Patient and Family Engaged Care: An Essential Element of Health Equity

ABSTRACT | In this paper, we emphasize and explore health equity as an integral component of a culture of patient and family engaged care (PFEC), rather than an isolated or peripheral outcome. To examine the role of PFEC in addressing health inequities, we build on the 2017 NAM Perspectives discussion paper “Harnessing Evidence and Experience to Change Culture: A Guiding Framework for Patient and Family Engaged Care.” Informed by both scientific evidence and the lived experience of patients, their care partners, practitioners, and health system leaders, the paper by Frampton et al. introduced a novel Guiding Framework that delineates critical elements that work together to co-create a culture of PFEC, while also depicting a logical sequencing for implementation that facilitates progressive change and improvement toward the Quadruple Aim outcomes of better culture, better care, better health, and lower costs. In this paper, the authors highlight the need to integrate addressing health and health care disparities and improving health equity as core components of the framework to ensure the culture and policy changes necessary to meaningfully engage patients, health system staff, families, and communities.
Introduction
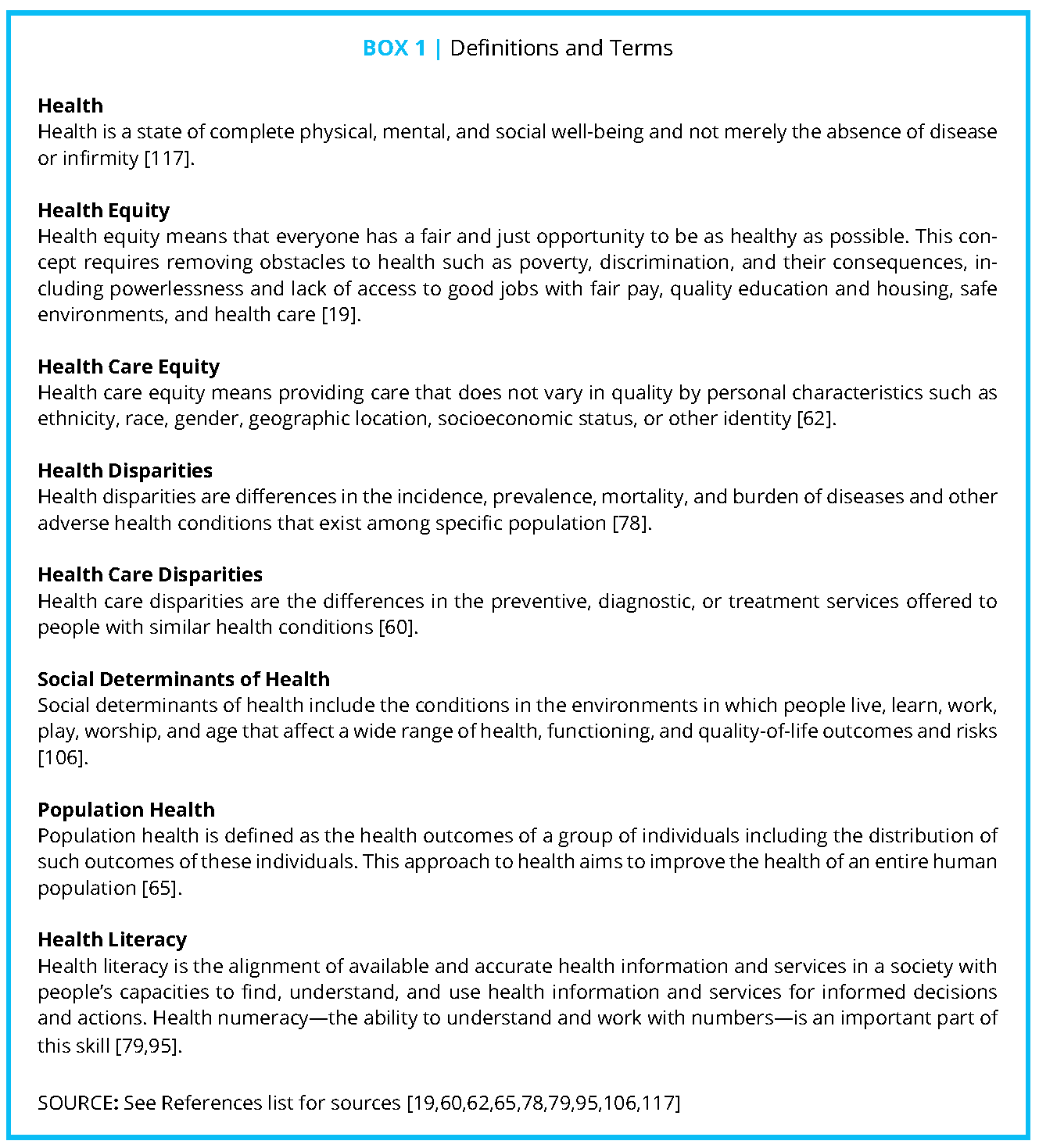
Health equity is emerging as an important topic for health care organizations, hospitals, clinics, providers, and their practices, due in part to policy changes at the federal and state levels, as well as new incentives to address the health of all populations. Despite efforts thus far, health and health care disparities persist, manifesting in poor health care system performance and subpar health outcomes [20,46,106]. Moreover, these inequities are not specific to individuals but affect groups of people, making it necessary to shift toward a population health approach that aims to reduce and eliminate health and health care inequities. Inequities in health and health care affect vulnerable populations across a spectrum of characteristics such as race; ethnicity; socioeconomic status; insurance status; incarceration status; geographic location; age; education; language or limited English proficiency (LEP); citizenship status; literacy, numeracy, or digital skills; religion/beliefs; health status; disability; and/or sexual orientation or gender identity (SOGI). While this is not designed to be an exhaustive list of all characteristics that result in disparities, it includes categories that are frequently associated with poor health outcomes [5,25,73]. It is estimated that eliminating health and health care disparities could save the United States approximately $230 billion in direct medical care expenditures [67]. The authors of this paper believe that improved population health, which is becoming the new fundamental premise of health care delivery today, cannot be achieved without progress toward a culture of patient and family engaged care (PFEC) that ensures all populations (and members within populations) have equitable opportunities to achieve and maintain health. See Box 1 for definitions of terms used in this paper.
The NAM Perspectives discussion paper, “Harnessing Evidence and Experience to Change Culture: A Guiding Framework for Patient and Family Engaged Care,” presents a vision for the role of PFEC in addressing the Quadruple Aim, which focuses on better care, culture, and health, and lower costs (see Figure 1) [49]. This Guiding Framework draws on the work of a scientific advisory panel that, over the course of more than a year, compiled important findings and insights on aspects of PFEC with validated results tied to the Quadruple Aim. The Guiding Framework that resulted from those discussions is designed to lay out specific practices and approaches to implement the panel’s insights is presented below.
The Guiding Framework includes core elements that align with each transformational stage of PFEC. The starting organizational foundations of leadership and levers for change represent the necessary underpinnings for creating a culture of PFEC. The next core element of strategic inputs are the needed structures, skill and awareness building, connections, and practices and represent the interventions and tactics that should be used to obtain the desired outcomes. The practice outputs of better engagement, better decisions, better processes, and better experience are shorter-term results that depict the direct results of implementing the inputs. The ultimate aim of the framework is the engagement outcomes of the Quadruple Aim: better culture, better care, better health, and lower costs. Surrounding the organizational foundations, strategic inputs, and practice outcomes are elements related to data collection, continuous feedback, increasing co-creation, and monitoring. The Guiding Framework indicates that reduced disparities occur only once the organizational foundations, inputs, and outputs are aligned with PFEC.
