Patient-Centered, Integrated Health Care Quality Measures Could Improve Health Literacy, Language Access, and Cultural Competence
ABSTRACT | The authors of this paper recommend the integration of health care quality improvement measures for health literacy, language access, and cultural competence. The paper also notes the importance of patient-centered and equity-based institutional performance assessments or monitoring systems. The authors support the continued use of specific measures such as assessing organizational system responses to health literacy or the actual availability of needed language access services such as qualified interpreters as part of overall efforts to maintain quality and accountability. Moreover, this paper is informed by previous recommendations from a commissioned paper provided by the National Committee for Quality Assurance (NCQA) to the Roundtable on Health Literacy of the National Academies of Sciences, Engineering, and Medicine. In the commissioned paper, NCQA explained that health literacy, language access, and cultural competence measures are siloed and need to generate results that enhance patient care improvements. The authors suggest that the integration of health literacy, language access, and cultural competence measures will provide for institutional assessment across multiple dimensions of patient vulnerabilities. With such integration, health care organizations and providers will be able to cultivate the tools needed to identify opportunities for quality improvement as well as adapt care to meet diverse patients’ complex needs. Similarly, this paper reinforces the importance of providing more “measures that matter” within clinical settings.
Introduction
The first section of this paper explains the need for a patient-centered and equity-based institutional performance assessment or monitoring system. The second section outlines the NCQA’s recommendations for an integrated measure of health literacy, cultural competence, and language access within future organizational performance assessments. The NCQA work was commissioned by the Roundtable on Health Literacy of the National Academies of Sciences, Engineering, and Medicine [1]. The third section explores some existing initiatives from the federal government, national health care quality organizations, and national health care leadership organizations that might benefit from the use of an integrated measure of health literacy, language access, and cultural competence.
Background
The provision of high-quality care has long been a goal of the medical care system. Yet a 2000 report from the Institute of Medicine (IOM), To Err Is Human, documented that as many as 98,000 Americans die each year as a result of medical errors, and many more thousands experience nonfatal injuries [2]. In Crossing the Quality Chasm: A New Health System for the 21st Century, the IOM report committee concluded that health care safety and quality problems required a redesigned health care system [3]. That IOM report committee recommended six aims for improvement: health care should be safe, effective, patient-centered, timely, efficient, and equitable. In this paper, we focus specifically on two of those aims: health care that is patient-centered and equitable. Being patient-centered means “providing care that is respectful of and responsive to individual patient preferences, needs, and values and ensuring that patient values guide all clinical decisions” [3]. Equitable care means “providing care that does not vary in quality because of personal characteristics such as gender, ethnicity, geographic location, and socioeconomic status” [3].
Yet we know that health care is not equitable or patient-centered. There are significant disparities in health care and health outcomes as documented by the IOM in its report Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care [4]. That report committee found that “[R]acial and ethnic minorities tend to receive a lower quality of healthcare than non-minorities, even when access-related factors, such as patients’ insurance status and income, are controlled.” Among the many report recommendations for action needed to eliminate disparities are those that emphasize equity and patient-centered care:
- Support the use of interpretation services where community need exists;
- Implement patient education programs to increase patients’ knowledge of how to best access care and participate in treatment decisions;
- Integrate cross-cultural education into the training of all current and future health professionals;
- Collect and report data on health care access and utilization by patients’ race, ethnicity, socioeconomic status, and, where possible, primary language; and
- Monitor progress toward the elimination of health care disparities.
Reducing disparities requires attention to the essential components of equitable, patient-centered, high-quality care—that is, to culturally and linguistically appropriate care as well as attention to health literacy. Low health literacy disproportionately affects racial and ethnic minorities and contributes to health disparities. It should be noted, however, that challenges of health literacy affect all segments of the population. According to the Department of Health and Human Services (HHS), “The primary responsibility for improving health literacy lies with public health professionals and the health care and public health systems. It is imperative to ensure that health information and services can be understood and used by all Americans. We must engage in skill building with health care consumers and health professionals” [5]. A 2009 IOM workshop reported that “Integrating quality improvement, health literacy, and disparities reduction emphasizes the intersection of the patient-centered and equitable aims” [6].
