Social Networking Sites and the Continuously Learning Health System: A Survey
Background
The use of social networking sites (SNSs) is widespread. As of December 2012, 67 percent of American adults with Internet access used some form of social media, and 59 percent of them used the Internet to look for health-related information (Brenner, 2013; Fox and Duggan, 2013). Through SNSs such as Facebook and Twitter, individuals might share their health experiences, such as disease diagnoses or side effects of a drug, or participate in research studies (Ramo and Prochaska, 2012).
In addition to these general-use SNSs, Americans currently use a number of health-specific SNSs that permit them to connect and collaborate with other people with the same or similar health conditions (e.g., TuDiabetes for diabetes mellitus, PatientsLikeMe [PLM] for chronic conditions, or TheBody for HIV). On these sites, people share health-related information that can include blood glucose levels, mood, medication dosages, and related side effects (Wicks et al., 2012). A number of benefits have been reported by people who use health-related SNSs, including gaining a better understanding of their medical conditions, feeling in greater control of their disease management, and improving treatment adherence (IOM, 2012). Such systems also may provide less-tangible benefits, including reduced isolation, increased disease awareness, and the opportunity to harness advocacy movements for lobbying or fundraising. From a research perspective, the potential benefits could be significant, including
- the use of SNSs to survey patients on the conduct of more patient-centric clinical trials;
- the design of patient-reported outcome measures that matter to patients;
- a faster way for academic and public health researchers to conduct observational studies; and, perhaps,
- a mechanism for regulators to collect information on drug-related adverse events (Pearson, et al., 2011).
Today, in the United States, the majority of health data are stored on paper or in electronic health records at medical facilities that are covered by the Health Information Technology for Economic and Clinical Health (HITECH) Act and the Health Insurance Portability and Accountability Act (HIPAA), meaning that sensitive information, e.g., a diagnosis of bipolar disorder, is more likely to remain confidential and patients are kept informed of how such data are used. However, SNSs are not HIPAA-covered entities. Therefore, the same information when shared on an SNS does not have the same protection, and potentially may lead to discrimination by a future employer or health insurance agency, although this has not been reported in the literature to date. Furthermore, in sharing their own digital information, including health-related data, with friends and peers, patients may be unaware of the ways in which these data may be re-used by third parties, such as for targeted advertising or research for the pharmaceutical industry (Fernandez-Luque et al., 2009). This is problematic because online consumers seldom read end-user license agreements, and even people who are concerned about privacy invariably click “accept” when they encounter these legal contracts (Böhme et al., 2010). As companies’ business models adapt in generating revenue through marketing and advertising, they often change the terms of users’ contracts; users are informed of the changes with alerts, but these are often ignored (Forbes, 2012).
Two similar Web-based surveys were fielded from March 7 to March 19, 2012, and from September 1 to October 31, 2012, respectively. The first survey was fielded by a research arm of the Consumer Reports National Testing and Research Center (CRNRC), which is staffed by social scientists and is free of corporate influence and advertising. Research conducted by CRNRC cannot be commissioned or financed by third parties. The second survey was fielded by PLM, a for-profit social networking site aimed at making health care better for everyone through data sharing, peer support, and transparent research. PLM works with trusted government, nonprofit, research, and industry partners who use the site’s health data to improve products, services, and care for patients.
Findings
Both surveys queried respondents on their attitudes toward health-related data sharing and their current medical care. A total of 2,094 participants were invited by CRNRC, and 13,524 participants were invited by PLM. Both samples were recruited independently of each other. The CRNRC sample has been described previously (IOM, 2012).
The CRNRC and PLM survey questionnaires were constructed using a modified Delphi protocol (Okoli and Pawlowski, 2004). Using an iterative process, 30 experts from the CRNRC and the Evidence Communication Innovation Collaborative (ECIC) of the Institute of Medicine’s (IOM’s) Roundtable on Value & Science-Driven Health Care (VSRT) developed and tested the CRNRC instrument after ECIC completed a literature review. No changes were deemed necessary after testing. The PLM survey was based on the CRNRC instrument but adapted to include a number of extra measures specific to the PLM population (e.g., Internet users who have a chronic health condition). Given the unique identifier for both the CRNRC and PLM populations, it is highly unlikely that any participant completed the survey more than once. Participants were given the option to opt out of any survey question. (For more information, please refer to Appendix C.)
A total of 3,335 participants completed the surveys. CRNRC sampled 2,094 participants, of whom 1,210, or 57.8 percent, completed the survey. PLM sampled 13,324 users, of whom 2,890, or 21.7 percent, completed the survey. (The PLM sample also included non-American users; these were excluded from the data presented here.)
A summary of the results follows and can be found in Appendix B. The complete tables can be found in Appendix A.