Nonetheless, although “reduced disparities” is highlighted as a key outcome under the heading of “Better Care,” “health equity” is not featured as a continuous or underlying goal in the Guiding Framework. We aim to rectify that gap in this paper. The framework presumes that those implementing a culture of PFEC will foster equity by reaching and improving health for all. Here, we posit that health equity will not organically emerge from PFEC, but must be an explicit priority and foundational element when implementing the Guiding Framework. Specifically, we argue that efforts to reduce disparities and drive toward the promotion of health equity must be purposefully and overtly built into the intent, structure, and function of all the elements identified in the Guiding Framework, including organizational foundations, strategic inputs, practice outputs, monitoring, data collection, increasing co-creation, and continuous feedback.
In this paper, we will explore recent efforts that have created new levers for change on the policy and cultural levels, and promising approaches in PFEC that may be scalable to deliver the transformative change needed for a cultural shift to health equity. Finally, we stress that a culture of PFEC must include all—in representation, participation, and the culmination of equitable outcomes—regardless of race; ethnicity; socioeconomic status; insurance status; incarceration status; geographic location; age; education; language or LEP; citizenship status; literacy, numeracy, and digital skills; religion/beliefs; health status; disability; and/or SOGI.
Social and Structural Inequities and the Challenge of Addressing Health and Health Care Inequities in the Health Care System
Health care leaders and policymakers increasingly acknowledge that social determinants, such as poverty, poor quality housing, and inadequate transportation infrastructure, negatively affect health and health care outcomes [98,73]. It is widely recognized that societal structures, governmental policies, and history are immensely impactful on health and health care [46].
These structural inequities result in two challenges for the health care system. See Box 2 for definitions of structural factors that influence health and health care. The first challenge is that people served by health care systems arrive with health conditions created or worsened by structural and social inequities or vulnerabilities. The prevalence, incidence, and burden of disease for conditions such as diabetes, cardiovascular disease, asthma, and depression are often worse for the vulnerable populations described above [5,25,69,111]. For example, adults with disabilities report higher rates of obesity, smoking, and lack of physical activity, and are three to four times more likely to have cardiovascular disease compared to those without disabilities [73]. Yet, the health care system is ultimately responsible for taking care of these and other groups who experience health disparities. As health financing moves from fee-for-service toward value and population health, care should be tailored to meet the needs of those whose health is negatively impacted by factors outside of the health care system.
In addition, a lack of access to quality care can exacerbate existing health disparities. The Agency for Healthcare Research and Quality’s 2016 National Healthcare Quality and Disparities Report (QDR) detailed that people with low incomes (at or below 100% of the Federal Poverty Level [FPL]) experienced worse access to care compared with high-income people (400% or more of FPL) for almost all access measures [5]. Moreover, in terms of access to health insurance, the 2018 uninsured rate for children under age 18 living in poverty was 6.4%, versus the 4.2% uninsured rate for children not living in poverty [5]. In 2018, the uninsured rates for non-Hispanic Whites was 8.1%, Hispanics 26.7%, African Americans 15.2%, and Asians 9% [4,97]. Addressing the challenges of health disparities requires a strong understanding of the structural elements and biases that caused them and consideration of how the health care system can address these barriers to overall health.
The second challenge that results from structural inequities is that the system itself has historically, even if unintentionally, contributed to inequities in care and outcomes [14]. For example, consistently significant disparities exist across low-income, uninsured, and racial/ethnic minority populations in all priority areas as reported in the QDR [4,5]. The 2018 version of the report details some improvement since the 2016 report was published, but minority populations continue to receive consistently worse care compared to Whites [5]. The disparate treatment varies by ethnic group; in the 2018 report, African Americans received worse care on 40% of measures and Hispanics on 35% of measures compared to Whites [5]. For example, in 2016, the rate of potentially avoidable hospital admissions with hypertension for African Americans was 156.1 per 100,000 population compared the rate of 37.6 per 100,000 population for Whites. This disparity increased from 2001 to 2015, although it dropped slightly in 2016 [5]. The Institute of Medicine’s 2003 Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care report identified a number of disparities in the receipt of appropriate care for African Americans compared to Whites [63]. Similarly, a 2012 meta-analysis of 34 articles identified a significant disparity in the way that pain, both acute and non-traumatic/non-surgical, is treated in minority populations [70]. Studies included in the analysis indicate that minorities, including African Americans and Hispanics, received inadequate treatment, and minorities did not receive guideline-recommended care [70]. While efforts have been made to address these and other health care disparities experienced by racial/ethnic minorities, these are not the only groups that experience disparities in health care. For example, in 2017, rural residents with diabetes enrolled in Medicare Advantage were significantly less likely than urban residents to have had an HbA1c test and eye exam in the past year [29]. Without a focus on structural inequities in the system, it will be difficult to improve the nation’s health as a whole.
The Population Health Imperative: Connecting Values, Strategy, and Action with Health Equity at the Core
Health care organizations’ responsibilities to achieve transformative culture change to address inequities must start with how they frame and then operationalize population health. From that fundamental premise, this deep-level change will be driven by a number of external levers and will encompass a range of strategic inputs. These efforts take many shapes that include promoting a culture of inclusion, engagement of diverse communities, place-based investment, and technology use to democratize health care delivery and decision making. As a property of organizational culture, health equity goals would be embedded in strategic plans; hiring and contracting practices ensure that a diverse workforce reflects the populations served; funding is allocated to research questions that reflect a variety of populations, perspectives, and experiences; the roles of patient and family advisors are adjusted and expanded to accommodate their needs and priorities; and engagement practices are implemented not only at the point of care but also where individuals live, work, play, worship, and learn.
This change would also include practices that ensure the continuous monitoring of quality of care throughout a health system with respect to important demographic characteristics (e.g., race/ethnicity, gender identity) where differentials in care are often experienced. All clinical care team members should participate in culture and climate surveys, implicit bias assessment, and ongoing training tailored to a particular set of needs. In addition, the proactive engagement of and partnership with communities, including patients and their care partners often labeled “underserved,” “hard-to-reach,” and “medically and socially complex” in all health care delivery and design initiatives, will be central to success because the people with the most complex health and social needs are often the most intense users of health system resources. It will take every health system, organization, and provider explaining information in a way patients and families can understand—with all systems, organizations, and providers confirming and documenting that understanding—to achieve the goals the authors believe are critical for an equity-based health system that deeply engages patients, families, and communities.
The Role of External Factors in Driving PFEC and Addressing Health Inequities
Within the Guiding Framework, in the area of Organizational Foundations, a number of external contextual factors create the necessary underpinnings for developing a culture of PFEC. These factors include industry, technology, business, and policy initiatives, and they are paving the way for more widespread adoption of engagement approaches. This is an area of emerging practice, and while there is not yet clear data on the outcomes of these initiatives, the authors of this paper believe these approaches will lead to more equitable health outcomes as the field matures.
It is important to note that these same external levers that impact PFEC are also significant in moving health care systems toward structures, policies, and management that address health and health care disparities. To ensure that health systems can arrive at outcomes that align with the Quadruple Aim, the external contextual factors must be considered as the underpinnings for creating a system that simultaneously focuses on improving health equity and actively engaging patients, health system staff, families, and communities in co-creating learning health systems.