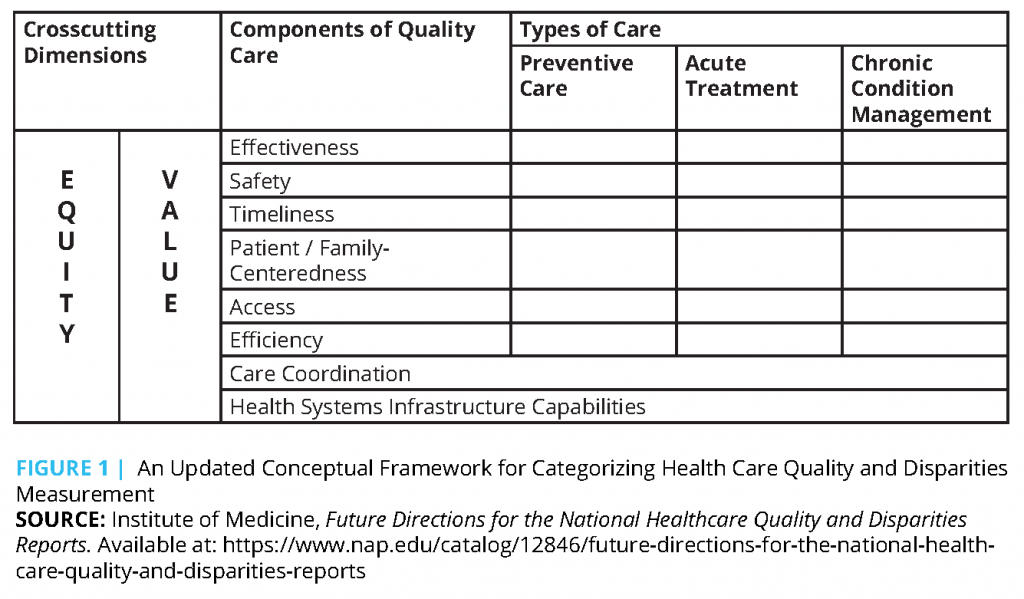
Tracking our progress in providing equitable, patient-centered care requires a monitoring system that can give feedback that helps us evaluate how well we are doing. In the IOM report Future Directions for the National Healthcare Quality and Disparities Reports [7], an updated framework is provided for measuring health care quality and disparities (see Figure 1) that continued the trend of highlighting the importance of equitable, patient-centered, high-quality care.
A review by Claxton and colleagues of current measures of health care system quality suggested that the quality of health care in the United States is improving in many areas, though it still lags behind comparable countries on a number of key measures, and the gap in health outcomes seems to be growing [8].
A 2016 IOM workshop reported: “Increasing health equity and reducing health disparities requires aligning health care system demands and complexities with individual skills and abilities, and such alignment requires attention to the integration of health literacy, culture competency and language access services” [9]. Health literacy, cultural competence, and language access interventions often are suggested approaches to delivering high-quality health care. They are inextricably linked, yet it is challenging to rigorously assess how these three domains contribute to improved health equity, reduction of health disparities, and patient-centered high-quality care.
Integrated approaches to fulfilling the aspirations of a monitoring system have yet to be developed, perhaps as a result of real and anticipated burdens in doing so. As we move forward toward a performance- and outcomes-based system of care, classic feedback loops in the form of metrics would be required to achieve the aims of equitable, high-quality, patient-centered care. A failure to implement such metrics would represent an abdication of our collective responsibility to engage and deliver high-quality care.
The concepts of health literacy, language access, and cultural competency have developed from separate theories and varying stakeholder perspectives. This has led to an understandably fragmented approach to any type of measurement in this space. Each concept has developed via differing histories that emphasize different aspects of care and with patient subgroups and goals that may not or do not overlap. More specifically, language access and cultural competency efforts focus on racial, ethnic, or linguistic minorities, whereas health literacy efforts target a broad array of patients to improve quality. These distinct histories, despite shared commonalities and linked concepts, have resulted in a fragmented approach to measurement with diverse approaches and multiple quality metrics that challenge implementation efforts during a time when reporting burden has been claimed as a significant obstacle. Consolidating this fragmented approach and ensuring that it is measuring the aspects of care that matter in improving health literacy, language access, and cultural competency is critical to delivering an appropriate standard of care to all Americans.
Description of Commissioned Paper
The development of integrated quality performance measures for three domains—health literacy, language access, and cultural competence—was proposed at a 2015 workshop of the Roundtable on Health Literacy of the National Academies of Sciences, Engineering, and Medicine [9].