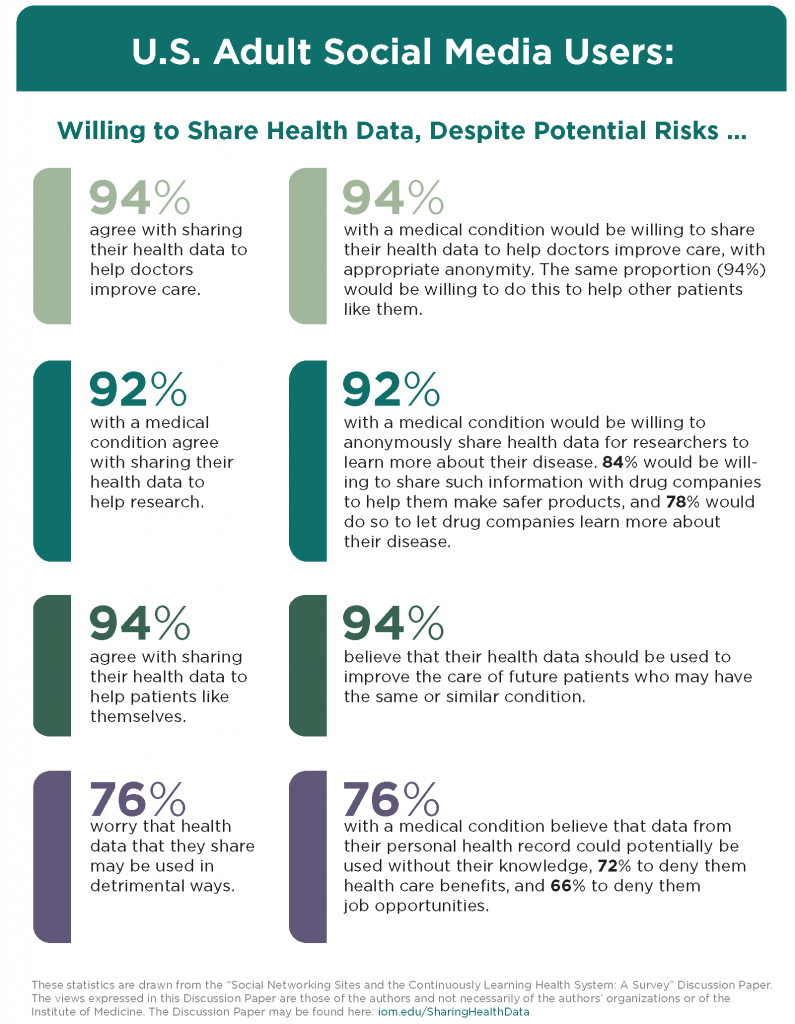
How Health Data Should Be Used
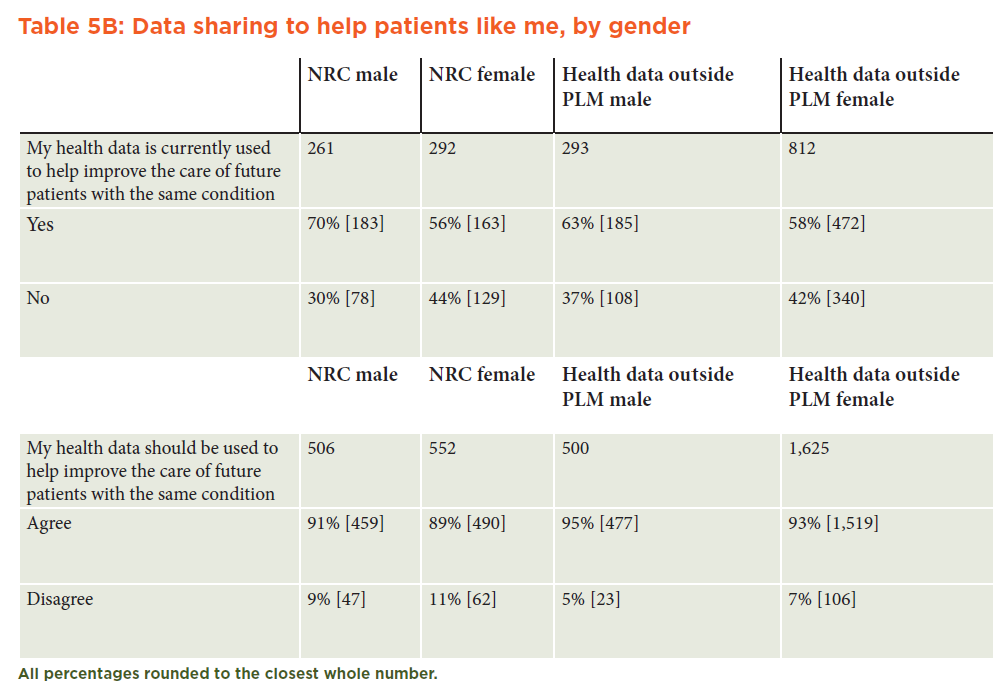
Most respondents believed that their data should be used to improve the care of future patients (CRNRC: 90 percent; PLM: 94 percent). A similar proportion of the CRNRC and PLM respondents believed that their routinely collected health data (outside an SNS context) were currently used to improve the care of future patients with the same (or similar) health conditions. However, a greater proportion of the PLM sample (91 percent) believed that the health data they shared through their health-centered SNSs were being used to improve care. (See Tables 5A and 5B in Appendix A.)
With Whom Data Should be Shared
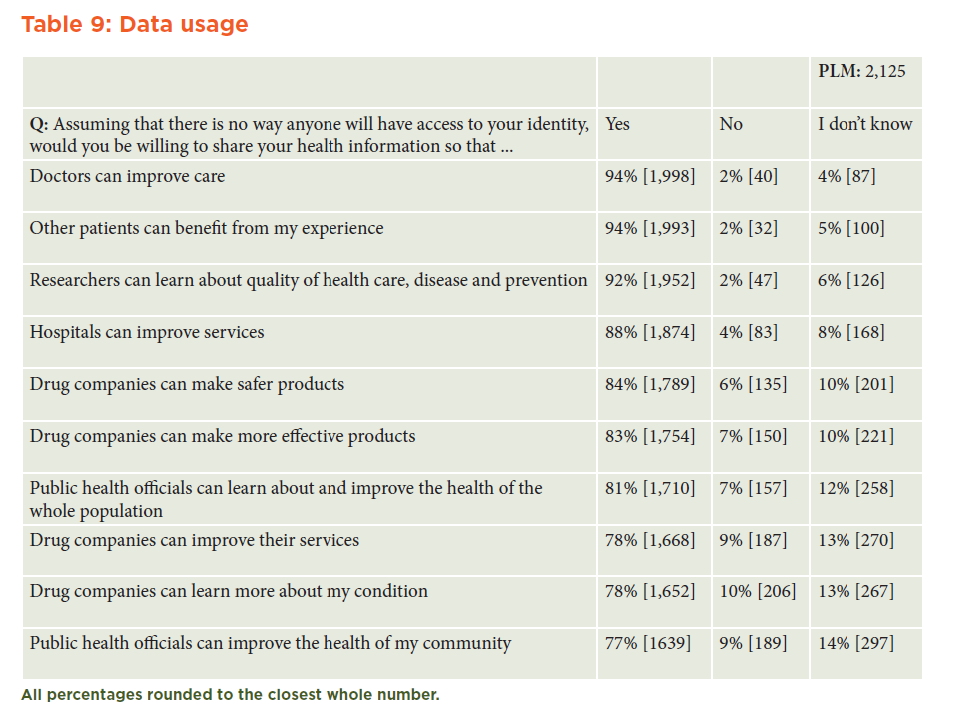
There was little difference in respondents’ perceptions of sharing data anonymously with public health officials (to improve community health) compared with sharing data with drug companies (to learn more about a patient’s condition). In general, at least 77 percent and as many as 94 percent of respondents were willing to share their health data for utilitarian purposes, regardless of the sharing party. (See Table 9 in Appendix A.)