Examples of Policy Changes That Are Driving Equity
Certainly, health policy reforms exist with the aim of incentivizing needed culture change at the organizational level and with a focus on improving quality of care and driving health equity. Such efforts should also institute strategies to enhance engagement of health care organizations and systems with patients, families, and the broader community. Indeed, the repositioning of PFEC and health and health care equity as more central to the core mission and guiding principles of policies helps shift the culture toward that of inclusion of patient and families, which then helps ensure those from less included groups are actually at the table [72].
Ayanian and Williams published five principles for eliminating racial disparities as part of health care reform: (1) provide insurance coverage and access to high-quality care for all Americans; (2) promote a diverse health care workforce; (3) deliver patient-centered care; (4) maintain accurate, complete race and ethnicity data to monitor disparities in care; and (5) set measurable goals for improving quality of care and ensure that goals are achieved equitably for all racial and ethnic groups [11]. These principles are not just critical for eliminating racial/ethnic disparities, but are also important and necessary for addressing other inequities in health care such as those faced by vulnerable populations. While the Affordable Care Act (ACA) of 2010 did not aim to reduce health care inequities as a central focus, several elements could be viewed as helping support health equity through removing barriers to health care and addressing the aforementioned principles. The ACA has increased awareness and created and resourced a number of initiatives and incentives (reviewed in more depth below) that aim to shift the culture of the US health care system to one that is value-based; incentivizes population health management; encourages patient, family, and community engagement; and addresses health and health care equity [1,32,89]. These initiatives and incentives in the areas of quality and safety, community benefit and engagement, and patient and family engaged research represent a roadmap for how system-level innovative changes can be developed and implemented. They serve as exemplars for the potential impact that external factors such as health systems, clinics, and communities can have when they focus intentionally on PFEC and health care equity.
Quality and Safety
As a result of the ACA, the Centers for Medicare & Medicaid Services (CMS), the largest health care payer in the United States, made several programmatic changes to create incentives for improving health care quality and safety by emphasizing patient, family, and community engagement. The CMS initiative Partnership for Patients (PfP) and the Center for Medicare and Medicaid Innovation (CMMI) are two examples. Congress primarily established CMMI to test new payment and care delivery models that would stabilize or reduce expenditures while ensuring and improving health care quality. The PfP is a public-private partnership of health systems, clinicians, patients, and their families that works to improve the quality and safety of health care, as part of a larger Quality Innovation Network-Quality Improvement Organization program [28].
Community Benefit and Engagement
The ACA’s requirement that 501(c)(3)-status hospitals conduct a Community Health Needs Assessment (CHNA) at least every three years with the involvement of public health and community representatives is another driver of increased accountability for population health among hospitals and health systems [34]. Under the regulation, a hospital or health system’s CHNA findings must be made publicly available, which shows a broader push toward transparency and accountability for these providers [34].
As hospitals and health systems identify the needs of their communities during the CHNA process, they are ideally situated to collect useful information that can inform PFEC and health disparities strategies. CHNAs and the concomitant community health improvement plans (CHIPs) are some of the primary ways hospitals identify the broader community’s needs and then, critically, work to address them. More than 50 percent of the membership of America’s Essential Hospitals, an association for safety net hospitals, is on the path toward community-integrated health care through the implementation actions on their CHNAs [90].
Though CHNAs offer the potential to foster increased PFEC, that potential has yet to be fully realized. For instance, while community benefit requirements reflect the changing priorities of the health care sector, some experts see the lack of a minimum spending requirement as a limiting factor [94,96]. There is additional concern that funding population health improvement through hospital community benefit requirements could lead to increased disparities based on geography because state policies, community benefit allocations, and the distribution of tax-exempt hospitals vary considerably between communities [42]. Furthermore, the CHNA process is not always well-integrated throughout the institution, community, or population health improvements. Often, there are missed opportunities for community members, patients, caregivers, and families to weigh into the scope of the CHNA, the collection of the data, and the analysis and reporting of results; and improvement efforts are not often linked to parallel patient and family engagement, population health management, quality, or safety initiatives occurring within the same institution. While there are challenges to the implementation and use of CHNAs, they offer a promising strategy to involve communities in determining their health needs and strategies for addressing those needs. In addition, where health and health care disparities exist in communities, hospitals, and health systems, CHNAs offer an opportunity to engage those most at risk to contribute to identifying the best solutions to improve equity. An example of a needs assessment and implementation strategy with an emphasis on equity is in Box 3 below.
Patient and Family Engagement in Research
The creation of the Patient-Centered Outcomes Research Institute (PCORI) in 2010 through the ACA has influenced the culture of health research to include all health care stakeholders, including patients and families, to inform health care decision making. PCORI has elevated expectations for how patients and families contribute to every step of the research process, from concept and protocol development to data collection, analysis, and dissemination. PCORI’s authorizing legislation states that “The Institute shall identify national priorities for research, taking into account factors of disease incidence, prevalence, and burden in the United States (with emphasis on chronic conditions), gaps in evidence in terms of clinical outcomes, practice variations and health disparities in terms of delivery and outcomes of care” [83]. In line with the legislation, two of PCORI’s five National Priorities for Research are
Improving Healthcare Systems and Addressing Disparities. Throughout its work in the priority area of Addressing Disparities, PCORI focuses on populations “for which there is either strong evidence for health and health care disparities or insufficient health data. These groups are racial and ethnic minorities; rural populations; people with low incomes or low socioeconomic status; individuals with disabilities; lesbian, gay, bisexual, and transgender communities; and people with limited English proficiency” [85]. The goal of this priority area is to fund clinical comparative effectiveness research on interventions that can “guide decisions about how to eliminate disparities,” rather than simply labeling and further describing the existence of inequities [19].
The scale and influence of PCORI has, in large part, led to a proliferation of patient, family, and community-engaged research, as well as the application of community-based participatory research principles to health care research more broadly. See Box 4 and Box 5 for examples.
Beyond the ACA: Other National Efforts to Drive and Support Change
Recently, efforts beyond the ACA have been developed and implemented that could advance a health system culture that is responsive to directly addressing PFEC and health equity. This section discusses national efforts to drive and support change in PFEC and health equity occurring in the areas of data collection, data access, community integration, national awareness-building initiatives, accreditation standards, and education.
Data Collection
A fundamental step in identifying which populations are most at risk is to collect data on race, ethnicity, English-language proficiency, and other characteristics that are associated with disparities, including SOGI and disability status. A large body of research has documented disparities in access to and quality of health care when measures are stratified by these patient characteristics. While there is some guidance on standardized data collection for race, ethnicity, and language, including the 2009 Institute of Medicine (IOM) report Race, Ethnicity, and Language Data: Standardization for Health Care Quality Improvement, in which the subcommittee recommends collection of more granular ethnicity and language data according to national standards in addition to OMB race and Hispanic ethnicity categories [64], there are obstacles to achieving more widespread collection and use of these data. Although the risks of limited health literacy and numeracy are well documented, population-level adult literacy and numeracy data are collected only about once a decade and are not specific to health information and services, leaving a major gap in our knowledge about how these factors perpetuate population-level health disparities and health inequity [13,45,57,74]. Guidance on standardization of limited literacy and numeracy, digital skills, SOGI, and disability status for data collection are also needed.
The availability of data on characteristics frequently associated with disparities does not guarantee subsequent actions to reduce or eliminate disparities that are found. The absence of data, however, essentially guarantees that none of those actions will occur in a systematic and widespread way.
