A Sustainable Financial Model for Community Health Systems
The key to the long term survival of the health care reforms being implemented under the Affordable Care Act (ACA) has little to do with the enrollment websites that have attracted so much attention and everything to do with transforming the performance of the systems that provide health care and promote health. The common framework for measuring the change in performance is the Triple Aim—better control of total per capita costs, better experience of care for those who need it, and better health for the population (Berwick et al., 2008). An impressive array of new payment and service models is being tested with encouraging signs of success with the first two aims—total cost and patient experience. Models for improving the health of the population have proven to be more elusive both because less attention has been focused on them and because the issue is more challenging (Hester, 2013). Timing is a major challenge in order to utilize the window of opportunity created by the current wave of reform initiatives (Auerbach et al., 2013). One such example is the State Innovation Model program sponsored by the Centers for Medicare & Medicaid Services (CMS) Center for Medicare & Medicaid Innovation to propose and implement novel integrated approaches to achieve the three elements of the Triple Aim, including improved population health. [Information about the CMS State Innovation Models Initiative is available at http://innovation.cms.gov/initiatives/state-innovations.]
Improving population health requires a coordinated strategy at multiple levels including individual provider practice, community, state, and national levels, with the community level recognized as an increasingly important locus of efforts (Hester et al., 2010). In a recent commentary, Stephen M. Shortell made a “bold proposal” to improve population health in which a community health management system would be paid a per capita budget for achieving specific quality and health status targets (Shortell, 2013). This proposal built on a number of other conceptual models that identified the need for an integrator function at the community level to mesh clinical care, public health programs and community-based initiatives in a coherent strategy to meet the community’s needs. This is the common denominator among several roughly analogous concepts Healthcare 3.0 (Halfon, 2012), Accountable Health Communities (Magnan et al., 2012), community integrators (Chang, 2012), community quarterbacks for community development (Erickson et al., 2012) and the “backbone organization” of the collective impact movement (Hanleybrown et al., 2012). These articles begin to identify the structure and functions of a community-level population health infrastructure that we will call a Community Health System (CHS). The CHS is accountable for the health of the population in a geographic area, including reducing disparities in the distribution of health. Its major functions include:
- convening a broad set of key stakeholders such as governmental public health agencies, communities, the health care delivery system, employers and businesses, and the education sector (IOM, 2012);
- reconciling diverse perspectives and defining a shared vision and goals;
- assessing the needs of the community, identifying gaps and potential interventions and prioritizing actions to achieve shared goals;
- managing a population health budget and allocating resources, and
- creating the information systems and capability to assess performance and implement rapid cycle changes.
The elusive “holy grail” for the population health movement has been a sustainable financial model that would break the cycle of dependence on limited-term grants and provide long term support for both infrastructure and interventions. What could be a sustainable financial model for a CHS? One part of the answer comes from the diverse set of new financial vehicles for financing population health interventions and infrastructure that have been emerging in recent years. These instruments fall into three broad categories: (1) new payment models for clinical services that reward Triple Aim outcomes instead of volume, (2) breaking down funding silos to create multi-sector programs that blend resources into a common pool, e.g., through a Medicaid Section 1115 waiver, and (3) a diverse set of innovative funding models that tap into new and existing pools of public and private capital (Cantor et al., 2013). Some examples include:
- new ACA requirements for non-profit hospitals to conduct Community Health Needs Assessments and adopt implementation strategies with specific resources to address priority needs;
- recognition of the connection between healthy populations and strong, economically vibrant communities opening the door to access Community Reinvestment Act vehicles such as Community Development Financial Institutions and Community Development Banks (Sprong and Stillman, 2014);
- the growing social capital movement, implementation of the first pay for success agreements (social impact bonds) and creation of new social mission corporate vehicles such as Low-Profit Limited Liability Companies;
- the use of Program Related Investments by philanthropic institutions as a complement to traditional grants; and
- the funding of Health and Wellness Funds at the state and local levels.