The Roundtable commissioned the National Committee for Quality Assurance (NCQA) to prepare a paper that would (1) identify measures of quality performance that assessed the three domains, (2) note any linkage or integration of the three domains, and (3) describe how the measures could be used to improve health care quality and the patient-consumer experience of care—especially among diverse and at-risk populations. NCQA’s initial findings and recommendations were presented at a May 2017 workshop. In response to suggestions of workshop participants, NCQA revised its paper. The following section briefly describes the highlights of that revised paper [1].
State of Measures of Health Literacy, Language Access, and Cultural Competence
Initially, NCQA suggested that health literacy, language access, and cultural competence initiatives are potential cornerstones for higher-quality care among diverse and at-risk populations at the nation’s hospitals and medical centers. NCQA noted that initiatives such as communicating with patients in their preferred language, providing health information in diverse multimedia formats, using teach-back/interactive strategies with patients, the participation of community health workers, and tailoring health information to a patient/caregiver’s literacy level are associated with improved health outcomes and behaviors. NCQA concluded that implementing more health literacy, language access, and cultural competence initiatives within the health care delivery system could contribute to improved health care in the United States—and that ensuring quality improvements might occur if these activities were assessed systematically.
Yet after a review of relevant self-assessment efforts within US health care organizations, NCQA found that only four measures evaluated health literacy, language access, or cultural competence services. Three of these four measures did not focus on patient care and instead evaluated some characteristics of extant health plans, such as the diversity of plan members and the availability of language assistance within a health plan.
NCQA found only one existing measure that partially assessed health literacy initiatives to patients within a health care setting. In addition, NCQA noted they were unable to find an evaluation instrument that simultaneously assessed health literacy, patient/caregiver language access needs, and cultural competence initiatives provided to diverse, at-risk, or other populations within health care settings. In turn, NCQA encouraged the development of an integrated measure of health literacy, language access, and cultural competence to demonstrate improved health care outcomes. NCQA suggested the diffusion of a more multidimensional instrument as a mechanism to boost the implementation of needed assessments of at-risk, diverse, and other patient initiatives.
Implementing a Broader Measure of Health Literacy, Language Access, and Cultural Competence: Barriers and Strategies
Conversely, NCQA acknowledged that the latter recommendations occur at a time when health care organizations are beset by proliferating measures of quality as well as complaints about a misalignment of measures. The latter barriers are coupled with a challenging, rapid expansion to payment models that are value-based, which changes the procedures under which health care organizations are paid by public and private health insurers.
As a result, NCQA suggested that an integrated measure might be more warmly received if it was part of a broader strategy to enhance patient-centered care (and its evaluation) within health care organizations.
Specifically, the NCQA paper proposed a broader patient-centered framework intended to address seven domains within health care organizations. The suggested evaluation domains are a health care organization’s:
- measures of health organizational culture/values;
- accountability and quality improvement efforts;
- workforce skills;
- assessment plans;
- community engagement activities;
- communication initiatives; and
- patient engagement efforts.
Subsequent Clarifications and Recommendations
To clarify, the authors of this paper suggest that the principles of patient-centered care include respect for patients’ values, preferences, and expressed needs; coordination and integration of care; and providing emotional support alongside the alleviation of fear and anxiety associated with clinical care. Similar to the NCQA report, the authors of this paper agree that patient-centered care initiatives are a parallel and possibly underlying dimension of health literacy, language access, and cultural competence efforts in that patient-centered health initiatives are associated with beneficial health outcomes, including improved patient experience, safety, and clinical effectiveness.
The authors of the current paper also agree that a more integrated approach would help mitigate the conceptual confusion promulgated by measures that NCQA acknowledged are currently siloed and separate. For example, since limited English proficiency (LEP) patients are one of the groups with the lowest level of health literacy, it seems efficient and sensible to assess them within an integrated measure of both domains.
However, the authors of the current paper acknowledge that individual measures that identify specific patient quality-improvement needs can provide singular contributions. For example, it may be important for health care organizations to understand the sufficiency of language access services for LEP patients to pinpoint tailored solutions. An integrated measure may or may not be sufficiently granular to provide needed information. The authors suggest that a solution is to develop integrated measures with enough items to assess domains with empirical validity or retain some carefully selected, individual domain measures that are implemented along with integrated measures of health literacy, language access, cultural competence, and other patient-centered initiatives.