Lingering Questions Among Patients
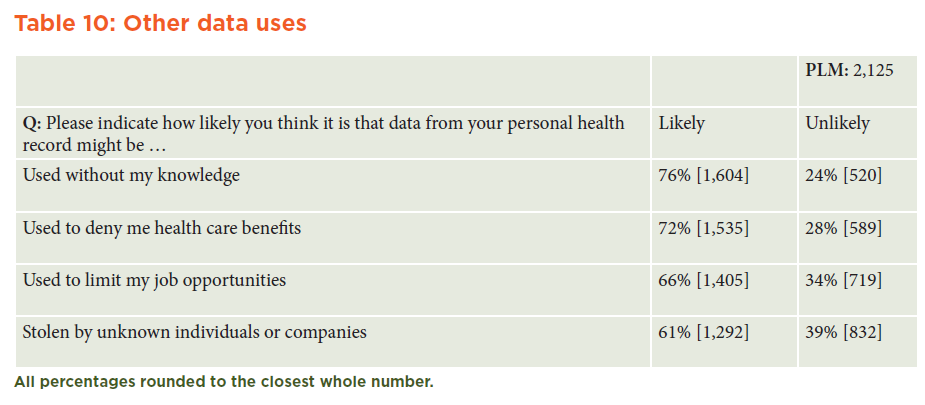
A majority of PLM respondents believed that it was likely or very likely that data from their personal health records might be used without their knowledge (76 percent), used to deny them health care benefits (72 percent), used to limit job opportunities (66 percent), or stolen by unknown individuals or companies (61 percent). (See Table 10 in Appendix A.)
Who Was Surveyed
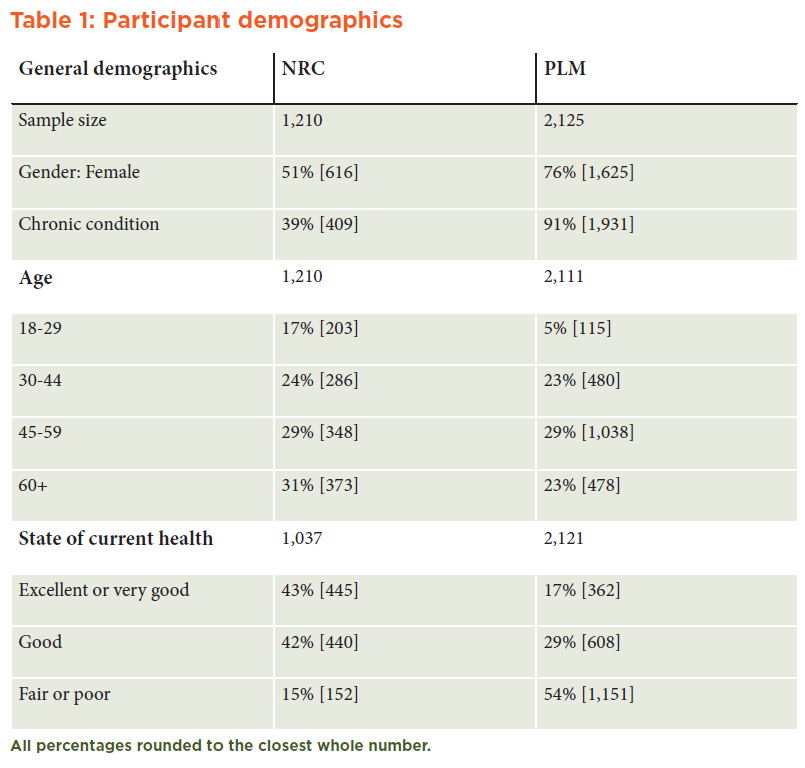
Although both samples are representative of U.S. adults, the CRNRC sample is more representative of the general American population, while the PLM sample is representative of Americans with chronic conditions. There were more CRNRC respondents in the older (60+) and younger (18-29) age categories compared with the PLM sample. In addition, the health status of the PLM respondents was disproportionately worse. (See Table 1 in Appendix A.)
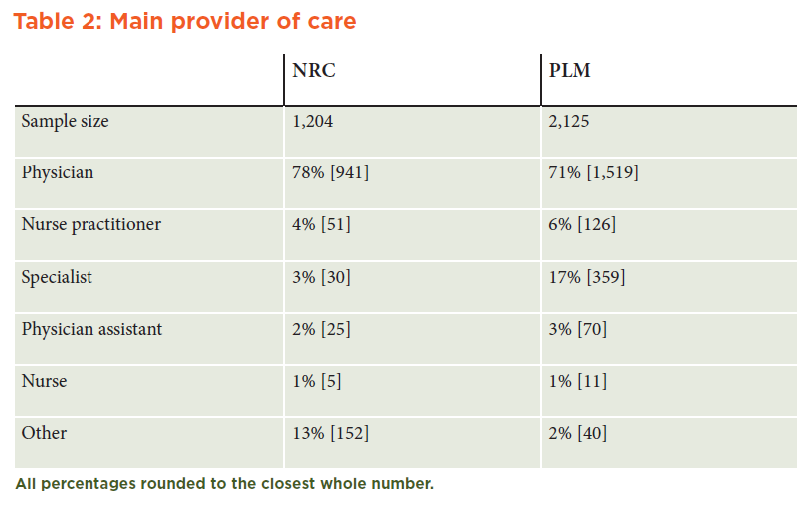
Who Provides Patients’ Care
Although the majority of both populations had a physician as their primary health care provider, the CRNRC sample had a greater proportion of “other” health care providers. These include naturopaths, the emergency room, walk in clinics, nutritionists, and chiropractors. The PLM sample had a greater proportion of specialists (17 percent vs. 3 percent in the CRNRC sample) as their main care provider, reflecting their specific health issues. (See Table 2 in Appendix A.)
