Designing Health Literate Mobile Apps
Overview
As mobile devices become more pervasive, mobile health (mHealth) application software (apps) presents an exciting new opportunity to improve health and wellness. However, if mobile apps are poorly designed, they may contribute to the challenges most users face in trying to understand and act on health information—challenges that are exacerbated for users with low health literacy. We believe that health literate apps have the potential to improve the quality and usefulness of health information for all users, leading to better outcomes. With this in mind, we call on developers to build “health literate apps”—apps that apply both usability and health literacy strategies throughout the development process. We offer a blend of health literacy– and usability-improving strategies that can help developers build health literate apps. We present a case study in mHealth design from a 2012 mobile app challenge, organized by the U.S. Department of Health and Human Services’ Office of Disease Prevention and Health Promotion (ODPHP), to demonstrate how these strategies can be applied throughout the development process.
Why Apply Health Literacy Strategies to Mobile Apps?
More Americans are using mobile devices to access health information than ever before. Mobile devices, which include smartphones, tablets, and Internet-connected devices, represent a rapidly growing market. Smartphone prevalence has increased from 33 percent of all mobile phones in 2011 to 53 percent in 2012 (Fox, 2012; Smith, 2012), and 25 percent of American adults owned a tablet by mid-2012 (Rainie, 2012). Smartphones and tablets are unique in that they allow users to download apps and access information at any time without being connected to a computer or an Internet service provider.
The digital divide is closing, thanks in large part to the surge in mobile devices. Smartphone ownership is proportionately higher among minorities, people who live in urban areas, and people aged 18-29 years, as well as those without high school diplomas (Smith, 2012). African Americans and Hispanics also show a greater rate of growth in tablet adoption than whites (Raine, 2012).
Mobile devices show promise as tools for delivering health information and helping users manage their health. Health information was the fastest-growing content category in mobile device use in 2011 (comScore, 2012), and, in 2012, more than half of smartphone users gathered health information on their phones (Fox, 2012). Surveys show that 20-30 percent of smartphone users download apps related to their health (Fox, 2012; Purcell, 2011). Minorities are more likely to use their smartphone to access health information and track their health (Fox, 2012), and health-focused apps are more likely to be downloaded by African Americans and Hispanics than the white non-Hispanic population (Fox, 2011; Purcell, 2011). This dramatic rise in access to and use of health information on mobile devices offers new possibilities for engaging everyone with the information they need to manage their health.
What are Health Literate Apps?
Although the growing prevalence of digital devices and mHealth apps hold great promise for achieving universal access to reliable health information, the benefit to users and, ultimately, the effect on health outcomes are diminished when apps are not designed for users of all health literacy levels.
Health literacy is defined in the Affordable Care Act (ACA) as “the degree to which an individual has the capacity to obtain, communicate, process, and understand health information and services in order to make appropriate health decisions.” Only 12 percent of Americans are proficient in understanding and acting on health information (Koh et al., 2013; Kutner et al., 2006). More than half of American adults have low health literacy; minorities, the elderly, and those with lower educational attainment and socioeconomic status are disproportionately affected (AHRQ, 2011; Baker et al., 2007; Berkman et al., 2011; Chaudhry et al., 2011; Gazmararian et al., 1999; IOM, 2004; Paasche-Orlow et al., 2005; Vernon et al., 2007). Low health literacy is linked to
- earlier death in elderly populations (Baker et al., 2007; Sudore et al., 2006),
- poor understanding of disease,
- lower reported health status,
- poor disease management,
- lower use of preventive care (AHRQ, 2004, 2011; Berkman et al., 2011; DeWalt et al., 2004), and
- higher rates of obesity (Huizinga et al., 2008).
Lower-literacy users experience more difficulty when accessing information online (Nielsen, 2005). These challenges may also translate to mHealth apps, which present additional usability issues, such as smaller screens for content display and tricky text-entry methods (Harrison et al., 2013; Pew, 2011).
Health literacy has been described as the juxtaposition of individuals’ skills and abilities with the demands and complexity of the health care system (IOM, 2009). Likewise, individuals’ health literacy skills and abilities are also a function of the complexity and ease of use of the communication channels and devices that carry health information. In either case, both health care organizations and those who develop communication channels and devices have a responsibility to make health information understandable and easy to use for people of all health literacy levels.