Finally, any approach to measures of health literacy, language access, and cultural competence should include specific strategies to reach diverse and at-risk populations. The authors of this paper enthusiastically endorse NCQA’s recommendations to develop packages of measures for vulnerable populations and to use specific strategies to achieve reasonable response rates.
Examples of Public and Private Quality Improvement Activities That Could Benefit from Using an Integrated Health Literacy, Language Access, and Cultural Competence Measure
Several current health care quality initiatives could implement integrated measurements of health literacy, language access, and cultural competence. The initiatives discussed below have been advanced by (1) the federal government and other payers, (2) national health care quality organizations, and (3) national health care leadership organizations.
Federal Government and Other Payers
Centers for Medicare and Medicaid Services Meaningful Measures Initiative
In 2017, the HHS Centers for Medicare and Medicaid Services (CMS) launched its Meaningful Measures initiative to identify the highest quality measurement and improvement priorities that are most important to improving patient outcomes [11]. The initiative seeks to respond to stakeholder feedback about the growing number of quality measures and the burden of quality measure reporting [12].
In identifying meaningful measures, the initiative will look for those that:
- address high-impact measure areas that safeguard public health;
- are patient-centered and meaningful to patients;
- are outcome-based where possible;
- fulfill requirements in programs’ statutes;
- minimize the level of burden for providers;
- provide significant opportunity for improvement;
- address measure needs for population-based payment through alternative payment models; and
- align across programs and/or with other payers (Medicaid, commercial payers).
CMS defines meaningful measures of equity of care as measures that “ensure high quality and timely care with equal access for all patients and consumers, including those with social risk factors, for all health episodes in all settings of care” [13]. Currently, the Meaningful Measures framework lists only stratification of the Hospital Readmission Reduction Program measures, Ambulatory Surgical Center Quality Reporting Program measures, and End-Stage Renal Disease Quality Incentive Program measures as potential meaningful measures for equity of care. Although the overall intent of the initiative is to reduce the number of measures, there have yet to be specific measures designated by CMS as meaningful measures of health equity and patient-centeredness.
An integrated measure of health literacy, language access, and cultural competence would meet the Meaningful Measures initiative’s principles of being patient-centered and meaningful to patients, and of minimizing the level of burden for providers. Such integrated measures would also be consistent with two of CMS’ overarching national quality strategies: to strengthen person and family engagement as partners in their care, and to promote effective communication and coordination of care. Although such an integrated measure of health literacy, language access, and cultural competence would not be the only measure that would address these strategies, goals, and principles, such an integrated approach is more likely to be adopted as part of the Meaningful Measures initiative than as separate measures in three separate domains.
CMS Quality Payment Program
CMS continues its implementation of the Quality Payment Program (QPP), created by the Medicare Access and Children’s Health Insurance Program Reauthorization Act (MACRA) of 2015, which shifts Medicare fee-for-service payments to physicians and other eligible providers to an increasing proportion of value-based payments [14]. The QPP’s Merit-based Incentive Payment System (MIPS) includes requirements for completing a certain number of Improvement Activities. Some of these Improvement Activities are identified as ones which would also assist in Achieving Health Equity. Currently, there are only four Achieving Health Equity Improvement Activities:
- Engagement of new Medicaid patients and follow-up;
- Leveraging a Qualified Clinical Data Registry (QCDR) for use of standardized questionnaires;
- Leveraging a QCDR to promote use of patient-reported outcome tools; and
- Leveraging a QCDR to standardize processes for screening [15].
Eligible providers can select from more than 90 Improvement Activities to complete. It has yet to be determined how many providers completed and reported on any of these four Achieving Health Equity Improvement Activities in MIPS.
In the future, integrated measures of health literacy, language access, and cultural competence could be proposed to, and adopted by, CMS as MIPS Improvement Activities [16]. CMS has described its criteria for consideration of new Improvement Activities as follows:
- Represents an area that could highlight improved beneficiary health outcomes, patient engagement, and safety based on evidence;
- Could reduce health care disparities;
- Would contribute to improvement in patient care practices or improvement in performance on quality measures and cost performance categories, or includes an emerging certified health IT capability;
- Does not duplicate existing improvement activities;
- May be considered for an Advancing Care Information bonus;
- Is feasible to implement; and/or
- Is able to be validated by CMS.