The diversity of interests, structures and objectives is valuable because it increases the likelihood that a given intervention will find a good match, however, it also raises the specter of fragmentation and conflicting efforts. The challenges and opportunities for improving population health vary widely from community to community. Achieving the goal of reduced disparities and better quality of life will require implementing a combination of interventions that are tailored to each community’s needs and that enhance each other, thus generating a community multiplier effect. Simply implementing an uncoordinated series of interventions is unlikely to be either effective or sustainable.
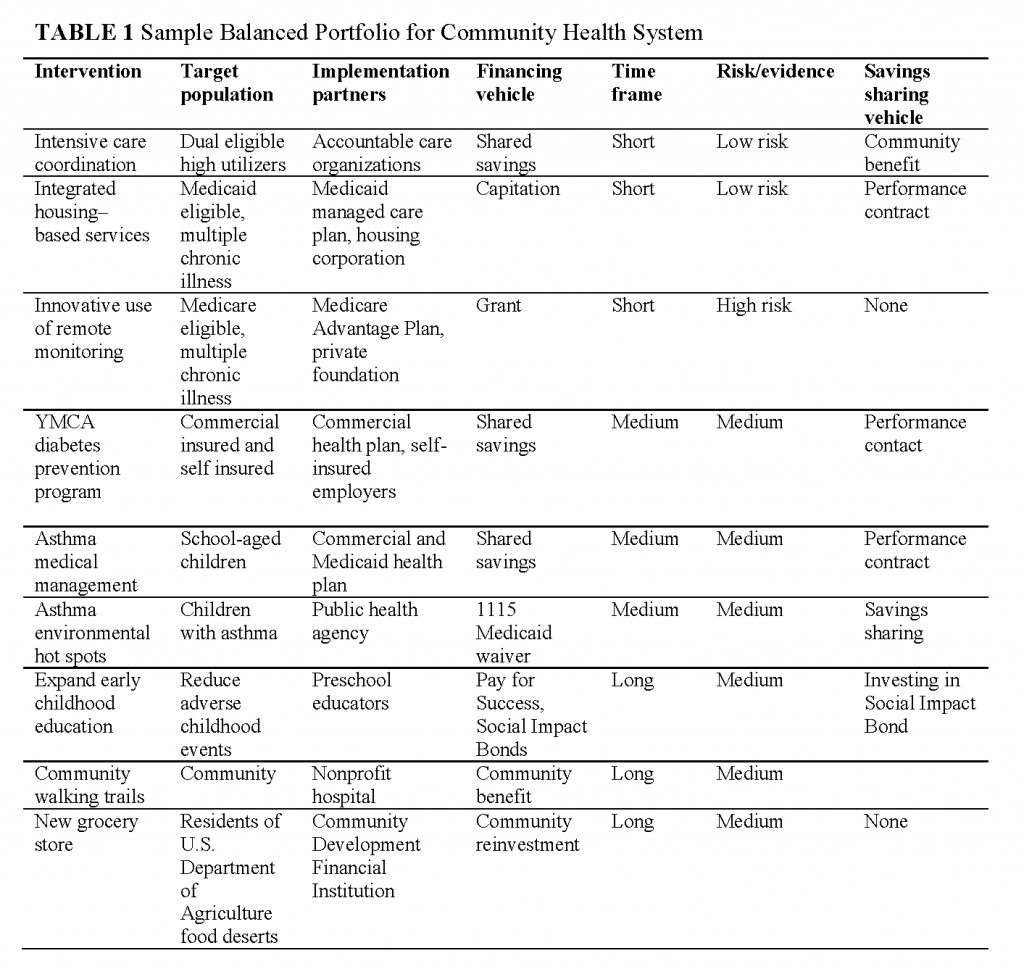
To avoid this, the CHS would use a solid grounding in the determinants of health to create and manage a portfolio of interventions that is balanced along the full spectrum of three perspectives: (1) time frames for effects of interventions, (2) the level of scientific evidence (investment risks) and (3) scale of return using both health and financial metrics. Table 1 illustrates how the CHS integrator organization would partner with other organizations to create a balanced portfolio that includes interventions with short, medium and long term impacts. Using its needs assessment process, it would prioritize interventions and combine them into a coherent strategy that realized short term opportunities for savings in medical costs, implemented medium-term interventions for changing risky behaviors and addressed longer-term upstream determinants of health such as early childhood development and the built environment. For each intervention, the CHS would identify an implementation partner with the appropriate skills (as well as a financing vehicle), facilitate the connection, and provide oversight to monitor results. In many cases, the CHS would also play a key role in identifying and securing financing. The more innovative financing vehicles are transaction-driven. Just as securing a mortgage on a house is specific to the particular owner of a specific house, closing on financing for a given intervention would be based on a specific intervention managed by a specific service provider in a specific place. Closing each deal would require a thorough feasibility study that documents both the business case of the financial flows and the capabilities of the organizations involved. Matching the time horizon, risk profile and returns of each intervention with the appropriate organization and financing vehicle, negotiating the agreement governing the relationship, and monitoring performance would be critical responsibilities of the CHS. These have not been identified previously as essential functions for population health improvement.