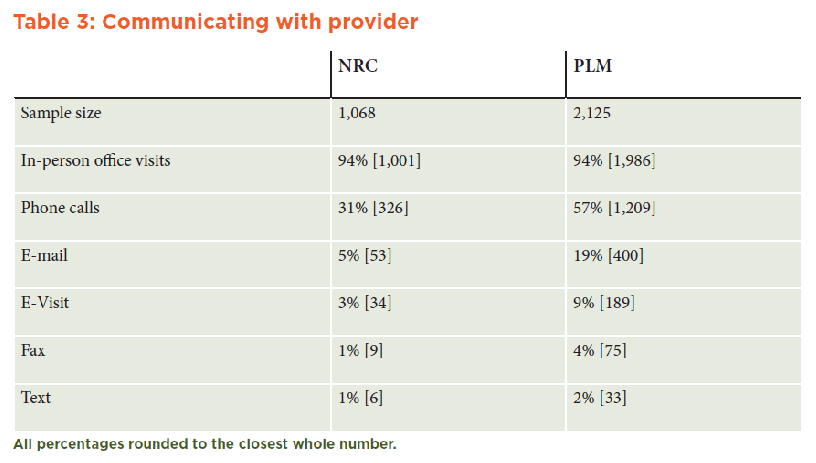
The Impact of Technology on Health
The data strongly suggest that the PLM user demographic is more comfortable with leveraging technology as part of their health care experience, and, thus, this demographic interacts with primary care providers more often via telephone calls (almost double the CRNRC rate), e-mail (almost four times the CRNRC rate), and e-visits. (See Table 3 in Appendix A.)
Patient Activity During Health Visits
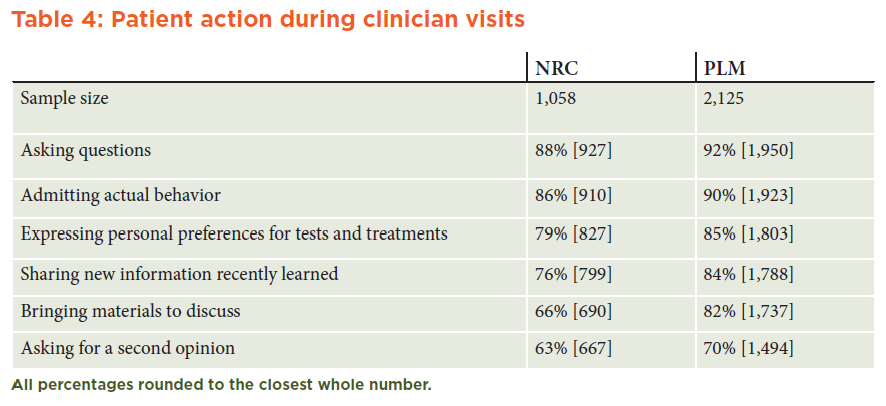
PLM users appeared more willing than the CRNRC sample to discuss new information, bring materials to visits, and express personal preferences about treatments. (See Table 4 in Appendix A.)
Patient Recognition of Team-Based Care
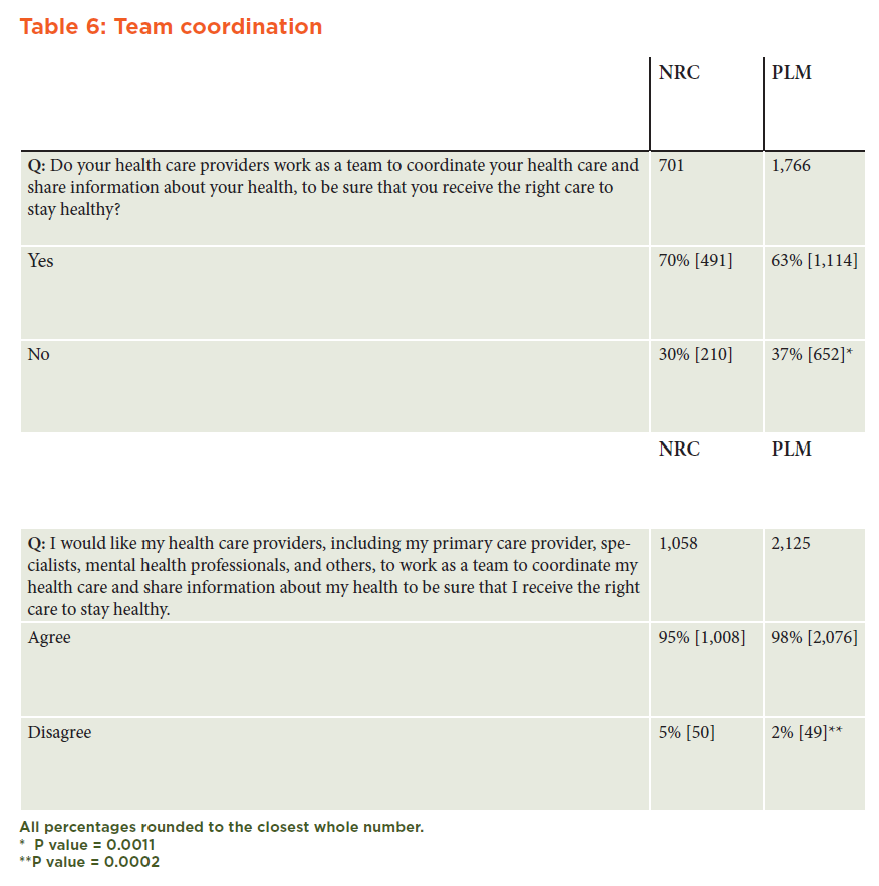
The proportion of respondents who believed that their care providers worked as a team to coordinate care was significantly greater in the CRNRC sample than in the PLM sample (CRNRC: 70 percent; PLM: 63 percent); and, conversely, the proportion of respondents who wanted their care providers to work as a team was significantly greater in the PLM group than in the CRNRC group (CRNRC: 95 percent; PLM: 98 percent). (See Table 6 in Appendix A.)
Rationale for Joining PLM
The highest proportion of PLM respondents wanted to compare their experiences with others (93 percent strongly or somewhat agreed) or share their experiences to benefit others (92 percent), rather than receive support from others (84 percent) or simply track their health over time (82 percent). (See Table 7 in Appendix A.)