This systems approach to health literacy was reflected in a recent Institute of Medicine (IOM) discussion paper that coined the term “health literate organizations”—organizations that support people as they navigate, understand, and use information and services to take care of their health, thereby improving their health literacy (Brach, et al., 2012).
We suggest that health literate apps, like health literate care organizations, will have more satisfied and engaged users if health literacy–improving strategies are built into their products and services.
Strategies for Developing Health Literate MHealth Apps
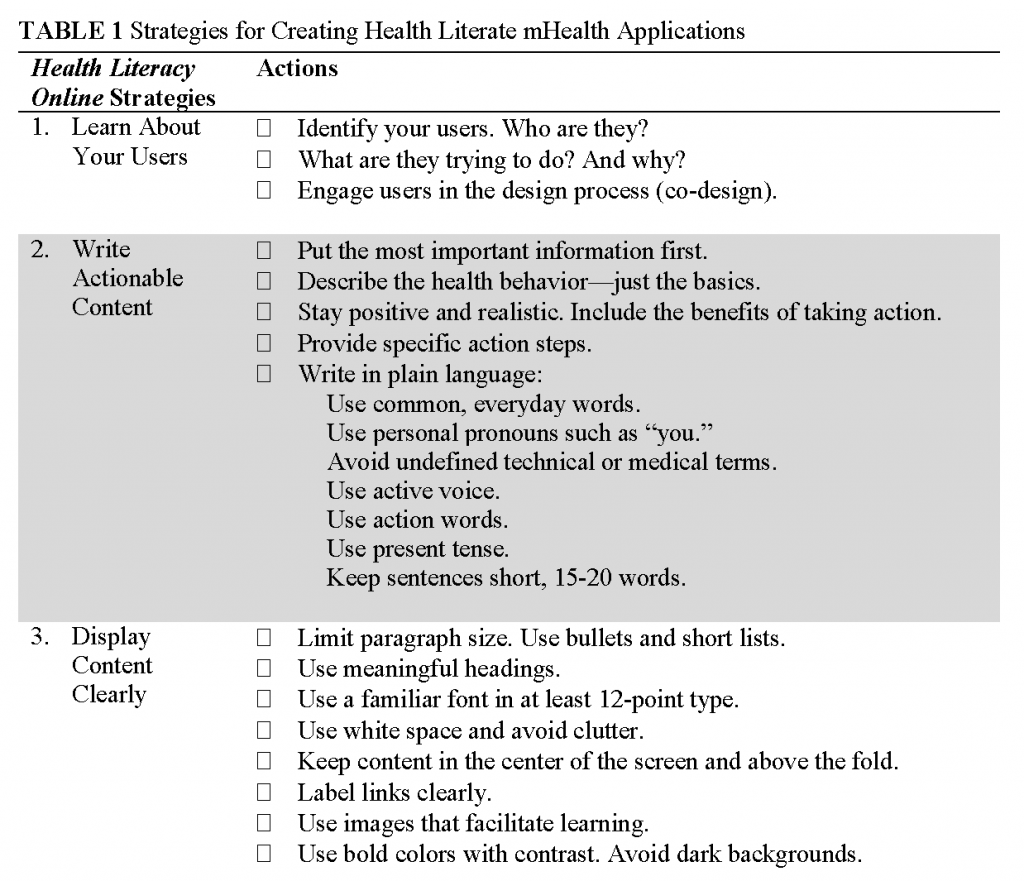
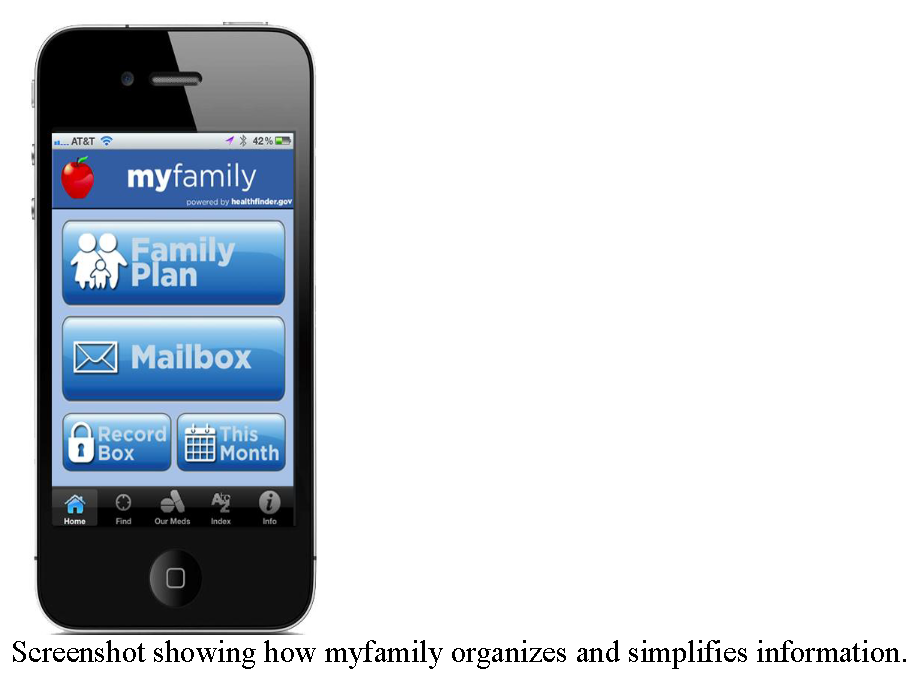
We believe that usability and health literacy strategies should guide the development of mHealth apps. We draw upon the six strategies and related actions outlined in Health Literacy Online: Strategies for Writing and Designing Easy To-Use Health Web Sites, an evidence-based guide with steps that developers and Web managers can take to design websites that improve users’ health literacy (ODPHP, 2010). Health Literacy Online, originally developed as guidance for designing health websites, contains both usability and health literacy–improving strategies (ODPHP, 2010). These strategies can also be used to create health literate mHealth apps. Table 1 lists these strategies, along with actions that can be taken for each strategy to develop health literate mHealth apps. The table can also serve as a checklist for developers to ensure that they have strived to create health literate apps. We believe that the successful implementation of these strategies will lead to more effective and user-friendly applications that engage users and have a positive impact on health. In a later section of this paper, we use a case study to examine how these strategies were used in the development of mHealth applications.
healthfinder.gov Case Study