An integrated measure of health literacy, language access, and cultural competence could reduce health disparities, could highlight patient engagement, would contribute to improvement in patient care practices, and would not duplicate existing improvement activities. Including such an Improvement Activity in MIPS would be particularly important for safety net providers—such as federally qualified health centers and public hospitals and health systems, and solo and small group physician practices—to receive recognition for providing culturally and linguistically appropriate services to their diverse patient populations. These types of providers often have less organizational infrastructure to support quality improvement activities [17] and would benefit from elements in the QPP that provide credit and financial incentives for continuing to provide care that highlights the importance of health literacy, language access, and cultural competence.
Although these initiatives are from CMS, state and commercial payers could conduct similar activities to adopt and implement an integrated measure of health literacy, language access, and cultural competence. For example, many state Medicaid programs and commercial payers continue to develop and implement models of accountable care that share savings based on quality improvement and cost reduction targets [18].
National Health Care Quality Organizations
National Quality Forum Roadmap for Promoting Health Equity and Eliminating Disparities
In September 2017, the National Quality Forum (NQF), the leading endorser of health care quality measures through a national stakeholder consensus process, issued its Roadmap for Promoting Health Equity and Eliminating Health Disparities and launched its Health Equity Program [19, 20]. The Roadmap lays out four actions for promoting health equity and eliminating disparities:
- Identify and prioritize reducing health disparities;
- Implement evidence-based interventions to reduce disparities;
- Invest in the development and use of health equity performance measures; and
- Incentivize the reduction of health disparities and achievement of health equity.
Although NQF recognizes that the current volume of existing quality measures makes prioritization a challenge, NQF suggests that measures that can help monitor and reduce disparities should be prioritized. One of these measures suggests “adopting and implementing a culture of equity.”
Since the NQF Roadmap identifies health literacy, language access, and cultural competence as important topics for measurement, an integrated measurement approach would be aligned with the Roadmap’s call for prioritized measures to implement its proposed measurement framework. NQF describes its Health Equity Program as a broad portfolio of cross-cutting projects that put into action the guidance laid out by NQF’s substantive work in health equity. One of the goals of the program is to facilitate the development of needed measures to promote health equity and reduce health disparities. NQF’s Health Equity Program could facilitate the development and testing, and ultimately, the endorsement, of integrated measures of health literacy, language access, and cultural competence.
Institute for Healthcare Improvement Pursuing Equity Initiative
The Institute for Healthcare Improvement (IHI) could add an integrated measure of health literacy, language access, and cultural competence to its Pursuing Equity in Health Care Systems initiative [21]. This addition to IHI’s planned quality improvement activities could foster an evidence base that better documents overall progress to achieve health equity. IHI, a leading national organization supporting health care quality improvement, launched a two-year Pursuing Equity initiative with eight health care systems across the nation in 2017. The participating health care systems apply practical improvement methods and tools, spread ideas in peer-to-peer learning, and disseminate results and lessons to support an ongoing national dialogue to advance health equity. Specifically, an integrated measure could be tested as part of IHI’s Achieving Health Equity: A Guide for Health Care Organizations, which features five strategies [22]:
- Make health equity a strategic priority;
- Develop structure and processes to support health equity work;
- Deploy specific strategies to address the multiple determinants of health on which health care organizations can have a direct impact;
- Decrease institutional racism within the organization; and
- Develop partnerships with community organizations to improve health and equity.
Patient-Centered Outcomes Research Institute’s Healthcare Delivery and Disparities Research
An integrated measure of health literacy, language access, and cultural competence would add new dimensions to the Patient Centered Outcomes Research Institute’s (PCORI) evaluation activities. Such a patient-centered measure seems well aligned with PCORI’s interest in advancing an evidence base to assess patient-centered outcomes within health care settings.
In 2017, PCORI merged its Advisory Panels on Improving Healthcare Systems and on Addressing Disparities into one Advisory Panel on Healthcare Delivery and Disparities Research. The merger integrated PCORI’s research on health care disparities reduction with its assessment of quality outcomes within health care delivery systems [23]. The integration of PCORI’s research fosters new opportunities to test and use integrated measures of health literacy, language access, and cultural competence. Overall, PCORI has made significant investments to support shared decision-making, including interventions tailored for vulnerable populations. For example, 72 percent (89 of 124) of PCORI’s studies on shared decision-making have received participation from diverse racial and ethnic patient populations [24]. To date, PCORI also has funded 30 studies with low health literacy populations, but not all have involved shared decision-making processes [25]. Since there is a foundation to address patient literacy and the health of vulnerable populations within PCORI’s work, an integrated measure of health literacy, language access, and cultural competence could boost PCORI’s future assessment plans and overall activities.