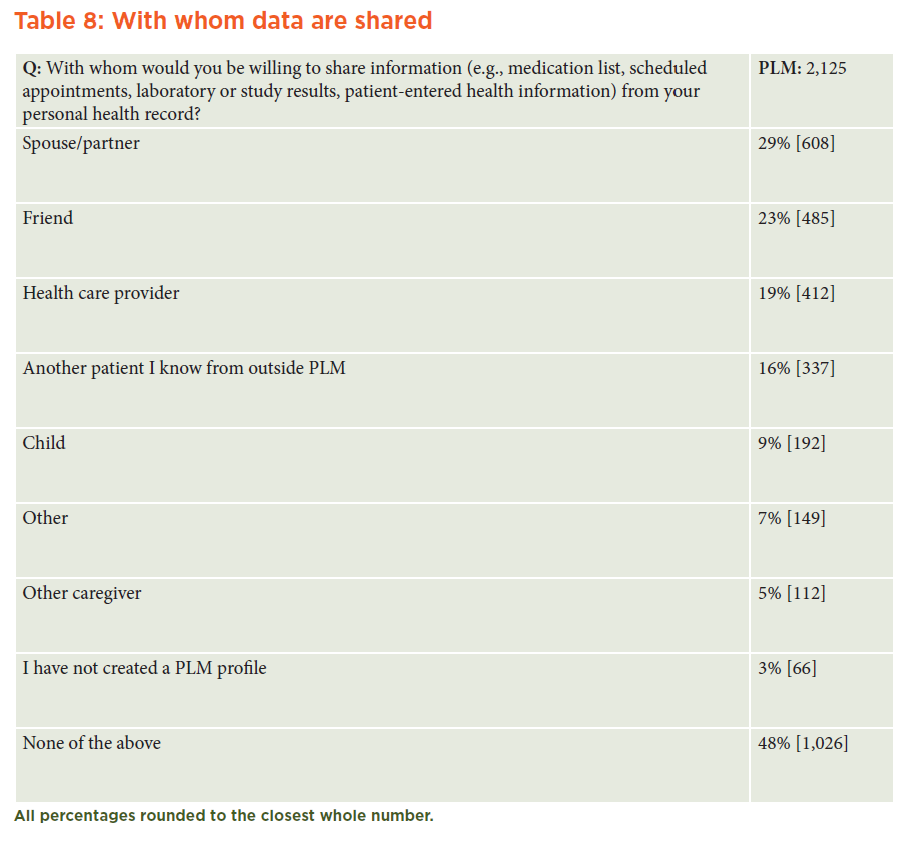
Patient Data Sharing Outside PLM
Although PLM respondents believed that their health data should be shared to help researchers and clinicians and to improve the care of future patients, most patients (52 percent) kept their own data within the confines of the PLM SNS. Only subsets shared their profiles with their spouses/partners (29 percent), health care providers (19 percent), friends (23 percent), or other patients outside PLM (16 percent). (See Table 8 in Appendix A.)
A Commitment to Data Sharing, Accompanied by Concerns
Our findings revealed that PLM respondents want their health data to be shared for utilitarian purposes, as long as anonymity is maintained. Despite this, a majority of PLM respondents believed that their PHR data were likely to be used without their knowledge or used against them to deny them health care benefits or limit job opportunities. To date, however, there have been no reports of such use occurring, and the provision in the Patient Protection and Affordable Care Act (ACA) that patients cannot be denied health coverage due to pre-existing conditions should alleviate lingering concerns about losing health benefits. These findings are aligned with a recent study (Agaku et al., 2013) that found that 64.5 percent of U.S. adults were concerned about electronic data breaches. Although people want their health data shared with researchers or patients, this does not mean that they are willing for their data to be posted publicly, as almost 48 percent of the PLM respondents did not share their PLM profiles with people outside the site.
Privacy Concerns Related to SNSs
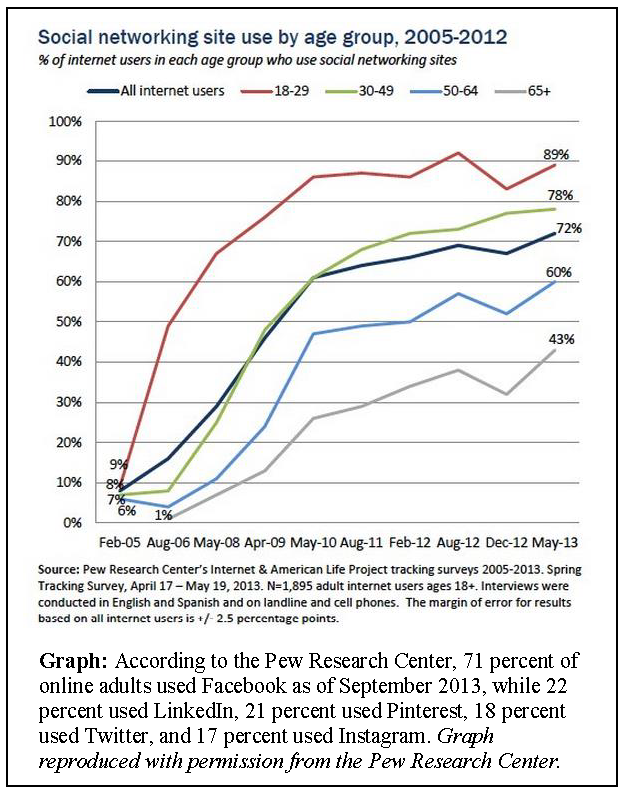
The use of SNSs is now almost ubiquitous in the United States, according to the Pew Research Center. About 73 percent of online adults use social networking sites, with SNS popularity cutting across all income levels. What’s more, 40 percent of mobile phone users access a SNS site via their phones, especially young people, African Americans, Latinos, the highly educated, and those with higher annual household incomes. From February 2005 to May 2013, the use of social networking sites among Internet users aged 18 to 29 experienced the most dramatic growth, rising from 9 to 89 percent (Brenner, 2013). The growth and adoption rates of SNS use, however, have outpaced policy changes designed to protect the interests of users (Solberg, 2012). Privacy, in an operational sense, can be defined as “contextual integrity” (Nissenbaum, 2004) and can be understood as matching the expectations of the information owner, so that information is only seen or used by intended parties. The companies that develop SNSs, in general, are for-profit entities that require users to accept license agreements prior to using SNS services. The terms of these agreements can only be changed by SNS companies, not by users. The data shared on an SNS site, both retrospectively and prospectively, suddenly may become a “digital tattoo” (Angwin and Stecklow, 2010; Walters, 2013) that is almost impossible to remove. Thus, data protection policies in the near future must evaluate the delicate balance of a free and democratic society that supports the sales of goods and services (based on a user’s data) while at the same time protecting people from discrimination.
