Care Transformation at Emory Hospital
The Institute of Medicine’s (IOM’s) release of the reports To Err is Human and Crossing the Quality Chasm in 1999 and 2001, respectively, were markers of a tipping point in U.S. health care. Prior to that time, “quality” in health care had largely been defined by innovation and cutting-edge diagnostic and therapeutic interventions. The challenge issued by these IOM reports and the “quality movement” in general was to continue such innovations, but at the same time to markedly improve the reliability and safety of the delivery of the more routine elements of care. Central to the new dogma was a growing appreciation that the limits of human performance are such that high-reliability care cannot be based on a model of individual perfection, but rather requires an approach built on highly effective teamwork and intentional process redesign. While tools ranging from simple checklists to sophisticated disciplines such as Six Sigma and Lean can be extremely helpful, culture plays a central role in achieving these goals.
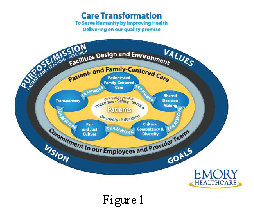
Our experience at Emory is illustrative, where, during the past decade Emory Healthcare initially focused on two key attributes of a culture of quality—transparency and disclosure, and a fair and just culture. Transparency and disclosure, of both data and individual errors, must occur to meaningfully surface the gap between actual performance and desired performance. Fair and just culture then addresses this gap in terms of inadequate system design and coaching failures, rather than reckless behavior. Emory Healthcare’s cultural framework, the Care Transformation Model, is growing organically, building on this foundation with the addition of three additional attributes—shared decision making, cultural competency and diversity, and patient- and family-centered care—all joined by teamwork around the Emory Healthcare quality promise of impeccable outcomes delivered safely with excellent service.
The results seem to be showing. The University HealthSystem Consortium (UHC), comprising the majority of academic medical centers in the United States, initiated its “Quality & Accountability Scorecard” in 2005, which also identified important cultural characteristics. [1] Judging this scorecard to be the best quality benchmarking system currently available, our leadership in 2006 set the goal of top-decile performance on this scorecard by 2012. At the time, Emory’s two participating hospitals’ composite rankings on this scorecard were 59 and 71, respectively, out of 81 hospitals then participating.
Anchoring efforts around the Care Transformation Model, Emory Healthcare embarked on an active program to spread and engrain the model through mandatory training, organizational storytelling, and other diffusion techniques, including ubiquitous use of a graphic model (Figure 1). With culture transformation as the leading wedge, the same two hospitals that were ranked 59 and 71 in 2006 were ranked 10 and 11 on the 2011 UHC scorecard.
While Donabedian postulated in 1980 [2] that outcomes result from process and structure, we believe that culture is an even more important determinant. Intentional “redesign” of culture can be accomplished and is necessary for breakthrough improvements in the quality of care.
References
- Keroack, M. A., B. J. Youngberg, J. L. Cerese, C. Krsek, L. W. Prellwitz, and E. W. Trevelyan. 2007. Organizational Factors Associated with High Performance in Quality and Safety in Academic Medical Centers. Academic Medicine 82:1178–1186. https://doi.org/10.1097/ACM.0b013e318159e1ff
- Donabedian, A. Explorations in quality assessment and monitoring: The definition of quality and approaches to its assessment. Ann Arbor, MI: Health Administration Press; 1980.