In 2012, healthfinder.gov launched a mobile app challenge that awarded developers a cash prize for creating an easy-to-use mHealth app that used healthfinder’s content via the Application Programming Interface (API). Healthfinder.gov is an award-winning website that was designed and developed based on extensive formative research and usability testing (Healthfinder.gov was designed based on formative research, card sorting, interviews, and usability testing with more than 700 people, many of whom had limited health literacy. This research is also the basis of Health Literacy Online.) and is written in plain, actionable language. As part of the healthfinder.gov mobile app challenge, ODPHP, in coordination with health care technology company Health 2.0 and the Robert Wood Johnson Foundation, challenged developers to work together with health professionals and potential end users to co-design a mobile application.
Lyfechannel, the team that won the mobile app challenge, used Health Literacy Online extensively as a reference in creating its app, called myfamily. The myfamily app helps users build personal and family health plans based on the priorities of the ACA and healthfinder.gov content. The myfamily mobile app reflects the action items of Health Literacy Online’s six main strategies. In the next section of this paper, we will explore how Lyfechannel integrated these strategies throughout the mHealth app development process.
Learn About Your Users (Strategy 1)
Co-design, which involves end users in testing a website or app and applies their feedback, is one of the primary principles in designing user-friendly websites. Co-design is one way developers can learn about users and conceptualize, evaluate, and revise the site or app. It is unique from usability testing in that it encourages developers to engage end users from the onset—building the app from the start with the end user in mind.
The healthfinder.gov mobile app challenge included co-design as part of the judging criteria, and all three finalists reported that their apps were improved by the feedback they received through the crowd-sourcing platform Health Tech Hatch. Although co-design using a crowd-sourcing platform was one criterion in the challenge, Lyfechannel went one step further in learning about and understanding the needs of potential users of the app by conducting user testing in the parking lot of a popular discount store.