Data Access
Twenty years ago, an expert panel convened by the US Department of Health and Human Services identified a number of critical digital health engagement and equity issues in their final report Wired for Health and Well-Being [116]. Subsequent policy and consumer/patient studies and the Healthy People 2020 objectives on digital health information access have continued to document information and technology disparities [9]. Policy developments that have driven data access are the creation of National Coordinator for Health Information Technology in 2004 and the American Reinvestment and Recovery Act (ARRA) of 2009, which included many strategies to modernize the US infrastructure with an emphasis on health information technology [8]. One of the strategies passed under the ARRA was the Health Information Technology for Economic and Clinical Health (HITECH) Act of 2009, which had the goal that every person would use an Electronic Health Record (EHR) by 2014 [55].
It was through HITECH that the concept of meaningful use was born. Meaningful use is founded on five pillars of health outcomes policy priorities, and the first and second explicitly relate to the question of health equity: (1) improving quality, safety, and efficiency, and reducing health disparities; and (2) engaging patients and families in their health [26]. In other words, this policy makes explicit the need to increase engagement and empowerment of patients and families, which the authors of this paper argue will shift the culture of care to be more equitable.
Federal health IT policy coincided with and reflected broad social trends and market forces that resulted in people increasingly using digital technologies to connect, share, explore, and manage a wide range of everyday activities, including those related to their health [53]. EHR incentive programs via the meaningful use act required providers to show they were engaging patients to earn financial incentives. There was a “Blue Button” program established that made it easy to visualize what it meant to give patients data access. In March 2018, CMS announced the MyHealthEData initiative as “Blue Button 2.0” that aims to give patients more control over their health data and to make it more portable as patients move between different care settings [27].
The Evolution of Care Delivery Toward Increased Community Integration
Even under the ACA, health care coverage does not necessarily translate to access; this lack of access remains a challenge, especially in rural areas and in states that did not take advantage of the law’s incentives to expand Medicaid. Despite this challenge, new models of outreach and extension of health care provision into communities have been arising. Technologies such as video conferencing and telehealth have been at the forefront of this initiative to provide care in less accessible areas, though a number of other models have emerged, including community or employer-based clinics, among others.
Project ECHO (Extension to Community Healthcare Outcomes) is an example of such a novel approach. Launched in 2003 at the University of New Mexico Health Sciences Center to scale treatment efforts for hepatitis C, Project ECHO began when a clinical care team including a physician, psychiatrist, pharmacist, nurse, and social worker decided to host weekly teleECHO clinics via videoconference for primary care providers across New Mexico [87,12]. After the first ECHO clinic launched, the wait times to receive treatment for hepatitis C dropped significantly, and this approach to increasing access to care maintained quality of care across medically underserved patients and reduced health disparities [10]. Since this landmark study, many areas have adopted this approach in different ways especially in the areas of geriatrics, chronic pain, endocrinology, and behavioral and mental health disorders [12]. Examples of community-based strategies that have had a clear focus on equity are in Box 6 and Box 7.
Awareness-Building Initiatives
Prominent awareness-building initiatives and public pledges introduced by the most influential bodies in health care have collectively served as a national call to action to increase awareness of health care disparities and work to eliminate them. America’s Essential Hospitals, for example, has promoted a roadmap that explicitly integrates the establishment of a person-centered, inclusive culture that benefits all. This culture involves reviewing organizational priorities, fostering champions, and offering trainings that are integrated into person-centered care with supportive shared decision-making approaches, tools and workflows, and evidence-based research that involves engagement with patients and families [90]. While this roadmap still falls short of explicitly calling out health equity, it is an important step in embracing person-centered care, which is lacking in many clinical care pathways. As this membership group of safety net hospitals serve the populations most likely to experience disparities, they note in a recent report the critical importance of moving toward equity by explicitly addressing disparities as part of a focus on fostering a truly patient-centered culture [90,115]. See Figure 2, next pages.
Other examples include the CMS Equity Plan, the US Department of Veterans’ Office of Health Equity, the Institute for Healthcare Improvement’s Achieving Health Equity: A Guide for Health Care Organizations, and the American Hospital Association’s #123forEquity pledge campaign, which has garnered support by more than 1,700 hospitals nationwide [7,35,107,118]. The campaign calls on hospital and health system leaders to commit to increase the collection and use of race, ethnicity, language preference, and socioeconomic data; advance cultural competency training; increase diversity in leadership and governance; and strengthen community capacity [7,61].
Accreditation and Measurement Standards
Integrating activities around PFEC and health equity into accreditation and measurement standards has effectively gone from optional to imperative. Joint Commission accreditation standards now oblige hospitals and health systems to identify and address patients’ communication needs and collect patient-level demographic data to monitor and analyze disparities [37]. Similar concepts have been embedded in patient-centered medical home standards. However, there are conflicting perspectives on the extent to which the medical home model is reducing health disparities [43,80]. There are increased efforts to standardize the collection and coding of social determinants in EHRs; for example, the American Medical Association and a large private insurer are calling for the creation of ten new disease codes to reflect patient-level social needs, such as access to nutritious food or ability to pay for medications [92].
The National Quality Forum views the development of performance measures that can monitor disparities and the extent to which interventions are effective at reducing them as essential. They have also recognized the importance of actively including patients and families in their process [76]. Further, as the health system moves from fee-for-service to value and population health, there are opportunities to leverage performance measurement and standards to address improve health equity [75]. A critical component to developing measures is the integration of PFEC into the process. A promising start to this effort is implementation of the Hospital Consumer Assessment of Healthcare Providers and Systems by the CMS. This survey asks recently discharged patients to report on different aspects of their experience at the hospital, ranging from their perception of the cleanliness of the facility to questions around communication with the treatment team, and allows better comparison across hospitals [38]. Patients and families, along with other health and health care stakeholders, can contribute their experiences to the development of measurement and policy levers that can help advance equity.
Education and Training
Concepts of PFEC and health and health care equity are starting to make their way into medical education as well, positioning the next generation of clinicians to enter the workforce having been exposed to curriculum designed to promote understanding of how health care disparities, social determinants of health, and patient and family engagement factor into care. The Accreditation Council for Graduate Medical Education incorporated reducing health disparities into its Clinical Learning Environment Review program, which evaluates accreditation institutions that sponsor residency programs. Under the focus area of health care quality, the pathway “Resident/fellow and faculty member education on reducing health care disparities” prioritizes education on identifying and reducing health care disparities for the patient population seen at their institution as well as training in cultural competency [3].
Building on efforts like these to also include interprofessional education, curricula describing health disparities, cultural humility, implicit bias, and team training are important elements of education that will improve workforce capacity to better meet the needs of all populations and to better promote PFEC.
Action Steps to Operationalize PFEC and Health Equity: Organizational Culture and Policies
Health care organizations comprise some of the most vital and valuable community assets, and their values, leadership, and policies inform the extent to which PFEC and health equity characterize available health care services. While the previous section addressed the national efforts and initiatives that promote PFEC and health equity, this section discusses specific interventions and strategies that can be taken at the organizational foundation and strategic input areas of the Guiding Framework to operationalize PFEC and health equity culture within health care organizations.
Embedded in an organization’s foundation is its culture and the ethical frameworks and values that inform policies and practices. An organization’s foundation will reflect its level of awareness that patients and families are the reason the health care facility exists, as well as its awareness of a moral obligation to provide equitable care. Organizations with greater awareness of and commitment to patients and families as core partners will be better positioned for successful integration of PFEC that addresses individual and population-based health inequities. Health care administrators and leadership who want to advance PFEC and health equity can look to the four domains of the Charter on Professionalism for Healthcare Organizations [47]. The domains already include patient partnerships, organizational culture, community partnerships, and operations and business practices. By adding health equity to this Charter’s listed domains, a hospital, clinic, or health system that embraces its mission to serve as stewards of their communities can build their organizational culture in a patient-, family-, and equity-centered manner.