In research, institutional review boards (IRBs) historically have deemed SNSs to be private spaces and have mandated that researchers inform potential subjects and acquire their consent prior to data collection (O’Connor, 2013). A marketing company or marketer may, however, pose as a member of an online community and receive no reprimand for violating user privacy, even if they are using the data for research or commercial purposes (Angwin and Stecklow, 2010).
Protecting Data Shared on SNSs
Previous work by VSRT (IOM, 2013) has underscored the potential value of linking large volumes of clinical and nonclinical data sources with electronic health records to optimize health care delivery and foster a continuously learning health care system. Our findings not only align with this work but also show that both the general public and Americans with health conditions want their data used to improve delivery both vertically and horizontally across health care stakeholders. Together, these linked data have the potential to improve disease surveillance and response, improve the focus of health care delivery, support improved decision making, prevent costly errors, and accelerate medical research discoveries.
A recent review published by the Journal of Law, Medicine and Ethics (O’Connor, 2013) affirms that social media has changed the paradigm from an intermediated world (in which the researcher who uses the data has control over the user or research subject) to an apomediated world. Apomediation refers to a flat system, in which the researcher and the data owner are on the same hierarchical level, are interdependent, and work in a peer-to-peer manner (Eysenbach, 2008). If, indeed, it is increasingly difficult to differentiate between researchers and subjects, what regulations should govern social media researchers (or third-party data users)?
Today, there is a gap in how health data are protected in the United States. Electronic patient records, such as those held by clinicians, are protected by HIPAA and HITECH. However, when people choose to share their information in order to improve how they manage their health conditions or find social support, they may not be protected and may be discriminated against by third parties. On May 21, 2008, President George W. Bush signed into law the Genetic Information Nondiscrimination Act (GINA) (NIH, 2008), which protects an individual’s genetic tests, those of family members, and the family’s medical history from being used in discriminatory ways. GINA raises the question of whether we, as a society, have a responsibility to similarly protect health-related data shared on SNSs. If so, what are the respective legal boundaries that must be in place to draft such legislation in Congress?
Future research should assess the actual vs. perceived risk of discrimination due to health-related data sharing on SNSs. Evaluating whether there is an association between universal health care coverage (e.g., the Canadian or British systems) and public perceptions about data sharing would shed light on the generalizability of results across geographical boundaries. Appraising participants’ responses against how much data they actually share on sites like PLM also would provide insight as to the validity of the survey findings. Questerviews, a technique that uses tape recordings to collect data about a questionnaire while participants are completing it, would provide qualitative context to people’s attitudes on data sharing and the justifications for their responses (Adamson et al., 2004). Finally, understanding public opinion and beliefs about the nature of anonymized vs. de-identified data would help policy makers draft legislation to protect the common good.
Conclusion
The Americans who participated in the CRNRC and PLM surveys, whether sick or healthy, want their data shared anonymously to improve the health of patients like themselves and to assist clinicians and researchers in improving health care delivery. However, their commitment to data sharing is accompanied by worry. They fear that the data they currently share could be used in detrimental ways, such as to deny them future job opportunities or health care coverage, although this last concern has been neutralized by passage of the ACA.
The data presented here provide a foundation for decision makers to evaluate current data use and access policies and align them with the views of the American population. However, much work remains to be done in order to implement policies that foster the delicate balance of a free and democratic society and support the sale of goods and services based on a user’s data, while simultaneously preventing harm.
We envision a health system defined by continuous learning that shares data between and across stakeholders to improve health care delivery. In this system, data use policies would align with patients’ privacy expectations. Moving forward, the engagement and collaboration of decision makers, policy makers, patients, clinicians, and the private sector will be crucial in ensuring that data sharing becomes the standard in the delivery of care for all.
Appendix A
Appendix B
Appendix C
IRB/Informed Consent/Data Protection
IRB approval was not sought for the fielding of this research; participation conveyed minimal risk. Additionally, all data were de-identified prior to analysis. Membership in both the Knowledge Panel, CRNRC’s software platform, and PatientsLikeMe is subject to voluntary research participation. Prior to undertaking the survey, all research participants provided informed consent and were briefed on their right to opt out of the survey during any point in the data collection process.
Participants and Recruitment
Both CRNRC and PLM utilized a closed-loop recruitment system in which a Web-based alert was sent to preselected candidates inviting them to participate in the survey. CRNRC participants were recruited from the KnowledgePanel® and KnowledgePanelLatino® probabilistic-sampling platforms (DiSogra, 2010; Agaku, et al., 2013), which are representative of U.S. adults. To become a member of this CRNRC platform, eligible subjects were recruited via stratified postal sampling and through random-digit telephone dialing. CRNRC subjects without Internet connectivity or computers were provided laptop computers with Internet access. The inclusion criteria for the CRNRC sample were non-institutionalized U.S. residents older than 18.
PLM is the world’s third-largest Patient Powered Research Network (PCORI, 2013). The site recruits patients with health conditions such as amyotrophic lateral sclerosis, diabetes, epilepsy, fibromyalgia, mood disorders, multiple sclerosis, and psoriasis through a variety of methods. For the PLM sample, registered members who had logged onto the site at least once in the preceding 90 days were invited to participate. Iterative messaging pilots were used by PLM to maximize response rates; a single automated reminder also was used three days after the initial invitation for members who had logged onto the site but had not acknowledged or had declined the invitation to participate in this research.