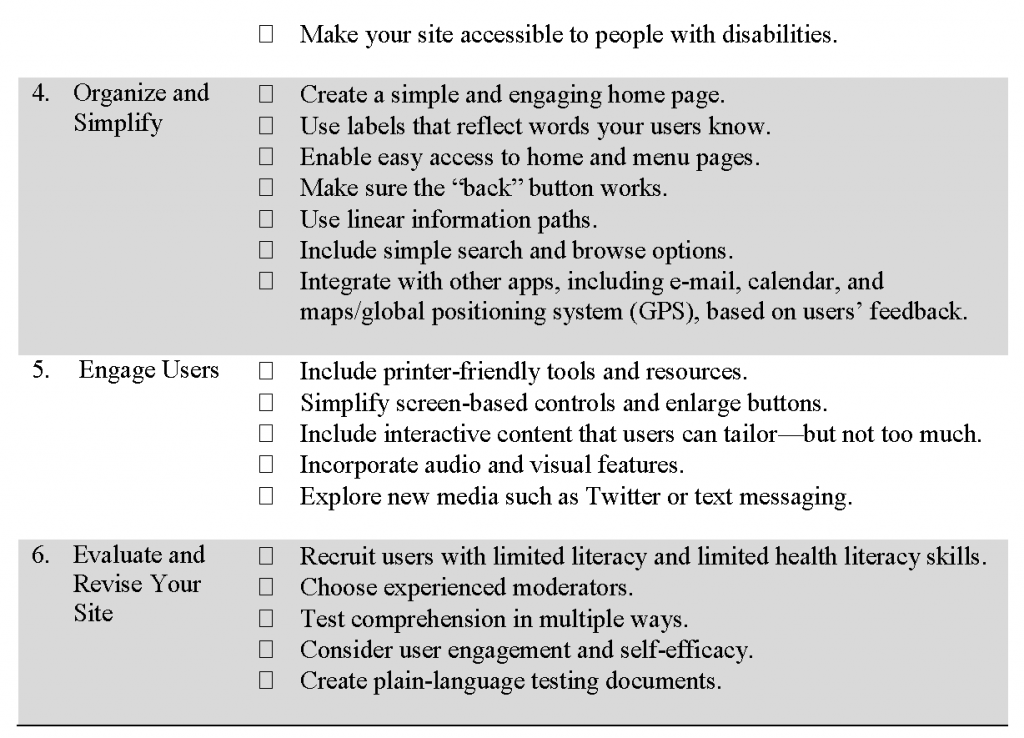
In a follow-up interview, Dave Vockell, lead designer of the winning myfamily app, said that co-design “really changed how [Lyfechannel] thought about how the information should be presented” and that it moved Lyfechannel’s vision from creating an app focused on just providing health information to an app that provided health management tools. App challenge participants also noted that the co-design process gave them ideas they had not thought of in the early stages of developing their apps for the challenge. Table 2 shows a sample of responses Lyfechannel received as part of its co-design process and the resulting action taken by the team in developing the final app.
Write Actionable Content (Strategy 2)
Action-oriented language is characterized by short statements with positive messages that quickly explain the benefit of a healthy behavior, followed by information on how to take action. Because mHealth apps are often intended to help users adopt healthy behaviors and/or manage their health, action-oriented language is important because it helps users act on the information they find in the app.
Action-oriented content should also be written in plain language, which is recognized as one of the keys to health literacy by government, academia, nonprofits, and hospitals (Stableford, 2007). Plain language is communication that allows users to find what they need, understand what they find, and act on what they find (PLAIN, 2013). It isn’t “dumbed-down” language; it is grammatically correct and utilizes full sentences and proper sentence structure, while also making the information easy to understand.
Apps created with plain language clearly communicate in a way that the intended user understands by presenting action-oriented information that is free of medical or technical jargon. Creating apps with plain language improves user experience and makes apps more functional by ensuring that most users can understand the content of the app.