National Health Care Leadership Organizations
American Hospital Association’s Institute for Diversity and Health Equity
An integrated measure of health literacy, language access, and cultural competence would enable a hospital or health system to establish baselines and evaluate progress as part of the American Hospital Association’s (AHA) renewed efforts to improve care to diverse patients and improve health equity. AHA’s commitment to revitalizing its prior equity and diverse care initiatives was underscored in a change in the name of the association’s efforts in 2018. AHA said that its renamed Institute for Diversity and Health Equity “more accurately depict[s] our mission now that we have realigned ourselves as a core membership resource within the AHA” [26].
Among the institute’s continuing activities will be boosting the signatories to its #123forEquity pledge and highlighting how member hospitals and health systems implement the pledge [27]. Under the pledge, launched in 2015, signatory hospitals and health systems commit to making organizational improvement in four areas:
- Increasing the collection and use of race, ethnicity, language preference, and other sociodemographic data;
- Increasing cultural competency training;
- Increasing diversity in leadership and governance; and
- improving and strengthening community partnerships.
Nearly 1,500 hospitals have signed the pledge [28]. An integrated measure of health literacy, language access, and cultural competence would help participating hospitals and health systems consider new activities to implement, and demonstrate their commitment to improving all three foundational care domains.
Families USA Call to Action for Health Equity Leaders
Families USA, a leading national health consumer organization, issued a 2017 Call to Action for Health Equity Leaders that recommends more health equity leadership in payment and other reforms within the health care delivery system [29]. The Call to Action concludes as follows:
We must work collaboratively to take the body of expertise and experience that has been developed on disparity-reducing, linguistically-accessible, and culturally-centered care. Together, we can create a shared national policy agenda that encompasses federal, state, and private policy recommendations, and a comprehensive action plan to advocate for those policy solutions that will enable our communities to achieve the best health possible.
In 2018, Families USA announced a Health Equity Task Force for Delivery and Payment Transformation. The task force will bring together leading experts and organizations to develop a national- and state-level policy agenda, and to provide recommendations to address persistent racial, ethnic, and geographic disparities [30]. The use of an integrated measure of health literacy, language access, and cultural competence provides a fresh strategy with which to assess improvements in health equity within delivery system and payment reforms.
Conclusion
The authors of this paper suggest that the adoption of an integrated measure of health literacy, language access, and cultural competence would enable hospitals and health systems, as well as health consumer leadership organizations, to address specific as well as broader patient-centered framework issues in health equity. Health care organizations could adopt pledges to act, as well as develop and test new assessment instruments. Certainly, an array of current initiatives by the federal government and other payers, national health quality organizations, and national health care leadership organizations provide timely opportunities for the adoption and use of an integrated measure of health literacy, language access, and cultural competence.
The overall goal of the quality movement is to improve care, but in the midst of developing and refining specific quality metrics, it can be easy to lose focus on the patient. Patients who would benefit from improved attention to health literacy, language access, and cultural competence are often overlooked in quality improvement. We support the continued use of specific measures, e.g., assessing organizational system responses to health literacy, or actual availability of needed language access services such as qualified interpreters, as part of overall efforts to maintain quality and accountability.
Moreover, we believe that by integrating measurement activities across multiple dimensions of vulnerabilities—that frequently exist in tandem—health care organizations and providers will gain the tools to identify opportunities for quality improvement, and adapt care to meet diverse patients’ complex needs. Such measures would advance the aims of both patient-centeredness and equity that have been elusive in many quality improvement efforts. The current policy and practice environment is calling for core measures, consideration of “all or none measures, and less measurement burden.” Using a patient-centered, integrated approach is consistent with the focus on concentrating on “measures that matter,” measures that will demonstrably improve patient care and outcomes. Such an integration approach would bring both cohesion and focus to improving the quality of care for our increasingly diverse patients.
Join the conversation!
