disparities in health: Evidence and needed research. Journal of Behavioral Medicine 32(1):20–47. https://doi.org/10.1007/s10865-008-9185-0
- Williams Shanks, T. R., and C. Robinson. 2013. Assets, economic opportunity and toxic stress: A framework for understanding child and educational outcomes. Economics of Education Review 33:154–170. Available at: http://www.sciencedirect.com/science/article/pii/S0272775712001458 (accessed June 3, 2014).
- Wilson, J. W. 1987. The truly disadvantaged: The inner city, the underclass, and public policy. Chicago: University of Chicago Press.
- Winkleby, M., C. Cubbin, and D. Ahn. 2006. Effect of cross-level interaction between individual and neighborhood socioeconomic status on adult mortality rates. American Journal of Public Health 96:2145–2153. https://doi.org/10.2105/AJPH.2004.060970
- Zhang, T. Y. and M. J. Meaney. 2010. Epigenetics and the environmental regulation of the genome and its function. Annual Review of Psychology 61:439-466. https://doi.org/10.1146/annurev.psych.60.110707.163625