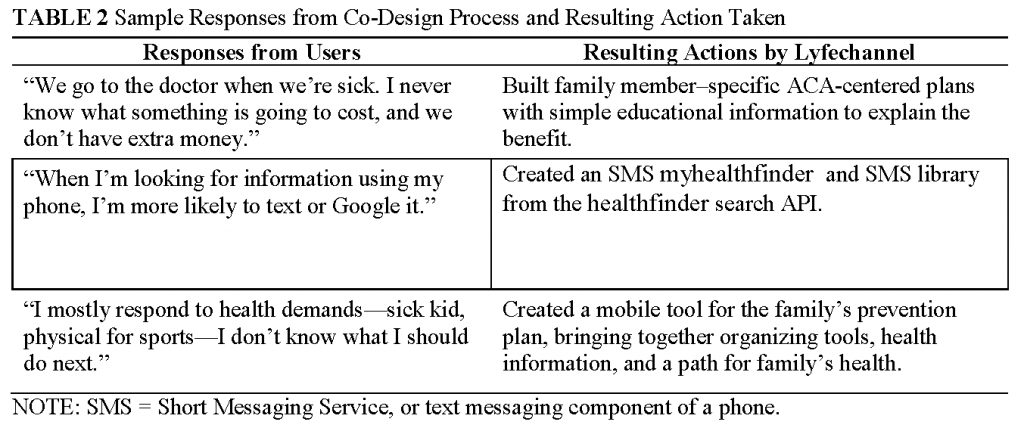
When developing the myfamily app, Lyfechannel organized actionable information from healthfinder content in a way that prioritized the most important information first. The family prevention plan builder, the foundation of the mobile app, is the top option on the homepage of the app, and the other main features are presented clearly on the screen.
In the family prevention plan, recommendations for family members are accompanied by basic information and realistic action steps to meet each recommendation. The myfamily app enables users to prioritize these small steps by saving tips and resources to a “Record Box,” scheduling vaccinations in the app’s calendar feature, or looking up local available health services.
Display Content Clearly (Strategy 3)
Displaying content clearly includes grouping information in a clear, consistent way and making sure that information is easily viewable and accessible. Information grouping, or “chunking,” means organizing information in short sections or groups of related items. Chunking reduces the amount of information in one place and helps users better retain the information. The classic study by George A. Miller (1956) notes that most people can only remember and act on about seven pieces of information held in their short-term memories. Chunking prevents information overload and is the best way to present information on the small screens of mobile devices. The smaller screen size of mobile devices makes chunking an important consideration when creating mHealth apps. Information needs to be broken down and presented in smaller chunks than would be seen on a computer screen. Chunking allows developers to use bigger font and mitigate the urge to squeeze extra information into a screen. Use of font and white space also affects users’ ability to read and fully understand the information provided by an app. Mobile Web safe sans-serif fonts like Arial, Helvetica, Lucinda Grande, Georgia, Times New Roman, and Verdana are highly readable, even on mobile devices.
The myfamily app displays content clearly and applies chunking by reusing healthfinder.gov content in short lists, bold headings, and legible fonts. The design of the app was based on feedback obtained from end users during the development process. The app also ensures that images and content are easy to view and accessible. Bold, primary colors are used against white backgrounds, and white title fonts are used against dark backgrounds. Images are borrowed from the healthfinder.gov website. Additionally, following a requirement of the healthfinder.gov mobile app challenge, Lyfechannel developed the app in a way that makes it accessible to people with disabilities.
Organize and Simplify (Strategy 4)
To organize and simplify means to employ consistent navigation and clean design to make apps more intuitive and easier to use, especially for people with low literacy. Consistent navigation reduces the burden on the user and makes it easier to move to and from information sources. Low-literacy users can be unfamiliar with the function of common navigation features like dropdown menus and often ignore them, preferring “back” and “forward” buttons (ODPHP, 2010).
A back button and consistent layout on each page allows the user to maneuver through the app without getting confused or stuck. Integration with e-mail, calendar, GPS, and other apps are also very useful, especially for mHealth apps.
The myfamily app applies consistent navigation and clean design by laying out the main features of the app through a neatly ordered homepage. Users are not expected to scroll through long pages of text and are easily directed toward previously viewed pages via labeled buttons. A highlighted button in the lower-left corner of the app allows users to return to the home screen and start again. The family plan, recommendations, and action steps are organized in a linear path. Additional services and resources, such as Service Locator, Medication Adherence Tool, and alphabetized (A-Z) index of health topics are clearly marked at the bottom of the screen. In the A-Z index of topics, users can search for information or browse by letter.
Engage Users (Strategy 5)
Engaging users through print and share features, integrated new media, and customizable content like polls or quizzes allows them to interact with content and integrate it with their daily lives. For some users with limited literacy skills, printing information from a website is preferable to reading it online (ODPHP, 2010). Print and share features should allow users with limited literacy skills to easily print content and share it with their doctors, families, and friends.
Ensuring that these features are easy to use, with simple input functions and large buttons and text fields, is also key.