![]() Tweet this! “Reducing disparities requires attention to the essential components of equitable, patient-centered, high-quality care – that is, to culturally and linguistically appropriate care as well as attention to health literacy.” https://doi.org/10.31478/201902a #NAMPerspectives
Tweet this! “Reducing disparities requires attention to the essential components of equitable, patient-centered, high-quality care – that is, to culturally and linguistically appropriate care as well as attention to health literacy.” https://doi.org/10.31478/201902a #NAMPerspectives
![]() Tweet this! In order to ensure our health care system is moving toward providing equitable, patient-centered care, we need a monitoring system that provides feedback and can evaluate our progress. Read more in our latest #NAMPerspectives: https://doi.org/10.31478/201902a
Tweet this! In order to ensure our health care system is moving toward providing equitable, patient-centered care, we need a monitoring system that provides feedback and can evaluate our progress. Read more in our latest #NAMPerspectives: https://doi.org/10.31478/201902a
![]() Tweet this! Health literacy, cultural competence, and language access are all critical factors in delivering high-quality care. Our latest #NAMPerspectives examines existing approaches we can utilize to ensure all 3 domains are addressed for all patients: https://doi.org/10.31478/201902a
Tweet this! Health literacy, cultural competence, and language access are all critical factors in delivering high-quality care. Our latest #NAMPerspectives examines existing approaches we can utilize to ensure all 3 domains are addressed for all patients: https://doi.org/10.31478/201902a
![]() Tweet this! Our approaches to measuring health literacy, cultural competence, and language access are fragmented. Authors of our newest #NAMPerspectives urge health care providers to unify all 3 in practice and in tracking/evaluation: https://doi.org/10.31478/201902a
Tweet this! Our approaches to measuring health literacy, cultural competence, and language access are fragmented. Authors of our newest #NAMPerspectives urge health care providers to unify all 3 in practice and in tracking/evaluation: https://doi.org/10.31478/201902a
Download the graphics below and share them on social media!
References
- French, J. B., S H. Scholle, J. Ng, and M. Taylor. 2017. Measuring improvement in the patient-consumer experience of health care: Aligning and leveraging measures of health literacy, language access and cultural competence. Paper commissioned by the Roundtable on Health Literacy. Available at: http://nationalacademies.org/hmd/~/media/Files/Activity%20Files/PublicHealth/HealthLiteracy/Commissioned%20Papers%20-Updated%202017/Briefer%20French%20et%20al%202017%20Measuring%20improvement%20in%20the%20patientconsumer%20experience%20of%20health%20care.pdf (accessed January 31, 2019).
- Institute of Medicine. 2000. To Err Is Human: Building a Safer Health System. Washington, DC: The National Academies Press. https://doi.org/10.17226/9728
- Institute of Medicine. 2001. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: The National Academies Press. https://doi.org/10.17226/10027
- Institute of Medicine. 2003. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: The National Academies Press. https://doi.org/10.17226/12875
- Office of Disease Prevention and Health Promotion. 2018. Quick guide to health literacy. Department of Health and Human Services. Available at: https://health.gov/communication/literacy/quickguide/factsbasic.htm (accessed January 31, 2019).
- Institute of Medicine. 2009. Toward Health Equity and Patient-Centeredness: Integrating Health Literacy, Disparities Reduction, and Quality Improvement: Workshop Summary. Washington, DC: The National Academies Press. https://doi.org/10.17226/12502
- Institute of Medicine. 2010. Future Directions for the National Healthcare Quality and Disparities Reports. Washington, DC: The National Academies Press. https://doi.org/10.17226/12846
- Claxton, G., C. Cos, S. Gonzales, R. Kamal, and L. Levitt. 2015. Measuring the quality of healthcare in the U.S. Petersen Kaiser Health System Tracker. Available at: https://www.healthsystemtracker.org/brief/measuring-the-quality-of-healthcare-in-the-u-s/?_sft_category=quality-of-care#item-start (accessed January 31, 2019).
- National Academies of Sciences, Engineering, and Medicine. 2016. Integrating Health Literacy, Cultural Competence, and Language Access Services: Workshop Summary. Washington, DC: The National Academies Press. https://doi.org/10.17226/23498
- MacLean, C. H., E. A. Kerr, and A. Qaseem. 2018. Time out–Charting a path for improving performance measurement. New England Journal of Medicine. https://doi.org/10.1056/NEJMp1802595
- Centers for Medicare and Medicaid Services (CMS). 2018. Meaningful measures framework. Available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/QualityInitiativesGenInfo/CMS-Quality-Strategy.html (accessed January 31, 2019).
- CMS. 2017. Core measures. Available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/QualityMeasures/Core-Measures.html (accessed January 31, 2019).