The sample portfolio in Table 1 shows the intervention, target population, implementation partner, financing vehicle, time horizon and risk profile for nine interventions targeted to address the needs of a hypothetical community. The combination covers a broad cross-section of the population and represents complementary efforts to improve the management of chronic illnesses, support changes in risky behaviors and change upstream determinants of health such as the built environment.
A key component of each intervention is identifying an explicit way in which the CHS could share in the savings generated by a successful intervention. Modeling of a variety of population health strategies has indicated that for the community to be able to sustain a balanced portfolio over time, the CHS must capture a portion of the savings and keep them available for reinvestment (Milstein et al., 2011). Different financing vehicles would provide different options for the CHS to capture savings. In short term initiatives using shared savings payment models or capitation, the CHS could negotiate receiving a percentage of savings which the provider organization could classify as a community benefit. At the other end of the spectrum, the CHS could use its Health and Wellness Fund to participate as an investor in a pay for success agreement and capture savings as its investment is repaid. The CHS share from each intervention flows into its Health and Wellness Fund. Initially, the CHS would have to be supported by startup grants and investments, but as its portfolio grows and matures, it would shift to support primarily from shared savings. In each case, the CHS would have to demonstrate a clear added value to the transaction to justify its sharing in the results. Understanding the specific ways it could do this is an area in which we have much to learn.
The financial model presented here is conceptual, not based on current experience. Although a variety of examples of community-based structures for improving the health of the population exists, no single organization has either the full range of competencies required for the integrator organization as described here, or the accountability to manage a broad spectrum of interventions with shared savings flowing to a Health and Wellness Fund. The next 3-5 years will be an important period of experimentation and development to translate this concept into a scalable reality. The timing is critical for a number of reasons. First, the innovative financing vehicles appear poised to develop and spread very rapidly with little, if any, focus on coordination with other population health initiatives in the community. This creates the very real danger that they will outrun our ability to create community-based structures to integrate them effectively to meet local needs. Second, there is not an unlimited pool of potential savings to be harvested and once the savings are gone, it will be more difficult to create a balanced portfolio. Third, the community development and population health movements are evolving on parallel tracks in creating community integrator structures. The last thing we need is to have dueling community infrastructure.
The State Innovation Models program created by CMS will provide a major opportunity for states to help test alternative approaches to a community integrator. The Transformation Plans of several states such as Washington and Minnesota explicitly call for the development of CHS’s and other states, such as Oregon, Colorado and Maryland are creating a regional accountability framework that could be a starting point for a CHS. Learning collaboratives such as the Robert Wood Johnston Foundation’s Aligning Forces for Quality and the Institute for Healthcare Improvement’s Triple Aim Collaborative, are other promising sources for early adopter organizations. It is essential that the public sector and private foundations combine resources to test how to create sustainable financial models and community-level infrastructure to support and reward improvements in the health of the population. Without them we will not be able to maintain the hard-won gains in expanding coverage for millions of Americans, or improve their health status.