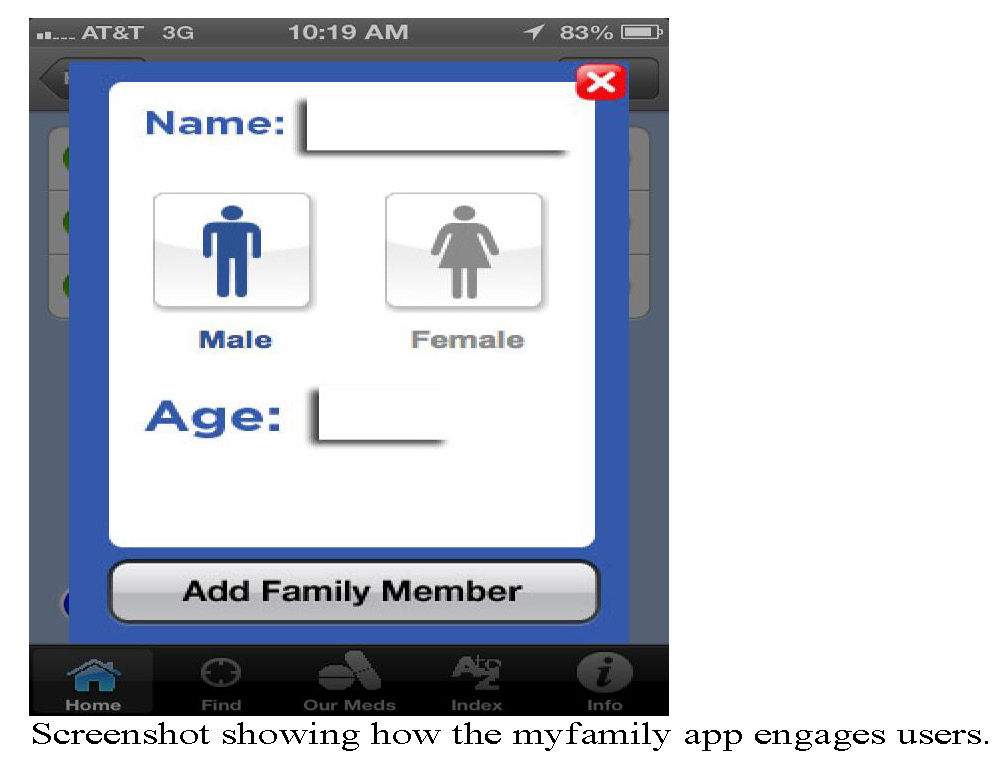
The myfamily app engages users in managing their family’s health by incorporating the myhealthfinder widget, which allows users to access tailored ACA-covered preventive services recommendations for each member of their family, based on family members’ age, gender, and pregnancy status. App users can then engage with this content by saving priority information and creating a personal calendar. The myfamily app also allows users to share information via their social networks.
Evaluate and Revise Your Site (Strategy 6)
Evaluating and revising the app plays an important role in ensuring that an app is health literate. Iterative feedback from usability tests that include users with limited literacy and limited health literacy skills is an important component of this. Health Literacy Online suggests that moderators should be experienced; comprehension should be tested in multiple ways; and testing documents should be in plain language.
Lyfechannel made revisions to their app based on iterative feedback from both Health Tech Hatch and its informal in-person usability testing. For example, one of the changes was to revise the title of the app itself to resonate more with target users. Lyfechannel continues to make technical updates to the app based on feedback it receives from partners and other interested groups, including the IOM Roundtable on Health Literacy’s member organizations.
Conclusion
We believe the need to integrate health literacy into the development of mHealth apps is critical. The healthfinder.gov app challenge and the winning app demonstrate how incorporating health literacy strategies throughout the development process creates effective apps.
Although the app challenge case study discussed above highlighted ways to design health literate mobile apps, ongoing discussion and work in this arena is needed. Next steps include, notably, the development of an assessment tool to determine the extent to which a mHealth app is health literate. We believe conducting research to monitor the impact of health literate mHealth apps on end users’ attitudes, knowledge, beliefs, and behavior related to health information is also important. Together, an assessment tool and research could spur further integration and innovation around health literacy principles in mHealth app design. Finally, as technology and mHealth apps continue to grow and change, additional health literacy strategies or criteria may be needed to support developers in integrating health literacy.