Data Analysis: Statistical Methods, Incomplete Data, and Statistical Correction
Descriptive statistics were calculated on the CRNRC and PLM data samples. Frequencies (n) and percentages (%) were used to describe the distributions of categorical variables. Z-ratios for the differences in independent proportions were calculated and used to compare the CRNRC and PLM populations with respect to their attitudes on health-related data sharing and health care team coordination. Chi-square statistics were also calculated to test for differences between men and women with respect to their attitudes on health-related data sharing in both samples. Missing data were omitted from question-specific analyses; statistical significance was set at p<0.005; and all tests were two-tailed. Analyses were conducted in SAS Version 9.3 (Cary, NC).
Limitations
This research is not without limitations, primarily the limitations of online-based studies, such as potentially biased participation, uncertain data collection accuracy, and variation in health care coverage. Secondly, both the CRNRC and PLM respondents are partially self-selected populations. It is also likely that PLM respondents are early adopters of technology, and, as a result, there may be an information divide between PLM respondents’ opinions and those of the general population (Fox and Purcell, 2010).
PLM/IOM Survey Instrument on Data Sharing
Current Practices
1. How often do you turn to each of the following about health issues or how to treat a health condition? (scale: very important, somewhat important, only a little important, not at all important)
- My [practitioner]
- Friend (male/female)
- Spouse or partner (male/female)
- Child (male/female)
- Other relative (male/female)
- Family or friend who works in the health care field (male/female)
- Media (TV, radio, or print)
- Medical information on the Internet*
- Online patient community*
- Advertising about drugs or medical devices
- Others with the same condition
- Other (specify)
[CRNRC survey q7]
*the original answer from CRNRC survey, “Internet,” was broken up into two options
2. Do you share the information on your PatientsLikeMe profile with…?
- Spouse or partner
- Child
- Friend
- Caregiver
- Other (specify)
3. How important was each of the following in helping you decide to start sharing your health data on PatientsLikeMe? (scale: very important, somewhat important, only a little important, not at all important).
- Means to track your health over time
- Compare your experience with the experience of others
- For community support from other individuals with similar health
- So other patients can benefit from your experience*
- Other (specify)
*this option is parallel to an option in question 8
Attitudes/Beliefs
“Now, thinking about the use of your health care information outside of PatientsLikeMe…”
4. Do you believe your health data is currently used to help improve the care of future patients who might have the same or similar condition?
- Yes
- No
- Don’t know
[CRNRC q17a]
5. Please indicate your level of agreement with the following statement: (scale: strongly agree, somewhat agree, somewhat disagree, strongly disagree)
“My health data should be used to help improve the care of future patients who might have the same or similar condition.”
[CRNRC survey q17b]
6. Please indicate with whom you would be willing to share the following information from your personal health record. (Medication list; scheduled appointments; laboratory or study results; patient-entered health information; basic information [age, height, blood pressure]; communication with provider; my diagnosis; treatment plan)
- Spouse or partner
- Close relatives, like your parents or children
- Your employer
- Your health insurance company or health plan
- The doctor you use most often
- Other doctors and health professionals involved with your own health care
- Doctors and other health professionals not involved with your own health care
- Pharmacies
- Drug companies
- Government agencies
7. Please indicate how concerned you are that information from your personal health record might be… (scale: very concerned, somewhat concerned, only a little concerned, not at all concerned)
- Used to deny me health care benefits
- Used to limit my job opportunities
- Used without my knowledge
- Stolen by unknown individuals or companies
8. Assuming that there is no way anyone will have access to your identity, would you be willing to share your health information so that…(answer: yes, no, don’t know)
- Doctors and hospitals can improve their services
- Researchers can learn about the quality of health care, disease and prevention, and related issues
- Public health officials can improve the health of my community*
- Public health officials can learn about and improve the health of the U.S. population*
- Other patients can benefit from my experience**
- Drug companies can make safer products
- Drug companies can make more effective products
- Drug companies can learn more about your condition
- Drug companies can improve their services
- Other (specify)**
*Original answer, “Public health officials can scan for bioterrorist attacks,” was changed
**Not in original survey
9. How secure do you think that your medical records are when they are stored in each of the following ways? (scale: very secure, somewhat secure, only a little secure, not secure at all)
- Paper
- Electronically
Background/Demographics
10. How do you rate your current state of health?
- Excellent
- Very good
- Good
- Fair
- Poor
[CRNRC survey q21]
11. When was the last time you visited your (practitioner), your main health care provider?
- Less than 1 year ago
- 1 year to less than 2 years ago
- 2 years to less than 3 years ago
- 3 years to less than 5 years ago
- 5 years to less than 10 years ago
- 10 years ago or longer
- Don’t know
[CRNRC survey q3]
[IF “Less than 1 year ago” in Q11, ASK Q12, otherwise skip to Q13]
12. During the past 12 months, not counting times you went to an emergency room, how many times did you go to (practitioner) to get care for yourself?
- None
- 1 time
- 2 times
- 3 times
- 4 times
- 5-9 times
- 10 or more times
- Don’t know
[CRNRC survey q4]
13. Are you able to access your health information online from your care provider?
- Yes
- No
- Don’t know
14. Do you yourself currently have health insurance?
- Yes
- No
- Don’t know
[CRNRC survey q19]
[IF “Yes” in Q14, ASK Q15, otherwise skip to Q16]
15. Which of the following statement represents your health insurance coverage?
- I currently get my health insurance through my employer
- I currently get my health insurance through my spouse’s employer
- I currently get my health insurance through Medicaid, Medicare, or through my state insurance plan
- I currently get my health insurance through COBRA
- I am self-insured; I currently get my health insurance privately
- Don’t know
[CRNRC survey q20]
16. Are you…?
- Male
- Female
[CRNRC survey q23]
Please indicate the year you were born _____
[CRNRC survey q24]
17. Are you Spanish, Hispanic, or Latino?
- Yes
- No
- Prefer not to answer
[CRNRC survey q25]
18. Which of the following describe your race? You can select as many as apply.
- White/Caucasian
- Black/African American
- Asian/Asian American
- Other race
- Prefer not to answer
[CRNRC survey q26]
19. Was your TOTAL household income BEFORE taxes for 2011…?
- Under $15,000
- $15,000 but less than $20,000
- $20,000 but less than $25,000
- $25,000 but less than $30,000
- $30,000 but less than $35,000
- $35,000 but less than $40,000
- $40,000 but less than $50,000
- $50,000 but less than $60,000
- $60,000 but less than $75,000
- $75,000 but less than $100,000
- $100,000 but less than $125,000
- $125,000 or more
[CRNRC survey q27]
References
- Adamson J., R. Gooberman-Hill, G. Woolhead, and J. Donovan. 2004. “Questerviews”: Using questionnaires in qualitative interviews as a method of integrating qualitative and quantitative health services research.