The Role of Hospitals in Advancing PFEC and Health Equity
Often hospitals and health systems hold key economic positions in their communities. This central role in communities is summarized well by the term “anchor institution.” Anchor institutions—or anchors—are organizations, including hospitals, that typically are the largest employer in the area and are closely tied to the larger “economic and social fabric of their communities” [39]. The mission of these types of institutions is a commitment to consciously apply the long-term, place-based economic power of the institution, in combination with its human and intellectual resources, to better the longterm welfare of the community in which the institution is anchored [39].
Another such role for health systems is that of the community “integrator,” which Nemours first introduced in 2012. Like anchors, integrators play a central role in their communities. However, the functions and responsibilities of the integrator go a step further. They fully assume accountability for the health of the community and act as a convener for population health improvements and collaborations [113]. Box 8 below depicts examples of integrators beyond hospitals and health systems, including quasi-governmental agencies, community-based nonprofits, and coalitions [30,31].
To fulfill an “anchor” or “integrator” role, health care systems will need to consider how PFEC and health equity are part of living their organizational values and meeting their ethical obligations [115]. Genuine commitment to health and well-being and leadership in a community entail acting on the core value that everyone in a community deserves access to high-quality health care that meets their needs.
The Role of Leadership to Drive Culture Change
As discussed in the Guiding Framework, health care leadership is a key element that can promote or inhibit changes toward a culture of PFEC. Leadership is also a key element needed to promote and advance health equity. Leaders occupy a central position in proposing and advancing organizational policies in favor of or opposed to (intentionally or unintentionally) PFEC and health equity. Leadership’s transparent and open commitment to improve the organization’s culture and root out bias and systemic (institutional and structural) racism to meet the needs of all populations served is essential to eliminate health care inequities. This change can occur through clear public statements about such commitment followed by regular and bidirectional information exchange with patients, families, and communities; invitations for engagement and input that are used to co-create positive changes; and supportive policies and training that intentionally aim to address health equity. Once these items are in place, transformative actions can emerge.
Another strategy that leadership can use to drive culture change toward PFEC and help reduce disparities is to create the space for diverse patient and family members to serve as co-leaders within the health system, along with the paid and titled professionals. Having a range of experiences and opinions from patients and families who play a significant role in the development, implementation, and/or evaluation of activities and policies can help to ensure health equity. This leadership role for patients and families must extend beyond sharing their stories. Although patient stories can provide powerful emotional witness to successes and failures in care processes, they are not sufficient measures of meaningfully engaging patients and families. When authentic engagement is not occurring, these stories can paradoxically feed the existing power imbalance between those who provide care and those
who receive it. Leaders can listen to and empathize with moving stories that give patients and families the illusion of being heard without leadership commitment to necessary culture and policy changes. This situation leaves in place or potentially allows for additional deterioration in the conditions that generated poor patient and family experiences and that perpetuate bias and permit systemic racism to persist.
When meaningful engagement occurs, patients and families actively participate and are empowered to contribute to the culture and needs of the hospital and health system. In this leadership role, patients and families can drive change by asking the sometimes uncomfortable questions, such as asking hospitals to explain their stewardship of funds and philanthropy allocation, or how the research they are conducting will benefit communities, especially those that bear the greatest burden of health inequities. Patients and families can ask how policies and rules are established and whether they have been analyzed for their health equity implications, and what strategies are in place to reduce and eliminate implicit bias. Recent reports indicate a promising trend toward more meaningful engagement [114]. Most importantly, patients and their families can contribute to the co-creation of more equitable policies, processes, and outcomes.
It is critical to note the importance of champions just beneath C-suite leaders. These champions provide backup and support to the leadership [110]. Some, like Dr. Ronald Copeland, Chief Diversity Officer at Kaiser Permanente, stated that in his organization, “diversity and inclusion are valued not just to be compliant with regulations but as business strategies to enhance [our] accomplishments and achieve [our] goals” [110]. Others, like Dr. Joan Reede, Dean for Diversity and Community Partnership at Harvard Medical School, look to the education of future health care professionals and take an explicit lens to recruiting, retaining, and advancing underrepresented groups, saying “when you have complex issues, linear and siloed thinking will not give you as good a result as having multiple voices, perspectives, and backgrounds at the table” [16]. Thus, leaders who shine in diversity and promote PFEC and health equity are those who listen to their champions, provide high levels of support and encouragement, and are equally receptive to feedback and guidance.
These leaders also understand that empathy is a key trait to promote throughout a health care team, organization, and system. Empathy is emerging as a key health care professional training strategy that can lead to culture shift, reduce bias, improve patient care, and enhance patient satisfaction [101,102,109]. Empathy is important to patients and employees. When employees feel their supervisors and coworkers care about them as humans, it can lead to reduced stress, improved engagement, and better performance [103]. This focus on empathy aligns with many health care systems’ trends toward promotion of “compassionate care” and improvement of the overall “patient experience.” An example of a health system implementing this concept is in Box 9.
Quality Improvement Initiatives
Quality improvement initiatives can drive health equity, but only when policies and their implementation are intentionally framed as addressing both quality and equity. Quality and equity are two sides of the same coin—they are inextricably linked and have to proceed together. First, hospitals should stratify clinical quality and patient experience data by race, ethnicity, language, SOGI, disability status, transportation access, and socioeconomic status to reveal disparities. Hospitals should next work with staff and patient, family, and community members to better understand the potential reasons for the disparities and discuss opportunities to address them. Hospitals then should create an action plan based on those findings and look to implement effective quality improvement solutions and interventions tailored to and proven to improve equity for populations who receive disparate quality care. For example, PCORI has funded, and will make publicly available, the results of more than 94 clinical comparative effectiveness research studies, representing over $309 million, focused on improving or eliminating health and health care disparities [85]. These patient-centered and patient- and stakeholder engaged studies could help identify interventions that work best to improve the health of populations at risk for disparities, identify tailored approaches to meeting patient needs, and address heterogeneity of treatment effects to understand “which treatment works best, for whom, and under what conditions” [84]. An example is presented in Box 10.
Patient and Family Advisory Councils
PFACs are a matter of both organizational culture and policy changes. PFACs have proliferated among health care organizations and set a preliminary tone of engagement with important stakeholders in health care. Many PFACs are at early stages of development and need better integration with senior leaders and governance bodies [59,105].
A critical issue for the next generation of PFACs and patient and family engagement activities is the inclusion of advisors who are more representative of populations served by the hospital and health systems, with special attention to recruitment and integration of diverse participants into PFACs and other patient, family, and community engagement efforts. It is essential to ensure that hospital and health system leadership interacts directly with those most immediately affected by health inequities.
Furthermore, PFACs should include better integration of patients and family members in governance bodies, including the boards of trustees, as well as in population and community health activities. Community health workers (CHWs) and patient navigators, a growing workforce that is often drawn from underserved or diverse communities, can “bridge” the health system and communities [56,112]. They should be included more intentionally in patient, family, and community engagement efforts at the organizational level.
There are challenges to ensuring that PFACs are diverse. In many cases, patients and family members are asked to volunteer their time to PFACs, which may be financially difficult for some. In addition, child care and transportation may further complicate patient and family desires to contribute to PFACs. There is room to address these and other barriers to improve the PFAC models; for example, the development of virtual opportunities may be one possible solution for inviting effective inclusion. Moving PFACs and engagement efforts in this direction will better position patients, families, and communities to help drive the alignment of quality and safety, population health management, and community health initiatives.