References
- Auerbach, J., D. I. Chang, J. Hester, and S. Magnan. 2013. Opportunity knocks: Population health in State Innovation Models. NAM Perspectives. Discussion Paper, National Academy of Medicine, Washington, DC. https://doi.org/10.31478/201308d
- Berwick, D. M., T. W. Nolan, and J. Whittington. 2008. The Triple Aim: Care, health, and cost. Health Affairs 27(3):759-769. https://doi.org/https://doi.org/10.1377/hlthaff.27.3.759
- Cantor, J., L. Mikkelsen, B. Simons, and R. Waters. 2013. How can we pay for a healthy population? Innovative new ways to redirect funds to community prevention. Oakland, CA: Prevention Institute. Available at: https://www.preventioninstitute.org/publications/how-can-we-pay-healthy-population-innovative-new-ways-redirect-funds-community (accessed May 26, 2020).
- Chang, D. 2012. Integrator role and functions in population health improvement initiatives. Nemours. Available at: http://www.improvingpopulationhealth.org/Integrator%20role%20and%20functions_FINAL.pdf (accessed November 27, 2013).
- Erickson, D., I. Galloway, and N. Cytron. 2012. Routinizing the extraordinary. Investing in what works for America’s communities. Available at: http://www.whatworksforamerica.org/the-book (accessed November 27, 2013).
- Halfon, N. 2012. Transforming the child health system: Moving from Child Health 2.0 to 3.0. Aspen Institute’s Children’s Forum presentation, July 23. Available at: http://www.aspeninstitute.org/sites/default/files/content/docs/psi/TransformingtheChildHealthSystem-HalfonNeal.pdf (accessed November 27, 2013).
- Hanleybrown, F., J. Kania, and M. Kramer. 2012. Channeling change: Making collective impact work. Stanford Social Innovation Review. Available at: http://partnership2012.com/download/Collective%20Impact%20II.pdf (accessed November 27, 2013).
- Hester, J. A. 2013. Paying for population health: A view of the opportunity and challenges in health care reform. NAM Perspectives. Commentary, National Academy of Medicine, Washington, DC. https://doi.org/10.31478/201309c
- Hester, J., J. Lewis, and A. McKethan. 2010. The Vermont Accountable Care Organization Pilot: A community health system to control total medical costs and improve population health. Commonwealth Fund, 1-22. Available at: http://www.commonwealthfund.org/~/media/Files/Publications/Fund%20Report/2010/May/1403_Hester_Vermont_accountable_care_org_pilot.pdf (accessed November 1, 2013).
-
Institute of Medicine. 2012. For the Public’s Health: Investing in a Healthier Future. Washington, DC: The National Academies Press. https://doi.org/10.17226/13268
- Magnan, S., E. Fisher, D. Kindig, G. Isham, D. Wood, M. Eustis, C. Backstrom, and S. Leitz. 2012. Achieving accountability for health and health care. Minnesota Medicine 95(11):37-39. Available at: https://pubmed.ncbi.nlm.nih.gov/23243752/ (accessed May 26, 2020).
- Milstein, B., J. Homer, P. Briss, D. Burton, T. Pechacek. 2011. Why behavioral and environmental interventions are needed to improve health at lower cost. Health Affairs 30(5):823-832. https://doi.org/10.1377/hlthaff.2010.1116
- Shortell, S. M. 2013. A Bold Proposal for Advancing Population Health. NAM Perspectives. Discussion Paper, National Academy of Medicine, Washington, DC. https://doi.org/10.31478/201308a
- Sprong, S., and L. Stillman, 2014. Leveraging multi-sector investments: New opportunities to improve the health and vitality of communities. Health Resources in Action. Available at: http://hria.org/uploads/reports/PPReport_r3_011614_pages.pdf (accessed November 27, 2013).