Access and use of mHealth apps is on the rise. We believe one way to maximize the potential of mHealth apps to improve health is to ensure that these apps are designed to deliver health information that is simple, engaging, and easy to use for people of all literacy levels. Applying evidence-based health literacy strategies to the development of mHealth apps is one way more Americans can improve their health through clear, actionable information and easy-to-navigate mobile devices.
References
- AHRQ (Agency for Healthcare Research and Quality). 2004. Literacy and health outcomes: Summary. Rockville, MD: AHRQ. Available at: https://www.ncbi.nlm.nih.gov/books/NBK11942/ (accessed May 26, 2020).
- AHRQ. 2011. Health literacy interventions and outcomes: An updated systematic review. Rockville, MD: AHRQ, U.S. Department of Health and Human Services. Available at: https://www.ahrq.gov/downloads/pub/evidence/pdf/literacy/literacyup.pdf (accessed May 26, 2020).
- Baker, D. W., M. S. Wolf, J. Feinglass, J. A. Thompson, J. A. Gazmararian, and J. Huang. 2007. Health literacy and mortality among elderly persons. Archives of Internal Medicine 167(14):1503-1509. https://doi.org/10.1001/archinte.167.14.1503
- Berkman, N. D., S. L. Sheridan, K. E. Donahue, D. J. Halpern, and K. Crotty. 2011. Low health literacy and health outcomes: An updated systematic review. Annals of Internal Medicine 155(2):97-107. https://doi.org/10.7326/0003-4819-155-2-201107190-00005
- Brach, C., D. Keller, L. M. Hernandez, C. Baur, R. Parker, B. Dreyer, P. Schyve, A. J. Lemerise, D. Schillinger. 2012. Ten Attributes of Health Literate Health Care Organizations. NAM Perspectives. Discussion Paper, National Academy of Medicine, Washington, DC. https://doi.org/10.31478/201206a
- Chaudhry, S. I., J. Herrin, C. Phillips, J. Butler, S. Mukerjhee, J. Murillo, A. Onwuanyi, T. B. Seto, J. Spertus, and H. M. Krumholz. 2011. Racial disparities in health literacy and access to care among patients with heart
failure. Journal of Cardiac Failure 17(2):122-127. https://doi.org/10.1016/j.cardfail.2010.09.016 - comScore. 2012. U.S. Digital future in focus 2012. Available at: http://www.comscore.com/Insights/Presentations_and_Whitepapers/2012/2012_US_Digital_Future_in_Focus (accessed January 14, 2014).
- DeWalt, D. A., N. D. Berkman, S. Sheridan, K. N. Lohr, and M. P. Pignone. 2004. Literacy and health outcomes. Journal of General Internal Medicine 19(12):1228-1239. https://doi.org/
- 10.1111/j.1525-1497.2004.40153.x
- Fox, S. 2011. The social life of health information. Washington, DC: Pew Internet and American Life Project. Available at: https://www.pewresearch.org/internet/2011/05/12/the-social-life-of-health-information-2011/ (accessed May 26, 2020).
- Fox, S. 2012. Mobile health 2012. Washington, DC: Pew Internet and American Life Project. Available at: https://www.pewinternet.org/wp-content/uploads/sites/9/media/Files/Reports/2012/PIP_MobileHealth2012_FINAL.pdf (accessed May 26, 2020).
- Gazmararian, J. A., D. W. Baker, M. V. Williams, R. Parker, T. L. Scott, D. C. Green, S. N. Fehrenbach, J. Ren, and J. F. Koplan. 1999. Health literacy among Medicare enrollees in a managed care organization. JAMA
281(6):545-551. https://doi.org/10.1001/jama.281.6.545 - Harrison, R., D. Flood, and D. Duce. 2013. Usability of mobile applications: Literature review and rationale for a new usability model. Journal of Interaction Science 1(1):1-16. Available at: https://link.springer.com/article/10.1186/2194-0827-1-1 (accessed May 26, 2020).