Journal of Health Services Research & Policy 9(3):139-145. https://doi.org/10.1258/1355819041403268 - Angwin, J., and S. Stecklow. 2010. “Scrapers” dig deep for data on Web. Wall Street Journal, October 11. Available at: http://online.wsj.com/article/SB10001424052748703358504575544381288117888.html (accessed April,
30, 2013). - Böhme, R. and S. Köpsell. 2010. Trained to accept?: Field experiment on consent dialogs. Proceedings of the 28th ACM Conference on Human Factors in Computing Systems. Association for Computing Machinery. https://doi.org/10.1145/1753326.1753689
- Brenner, J. 2013. Pew Internet: Social networking. Pew Internet & American Life Project. Available at: http://pewinternet.org/Commentary/2012/March/Pew-Internet-Social-Networking-full-detail.aspx (accessed April 30, 2013).
- DiSogra, C. 2010. Address-based sampling nets success for KnowledgePanel® recruitment and sample representation. Accuracy’s Impact on Research. Available at: http://www.ca.knowledgenetworks.com/accuracy/spring2010/pdf/disogra-spring10.pdf (accessed April 30, 2013).
- Eysenbach, G. 2008. Medicine 2.0: Social networking, collaboration, participation, apomediation, and openness. Journal of Medical Internet Research 10(3):e22. https://doi.org/10.2196/jmir.1030
- Fernandez-Luque, L., N. Elahi, and F. Grajales. 2009. An analysis of personal medical information disclosed in YouTube videos created by patients with multiple sclerosis. Studies in Health Technology and Informatics
150:292-296. Available at: https://pubmed.ncbi.nlm.nih.gov/19745316/ (accessed May 26, 2020). - Fox, S., and K. Purcell 2010. Chronic disease and the Internet. Pew Internet & American Life Project. Available at: http://www.pewinternet.org/Reports/2010/Chronic-Disease.aspx (accessed April 30, 2013).
- Fox, S., and M. Duggan. 2013. Health online 2013. Pew Internet & American Life Project. Available at: http://www.pewinternet.org/Reports/2013/Health-online.aspx (accessed April 30, 2013).
- Forbes. 2012. What you actually need to know about the changes Facebook is making to its privacy policy. Available at: http://www.forbes.com/sites/kashmirhill/2012/11/26/what-you-actually-need-to-know-about-the-changes-facebook-is-making-to-its-privacy-policy (accessed April 30, 2013).
- HHS (Department of Health and Human Services). Omnibus HIPAA Final Rule. Available at: http://www.hhs.gov/ocr/privacy/hipaa/administrative/omnibus/index.html (accessed June 30, 2013).
- Alston, C., L. Paget, G. Halvorson, B. Novelli, J. Guest, P. McCabe, K. Hoffman, C. Koepke, M. Simon, S. Sutton, S. Okun, P. Wicks, T. Undem, V. Rohrbach, and I. Von Kohorn. 2012. Communicating with Patients on Health Care Evidence. NAM Perspectives. Discussion Paper, National Academy of Medicine, Washington, DC. https://doi.org/10.31478/201209d
- Okun, S., D. McGraw, P. Stang, E. Larson. D. Goldmann, J. Kupersmith, R. Filart, R. M. Robertson, C. Grossmann, and M. D. Murray. 2013. Making the case for continuous learning from routinely collected data. NAM Perspectives. Discussion Paper, National Academy of Medicine, Washington, DC. https://doi.org/10.31478/201304d
- NIH (National Institutes of Health). 2008. Genomic Information Nondiscrimination Act of 2008. Available at: http://www.genome.gov/24519851 (accessed April 30, 2013).
- Nissenbaum, H. 2004. Privacy as contextual integrity. Washington Law Review 79(1):101-139. Available at: https://crypto.stanford.edu/portia/papers/RevnissenbaumDTP31.pdf (accessed May 26, 2020).
- O’Connor, D. 2013. The apomediated world: Regulating research when social media has changed research. Journal of Law, Medicine, and Ethics 41(2):470-483. https://doi.org/10.1111/jlme.12056
- Okoli, C., and S. Pawlowski. 2004. The Delphi method as a research tool: An example, design considerations, and applications. Information & Management 42(1):15-29. https://doi.org/10.1016/j.im.2003.11.002
- PCORI (Patient-Centered Outcomes Research Institute). 2013. Comprehensive inventory of research networks: Clinical data research networks, patient-powered research networks, and patient registries. Available at: http://pcori.org/assets/2013/06/PCORI-Comprehensive-Inventory-Research-Networks-061213.pdf (accessed June 30, 2013).
- Pearson, J., C. Brownstein, and J. Brownstein. 2011. Potential for electronic health records and online social networking to redefine medical research. Clinical Chemistry 57(2):196-204. https://doi.org/10.1373/clinchem.2010.148668
- Ramo, D., and J. Prochaska. 2012. Broad reach and targeted recruitment using Facebook for an online survey of young adult substance use. Journal of Medical Internet Research 14(1):e28. https://doi.org/10.2196/jmir.1878
- Solberg, L. 2012. Regulating human subjects research in the information age: Data mining on social networking sites. Northern Kentucky Law Review 39(2):327-358. Available at: https://papers.ssrn.com/sol3/papers.cfm?abstract_id=2157302 (accessed May 26, 2020).
- Walters, H. 2013. When our private lives become public online … will it make us more or less tolerant? TED Blog. Available at: http://blog.ted.com/2013/05/02/when-our-private-lives-become-public-online-will-it-make-us-more-orless-tolerant (accessed June 30, 2013).
- Wicks P., D. Keininger, M. Massagli, C. de la Loge, C. Brownstein, J. Isojarvi, and J. Heywood. 2012. Perceived benefits of sharing health data between people with epilepsy on an online platform. Epilepsy & Behavior
23:16-23. https://doi.org/10.1016/j.yebeh.2011.09.026