Creating a Health Literate Organization
Health literacy encompasses skills that go beyond reading and writing, but also include the ability to listen, speak, and have cultural knowledge and numeracy around health information. Implementing initiatives around health literacy allows organizations to learn how to address and align health information and services with people’s knowledge, skills, and needs to provide better care [95]. Attention to health literacy should improve people’s general capacities to act in health-promoting/protecting ways and navigate health systems, including how/when to get care, how to seek information, how to communicate their needs, how to set health goals, and how to think critically about health at personal, family, and community levels [95].
To ensure that patients can speak about and understand discussions around health, organizations may have policies on language access to provide both interpretation and translation services; however, these policies may not be well-supported, well-supervised, or understood by health care team members. Interpreter services for patients and family members provide support for PFEC and health equity by facilitating communication between providers and patients. Efforts to improve access should align with the federal plan to move the legal standard for interpreters in health care organizations from “competent” to “qualified” to reduce the risk of medical errors [4]. Measures for improving language access could include (1) identification of participants’ need for language services; (2) leadership training and orientation programs for administrative and clinical leaders; (3) patient engagement in language access services, smartphone support, online patient education materials, and translated documents; (4) stratification of performance data by language to determine disparities; and (5) use of the most appropriate individuals for interpretation [44].
Health literacy researchers and practitioners have proposed the concept of “health literate health care organizations” as a means to change polices, practices, and culture to ensure that patient and family needs are at the heart of care processes and that organizations can address disparities associated with low health literacy and numeracy and LEP [15]. Although health literacy improvement was not mandated by the ACA, it has been recognized as a fundamental element of successful PFEC.
Health literacy has patient and family engagement implications at both the individual and organizational level. Inviting patients and families to serve on hospital boards or advisory groups introduces both challenges and opportunities from a health literacy perspective. People with limited numeracy and literacy skills may be comfortable communicating orally but be challenged to understand and use written documents, forms, and patient portals. For example, if a patient or family member on a hospital advisory board receives a lengthy, dense written document to prepare for a meeting, they may not be able to prepare and fully participate in the discussion and provide recommendations. Health care organizations should recognize literacy and numeracy challenges in their communities and provide information in multiple formats, such as digital recordings, health education visualization tools,
or other mechanisms to make information more accessible and useful by all. Although organizations may perceive these additional formats as a burden, they will gain in the long run by including the perspectives of patients, families, and community members who would otherwise not pay attention to or use hospital- and clinic-supplied information. While upstream efforts to increase the health literacy of communities are needed, Box 11 shows an example of an organization changing its practices to better suit the existing needs of the community it serves.
Diversifying the Workforce and Integrating Culturally Responsive Training Approaches
The many cultures of the health care workforce can help support better PFEC integration through improving trust, understanding, and cultural humility, as well as opening up the lines of communications among patients, families, and their clinical care teams. Research suggests that patients may prefer to seek care in environments and from care team members that look like and understand them [6].
Many organizations use cultural competency and implicit bias training as a way to bridge cultural and language differences between providers and patients. The authors of this paper believe that it is important to shift the paradigm toward training that recognizes implicit biases and cultural responsiveness that involves cultural humility, with the understanding that no one can be completely “culturally competent” [111]. This type of training recognizes individual and collective power and privilege from multiple viewpoints and then creates dialogue around our place and space and the interactions that occur within the health system, patients, family, and the community. Some states, such as California, are moving to require implicit bias training in an effort to reduce particularly troubling maternal mortality disparities [23]. Health care leaders also have to be proactive and intentional about training and bringing on board diverse PFAC members, and ensuring that trainings and meetings take place not only in the walls of the medical centers but also outside in community spaces.
Beyond the diversity of the workforce and patient and family advisors, the authors of this paper believe it is critical to also look at the influence specific positions or functions have on increasing engagement and reducing disparities. One important exemplar is patient navigators. Patient navigators have become more prevalent across health care organizations—especially around cancer care delivery support. Patient navigation is an empirically supported care management strategy initially deployed to address disparities in cancer [50]. This type of support has demonstrated efficacy in overcoming barriers to health care access and utilization, bandaging system fragmentation, and addressing social determinants of health [51,88]. Established navigation practices include individual-level information exchange, resource referral, appointment scheduling, and tailored assistance to overcome barriers to health care [112].
The bottom line, however, is that all of our health care workforce members—regardless of role—need to be comfortable engaging with all of the populations with whom they work. The models that have proliferated across the United States, such as patient navigators and CHWs, have not been well integrated into the actual health care delivery system [112]. Currently, they are mostly funded by soft funds (e.g., grants, philanthropy) because at present, navigators do not have an officially designated health care system position, and it is challenging to get reimbursement for their work [93]. This new workforce provides a critical bridge to the communities, and the health system should see roles such as patient navigators and CHWs as sources of empathetic insights around optimal ways of caring for patients who face great disparities in care.
Conclusion
It is imperative that health equity be explicitly integrated into the core of a culture that truly engages patients and their families in care. This paper detailed some of the essential levers of change that health systems, health care institutions, and policy makers should consider in trying to implement a culture that values PFEC and health equity, and that takes care of and improves the health of all populations. Achieving this goal will necessitate both a cultural shift and innovative and unconventional strategies to deliver health for all, such as adopting strategies to support patients with low levels of health literacy, supporting better integration of diverse PFACs, improving the cultural humility of the health care workforce, increasing access to care, and expanding telehealth strategies. These strategies support all persons in accessing appropriate care and ensuring they have the ability to participate as partners in that care.
One underlying truth to implementing such an inclusive approach is that there needs to be alignment of levers including that of the mission, values, and leadership of a particular system or organization. Without such alignment, there is no sustainability. As systems of PFEC are being built, health equity must be included as a basic necessity of the system, not an afterthought. National policies such as CMS’s Equity Plan and Joint Commission accreditation standards that include health disparities are important steps in the right direction but need to be supplemented by committed organizational and individual efforts.
Achieving health equity requires flipping the traditional institutional approach to delivering health care that positions providers as the sole experts and deprioritizes the experiences of a diverse population. We must leverage all talents, including those of patients, families, and communities who have a wealth of knowledge to share and should be included as equal partners, to help achieve population health with health equity at its core. To achieve such a transformation, inclusion of people from a diverse background, with full transparency, is essential. Leaders of hospitals and health care systems must remain vigilant and examine the policies and structures, which could have intentional and unintentional consequences and could be perpetuating systemic (structural and institutional) racism. An organization and its leaders need to be ready for such change and to actively integrate diverse voices who have not traditionally been involved in the decision-making process. A cultural and transformational change to PFEC and health equity is difficult to achieve without making an explicit commitment to such inclusion, and it is hard to drive and sustain change in established and complex systems. Change efforts must be grounded in core values that continually and comprehensively emphasize equity, are lived out across organizations with leadership investment and vocal support, and are infused throughout every aspect of day-to-day operations. The time for changing organizations from the inside moving forward with patients and their caregivers as full partners, for creating the inclusive environments that break down the usual siloed and biased care, and for driving a shift toward health equity that lifts health for all is now.
Join the conversation!