- CMS. 2018. Meaningful measures framework across CMS drawn from multiple national priorities and programs’ feedback. Available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/QualityInitiativesGenInfo/Downloads/MMF-Handout-2.pdf (accessed January 31, 2019).
- CMS. 2018. Quality payment program. Available at: https://qpp.cms.gov (accessed January 31, 2019).
- CMS. 2018. MIPS improvement activities. Available at: https://qpp.cms.gov/mips/improvement-activities (accessed January 31, 2019).
- CMS. n.d. Annual call for measures and activities: The quality payment program. Available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/MMS/Downloads/Annual-Call-for-Measures-and-Activities-for-MIPS_Overview-Factsheet.pdf (accessed January 31, 2019).
- Weinick, R. M., S. C. Byron, E. S. Han, J. B. French, and S. H. Scholle. 2010. Reducing disparities and improving quality: Understanding the needs of small primary care practices. Ethnicity & Disease 20(1):58-63. Available at: https://europepmc.org/article/med/20178184 (accessed September 2, 2020).
- Muhlestein, D., R. Saunders, and M. McClellan. 2017. Growth of ACOs and alternative payment models in 2017. Health Affairs Blog. Available at: http://www.healthaffairs.org/do/10.1377/hblog20170628.060719/full/ (accessed January 31, 2019).
- National Quality Forum (NQF). 2018. NQF issues quality roadmap for reducing healthcare disparities. Available at: https://www.qualityforum.org/NQFs_Roadmap_to_Health_Equity.aspx (accessed January 31, 2019).
- NQF. 2017. NQF launches multi-year program to improve health equity. Available at: https://www.qualityforum.org/News_And_Resources/Press_Releases/2017/NQF_Launches_Multi-Year_Program_to_Improve_Health_Equity.aspx (accessed January 31, 2019).
- Institute for Healthcare Improvement. 2018. Pursuing equity. Available at: http://www.ihi.org/Engage/Initiatives/Pursuing-Equity/Pages/default.aspx (accessed January 31, 2019).
- Wyatt, R., M. Laderman, L. Botwinick, K. Mate, and J. Whittington. 2016. Achieving health equity: A guide for health care organizations. IHI White Paper. Cambridge, MA: Institute for Healthcare Improvement. Available at: http://www.ihi.org/resources/Pages/IHIWhitePapers/Achieving-Health-Equity.aspx (accessed January 31, 2019).
- Patient-Centered Outcomes Research Institute (PCORI). 2017. Advisory panel on healthcare delivery and disparities research (HDDR). Available at: https://www.pcori.org/engagement/engage-us/pcoris-advisory-panels/advisory-panel-healthcare-delivery-and-disparities (accessed January 31, 2019).
- PCORI. n.d. Shared decision making. Available at: https://www.pcori.org/sites/default/files/PCORI-Research-Spotlight-Shared-Decision-Making.pdf (accessed January 31, 2019).
- PCORI. n.d. Addressing disparities. Available at: https://www.pcori.org/sites/default/files/PCORI-Research-Spotlight-Addressing-Disparities.pdf (accessed January 31, 2019).
- Tejeda, N. 2018. The imperative of diversity and health equity in our culture. American Hospital Association Insights and Analysis. Available at: https://www.aha.org/news/insights-and-analysis/2018-02-08-imperative-diversity-and-health-equity-our-culture?utm_source=newsletter&utm_medium=email&utm_content=02082018-at-pub&utm_campaign=aha-today (accessed January 31, 2019).
- American Hospital Association (AHA). 2018. #123forEquityCampaign to eliminate health care disparities. Available at: http://www.equityofcare.org (accessed January 31, 2019).
- AHA. 2017. AHA national call to action partners. Available at: http://www.equityofcare.org/pledge/resources/EOC_Pledge_Packet_Aug2017_FINAL.pdf (accessed January 31, 2019).
- Hernández Cancio, S. 2017. A call to action for health equity leaders: Health care transformation efforts must include strong focus on health equity. Available at: http://familiesusa.org/sites/default/files/product_documents/Health-Equity-and-Value-Call-to-Action_brief_final.pdf (accessed January 31, 2019).
- Families USA. 2018. Families USA joins diverse partners in launching health equity task force to leverage health system reform to address persistent health disparities. Available at: http://familiesusa.org/press-release/2018/families-usa-joins-diverse-partners-launching-health-equity-task-force-leverage (accessed January 31, 2019).