- Huizinga, M. M., B. M. Beech, K. L. Cavanaugh, T. A. Elasy, and R. L. Rothman. 2008. Low numeracy skills are associated with higher BMI. Obesity 16(8):1966-1968. https://doi.org/10.1038/oby.2008.294
- Institute of Medicine. 2004. Health Literacy: A Prescription to End Confusion. Washington, DC: The National Academies Press. https://doi.org/10.17226/10883
-
Institute of Medicine. 2009. Measures of Health Literacy: Workshop Summary. Washington, DC: The National Academies Press. https://doi.org/10.17226/12690
- Koh, H. K., C. Brach, L. M. Harris, and M. L. Parchman. 2013. A proposed “health literate care model” would constitute a systems approach to improving patients’ engagement in care. Health Affairs 32(2):357-367. https://doi.org/10.1377/hlthaff.2012.1205
- Kutner, M., E. Greenberg, Y. Jin, C. Paulsen, and S. White. 2006. The health literacy of America’s adults: Results from the 2003 National Assessment of Adult Literacy. Washington, DC: U.S. Department of Education,
National Center for Education Statistics, Institute of Education Services. Available at: https://nces.ed.gov/pubs2006/2006483.pdf (accessed May 26, 2020). - Miller, G. A. 1956. The magical number seven, plus or minus two: Some limits on our capacity for processing information. Psychological Review 63(2):81. https://doi.org/10.1037/h0043158
- Nilsen, W., S. Kumar, A. Shar, C. Varoquiers, T. Wiley, W. T. Riley, M. Pavel, and A. A. Atienza. 2012. Advancing the science of mhealth. Journal of Health Communication 17(Suppl 1):5-10. https://doi.org/10.1080/10810730.2012.677394
- ODPHP (Office of Disease Prevention and Public Health Promotion). 2010. Health literacy online: A guide to writing and designing easy-to-use health web sites. Washington, DC: U.S. Department of Health and
Human Services. Available at: https://health.gov/healthliteracyonline/2010/Web_Guide_Health_Lit_Online.pdf (accessed May 26, 2020). - Paasche-Orlow, M. K., R. M. Parker, J. A. Gazmararian, L. T. Nielsen-Bohlman, and R. R. Rudd. 2005. The prevalence of limited health literacy. Journal of General Internal Medicine 20(2):175-184. https://doi.org/10.1111/j.1525-1497.2005.40245.x
- PLAIN (Plain Language Action and Information Network). 2013. What is plain language? Available at: http://www.plainlanguage.gov/whatisPL/index.cfm (accessed August 29, 2013).
- Purcell, K. 2011. Half of adult cell phone owners have apps on their phones. Washington, DC: Pew Internet and American Life Project. Available at: https://www.pewresearch.org/internet/wp-content/uploads/sites/9/media/Files/Reports/2011/PIP_Apps-Update-2011.pdf (accessed May 26, 2020).
- Rainie, L. 2012. 25% of American adults own tablet computers. Washington, DC: Pew Internet and American Life Project. Available at: https://www.pewresearch.org/internet/wp-content/uploads/sites/9/media/Files/Reports/2012/PIP_TabletOwnership_August2012.pdf (accessed May 26, 2020).
- Smith, A. 2011. Americans and their cell phones. Washington, DC: Pew Internet and American Life Project. Available at: https://www.pewresearch.org/internet/wp-content/uploads/sites/9/media/Files/Reports/2011/Cell-Phones-2011.pdf (accessed May 26, 2020).
- Smith, A. 2012. Smartphone ownership 2012. Washington, DC: Pew Internet & American Life Project. Available at: https://www.pewresearch.org/internet/wp-content/uploads/sites/9/media/Files/Reports/2013/PIP_Smartphone_adoption_2013_PDF.pdf (accessed May 26, 2020).
- Stableford, S., and W. Mettger. 2007. Plain language: A strategic response to the health literacy challenge. Journal of Public Health Policy 28(1):71-93. https://doi.org/10.1057/palgrave.jphp.3200102
- Sudore, R. L., K. Yaffe, S. Satterfield, T. B. Harris, K. M. Mehta, E. M. Simonsick, A. B. Newman, C. Rosano, R. Rooks, and S. M. Rubin. 2006. Limited literacy and mortality in the elderly: The health, aging, and body
composition study. Journal of General Internal Medicine 21(8):806-812. https://doi.org/10.1111/j.1525-1497.2006.00539.x - Vernon, J. A., A. Trujillo, S. Rosenbaum, and D. DeBueno. 2007. Low health literacy implications for national policy. Available at: http://sphhs.gwu.edu/departments/healthpolicy/CHPR/downloads/LowHealthLiteracyReport10_
4_07.pdf (accessed February 28, 2013).