![]() Tweet this! Patient & family engaged care and health equity are critical to improving population health, but achieving both will require planning. Read more about how to move toward health equity by involving patients and families in a new #NAMPerspectives: https://doi.org/10.31478/202007a
Tweet this! Patient & family engaged care and health equity are critical to improving population health, but achieving both will require planning. Read more about how to move toward health equity by involving patients and families in a new #NAMPerspectives: https://doi.org/10.31478/202007a
![]() Tweet this! How can we work to improve a health care system that has historically contributed to health inequities so that it can better serve patients who arrive at the health care system w/ conditions created by these inequities? Read more: https://doi.org/10.31478/202007a #NAMPerspectives
Tweet this! How can we work to improve a health care system that has historically contributed to health inequities so that it can better serve patients who arrive at the health care system w/ conditions created by these inequities? Read more: https://doi.org/10.31478/202007a #NAMPerspectives
![]() Tweet this! Read a new #NAMPerspectives discussion paper for examples of organizations across the country who are working to ensure health equity and patient and family engaged care are critical parts of accessing health care: https://doi.org/10.31478/202007a
Tweet this! Read a new #NAMPerspectives discussion paper for examples of organizations across the country who are working to ensure health equity and patient and family engaged care are critical parts of accessing health care: https://doi.org/10.31478/202007a
Download the graphics below and share them on social media!


References
- Abrams, M., R. Nuzum, S. Mika, and G. Lawlor. 2011. Realizing health reform’s potential: How the affordable care act will strengthen primary care and benefit patients, providers, and payers. Issue brief (Commonwealth Fund) 1:1-28. Available at: https://www.commonwealthfund.org/publications/issuebriefs/2011/jan/realizing-health-reforms-potential-how-affordable-care-act-will (accessed May 31, 2020).
- Abrams, M. A., S. Kurtz-Rossi, A. Riffenburgh, and B. Savage. 2014. Building health literate organizations: A guidebook to achieving organizational change. Available at: https://www.unitypoint.org/filesimages/Literacy/Health%20Literacy%20Guidebook.pdf (accessed May 31, 2020).
- Accreditation Council for Graduate Medical Education. 2014. Clinical learning environment review (cler): Expectations for an optimal clinical learning environment to achieve safe and high-quality patient care. Available at: http://www.acgme.org/Portals/0/PDFs/CLER/CLER_Brochure.pdf (accessed May 10, 2017.)
- Agency for Healthcare Research and Quality, and U.S. Department of Health and Human Services. 2016. 2016 National Healthcare Quality and Disparities Report. Rockville, MD: Agency for Healthcare Research and Quality. Available at: https://www.ahrq.gov/research/findings/nhqrdr/nhqdr16/index.html (accessed May 31, 2020).
- Agency for Healthcare Research and Quality, and U.S. Department of Health and Human Services. 2018. 2018 National Healthcare Quality and Disparities Report. Rockville, MD: Agency for Healthcare Research and Quality. Available at: https://www.ahrq.gov/research/findings/nhqrdr/nhqdr18/index.html (accessed May 31, 2020).
- Alsan, M., O. Garrick, and G. C. Graziani. 2018. Does Diversity Matter for Health? Experimental Evidence from Oakland. National Bureau of Economic Research. Available at: https://differencesmatter.ucsf.edu/sites/g/files/tkssra1966/f/wysiwyg/oakland_0%20%281%29.pdf (accessed May 31, 2020).
- American Hospital Association. 2018. American Hospital Association #123forequity Campaign to Eliminate Health Care Disparities. Available at: http://www.equityofcare.org/ (accessed May 31, 2020).
- American Recovery and Reinvestment Act of 2009. 2009. 111th Congress of the United States of America. Available at: https://www.govinfo.gov/content/pkg/BILLS-111hr1enr/pdf/BILLS-111hr1enr.pdf (accessed May 31, 2020).
- University of Vermont Medical Center. 2019. Applying for a grant: Community health investment fund. Available at: https://www.uvmhealth.org/medcenter/pages/about-uvm-medical-center/the-community/grants.aspx (accessed June 18, 2019).
- Arora, S., K. Thornton, G. Murata, P. Deming, S. Kalishman, D. Dion, B. Parish, T. Burke, W. Pak, J. Dunkelberg, M. Kistin, J. Brown, S. Jenkusky, M. Komaromy, and C. Qualls. 2011. Outcomes of Treatment for Hepatitis C Virus Infection by Primary Care Providers. New England Journal of Medicine 364(23):2199-2207. https://doi.org/10.1056/NEJMoa1009370.
- Ayanian, J. Z., and R. A. Williams. 2011. Principles for eliminating racial and ethnic disparities in health care under healthcare reform. In Healthcare Disparities at the Crossroads with Healthcare Reform, edited by R. A. Williams: Springer.
- Barash, D. 2015. Project ECHO: Force Multiplier for Community Health Centers. Health Affairs Blog. Available at: https://www.healthaffairs.org/do/10.1377/hblog20150720.049437/full/ (accessed May 31, 2020).
- Berkman, N. D., S. L. Sheridan, K. E. Donahue, D. J. Halpern, A. Viera, K. Crotty, A. Holland, M. Brasure, K. N. Lohr, E. Harden, E. Tant, I. Wallace, and M. Viswanathan. 2011. Health literacy interventions and outcomes: An updated systematic review. Rockville, MD: Agency for Healthcare Research and Quality (AHRQ). Available at: https://www.ahrq.gov/downloads/pub/evidence/pdf/literacy/literacyup.pdf (accessed May 31, 2020).
- Bourgois, P., S. M. Holmes, K. Sue, and J. Quesada. 2017. Structural vulnerability: Operationalizing the concept to address health disparities in clinical care. Academic Medicine 92(3):299-307. https://doi.org/10.1097/ACM.0000000000001294
- Brach, C., D. Keller, L. M. Hernandez, C. Baur, R. Parker, B. Dreyer, P. Schyve, A. J. Lemerise, D. Schillinger. 2012. Ten Attributes of Health Literate Health Care Organizations. NAM Perspectives. Discussion Paper, National Academy of Medicine, Washington, DC. https://doi.org/10.31478/201206a
- Bradley Ruder, D. 2018. Champion of equity and social justice. The Harvard Gazette. Available at: https://news.harvard.edu/gazette/story/2018/10/joan-reede-builds-diversity-and-inclusion-intoharvard-medical-schools-ethos/ (accessed May 31, 2020).
- Brady, K. 2016. The Status of Public Health: Spartanburg County, South Carolina 2016 Update. Spartanburg Community Indicators Project. Available at: https://www.strategicspartanburg.org/files/The%20Status%20of%20Public%20Health,%20Spartanburg%20County%202016%20Update.pdf (accessed May 31, 2020).
- Brady, K. 2018. Spartanburg Racial Equity Index: A Review of Predictors and Outcomes. Metropolitan Studies Institute at USC Upstate. Available at: https://www.strategicspartanburg.org/data/Spartanburg-Racial-Equity-Index.pdf (accessed May 31, 2020).
- Braveman, P., E. Arkin, T. Orleans, D. Proctor, and A. Plough. 2017. What is health equity? And what difference does a definition make? Princeton, NJ: Robert Wood Johnson Foundation. Available at: https://www.rwjf.org/en/library/research/2017/05/whatis-health-equity-.html (accessed May 31, 2020).
- Braveman, P., and L. Gottlieb. 2014. The Social Determinants of Health: It’s Time to Consider the Causes of the Causes. Public Health Reports 129 Suppl 2:19-31. https://doi.org/ 10.1177/00333549141291S206
- Burton Blatt Institute. 2011. What is an inclusive culture? Available at: https://fdocuments.in/document/what-is-an-inclusive-culture-burton-blattinstitute-at-is-an-inclusive-culture.html (accessed May 31, 2020).
- Cairns, A. L., F. Schlottmann, P. D. Strassle, M. Di Corpo, and M. G. Patti. 2019. Racial and socioeconomic disparities in the surgical management and outcomes of patients with colorectal carcinoma. World Journal of Surgery 43(5):1342-1350. https://doi.org/ 10.1007/s00268-018-04898-5
- California Senate. 2018. California dignity in pregnancy and childbirth act. SB 464. Available at: https://leginfo.legislature.ca.gov/faces/billTextClient.xhtml?bill_id=201920200SB464 (accessed May 31, 2020).
- Center for Economic and Community Development. 2020. Community engagement. Available at: https://aese.psu.edu/research/centers/cecd/engagement-toolbox/engagement (accessed July 9, 2019.)
- Centers for Disease Control and Prevention. 2013. CDC Health Disparities and Inequalities Report – United States, 2013. Morbidity and Mortality Weekly Report 62(Suppl 3). Available at: https://www.cdc.gov/mmwr/pdf/other/su6203.pdf (accessed May 31, 2020).
- Centers for Disease Control and Prevention. 2017. Public Health and Promoting Interoperability Programs. Available at: https://www.cdc.gov/ehrmeaningfuluse/introduction.html (accessed May 31, 2020).
- Centers for Medicare and Medicaid Services Newsroom. 2018. Trump Administration Announces MyHealthEData Initiative to Put Patients at the Center of the US Healthcare System system. Available at: https://www.cms.gov/newsroom/press-releases/trump-administration-announces-myhealthedatainitiative-put-patients-center-us-healthcare-system (accessed May 31, 2020).
- Centers for Medicare and Medicaid Services. 2019. Current work. Available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/QualityImprovementOrgs/Current (accessed May 31, 2020).
- Centers for Medicare and Medicaid Services. 2018. Rural-Urban Disparities in Health Care in Medicare. Available at: https://www.cms.gov/About-CMS/Agency-Information/OMH/Downloads/Rural-Urban-Disparities-in-Health-Care-in-Medicare-Report. pdf (accessed May 31, 2020).
- Nemours. 2012. Integrator Role and Functions in Population Health Improvement Initiatives. Available at: http://www.movinghealthcareupstream.org/wp-content/uploads/2018/06/Integrator.role_.in_.pop_.health.improvement.initiatives-2.pdf (accessed May 31, 2020).
- Chang, D. I. 2012. What does a population health integrator do? Improving Population Health. Available at: https://www.improvingpopulationhealth.org/blog/2012/05/what-does-a-population-healthintegrator-do.html (accessed May 31, 2020).
- Chen, J., A. Vargas-Bustamante, K. Mortensen, and A. N. Ortega. 2016. Racial and Ethnic Disparities in Health Care Access and Utilization Under the Affordable Care Act. Medical Care 54(2):140. https://doi.org/10.1097/MLR.0000000000000467.
- Boston CHNA-CHIP Collaborative. 2018. The CHNA Process. Available at: http://bostonchna.org/chna.html (accessed May 31, 2020).
- Cleland, C. L., R. F. Hunter, M. A. Tully, D. Scott, F. Kee, M. Donnelly, L. Prior, and M. E. Cupples. 2014. Identifying Solutions to Increase Participation in Physical Activity Interventions Within a Socio-Economically Disadvantaged Community: A Qualitative Study. International Journal of Behavioral Nutrition and Physical Activity 11(1). https://doi.org/10.1186/1479-5868-11-68.
- CMS Office of Minority Health. 2015. The CMS Equity Plan for Improving Quality in Medicare. Centers for Medicare & Medicaid Services, Department of Health and Human Services. Available at: https://www.cms.gov/About-CMS/Agency-Information/OMH/OMH_Dwnld-CMS_EquityPlanforMedicare_090615.pdf (accessed May 31, 2020).
- Coleman, C. L., M. R. Abraham, and B. H. Johnson. 2019. Strengthening Diversity in Research Partnerships: Knowledge to Action Guide. Bethesda, MD: Institute for Patient- and Family-Centered Care. Available at: https://www.ipfcc.org/bestpractices/strengthening-diversity/IPFCC_Strengthening_Diversity_In_Research_Partnerships_Final.pdf (accessed May 31, 2020).
- Institute for Healthcare Improvement. 2010. Advancing effective communication, cultural competence, and patient- and family-centered care: A roadmap for hospitals. Oakbrook Terrace, IL: The Joint Commission. Available at: http://www.ihi.org/resources/Pages/Publications/AdvancingEffective-CommunicationCulturalCompetencePFCC.aspx (accessed May 31, 2020).
- Cooper, J., and W. Zimmerman. 2017. The effect of a faith community nurse network and public health collaboration on hypertension prevention and control. Public Health Nursing 34(5):444-453. https://doi.org/10.1111/phn.12325
- County Health Rankings & Roadmaps, and University of Wisconsin Population Health Institute. 2016. What works? Strategies to improve rural health. Available at: https://www.countyhealthrankings.org/reports/what-works-strategies-improve-rural-health (accessed May 31, 2020).
- King County. 2016. County leaders, UW President propose historic agreement to ensure Harborview remains one of the nation’s premier medical centers, expands reach to community-based care. Available at: https://www.kingcounty.gov/elected/executive/constantine/news/release/2016/February/01-harborview-agreement.aspx (accessed May 31, 2020).
- United Nations Educational, Scientific and Cultural Organization. 2020. Cultural Inclusion. Available at: http://www.unesco.org/new/en/social-andhuman-sciences/themes/urban-development/migrants-inclusion-in-cities/good-practices/culturalinclusion/(available at May 31, 2020).
- Curtis, J., and H. Lang. 2018. Hospital Community Benefit Dashboard: Advancing Health Equity and Community Engagement. Community Catalyst. Available at: https://www.communitycatalyst.org/resources/publications/document/CC-HospitalCommenefitDashboard-Report-F2.pdf (accessed May 31, 2020).
- De Marchis, E. H., K. Doekhie, R. Willard-Grace, and J. N. Olayiwola. 2018. The impact of the patient-centered medical home on health care disparities: Exploring stakeholder perspectives on current standards and future directions. Population Health Management 22(2):99-107. https://doi.org/10.1089/pop.2018.0055.
- Department of Health and Human Services. 2013. National Culturally and Linguistically Appropriate Services Standards. Available at: https://www.thinkculturalhealth.hhs.gov/clas/standards (accessed June 1, 2020).
- Desmond, M., and M. Emirbayer. 2016. Race in America. New York : W.W. Norton & Company, Inc.
- Dzau, V. J., M. B. McClellan, J. McGinnis, S. P. Burke, M. J. Coye, A. Diaz, T. A. Daschle, W. H. Frist, M. Gaines, M. A. Hamburg, J. E. Henney, S. Kumanyika, M. O. Leavitt, R. M. Parker, L. G. Sandy, L. D. Schawff er, G. D. Steele, Jr. P. Thompson, and E. Zerhouni. 2017. Vital Directions for Health and Health Care: Priorities From a National Academy of Medicine Initiative. JAMA 317(14):1461-1470. https://doi.org/ 10.1001/jama.2017.1964
- Egener, B. E., D. J. Mason, W. J. McDonald, S. Okun, M. E. Gaines, D. A. Fleming, B. M. Rosof, D. Gullen, and M.-L. Andresen. 2017. The Charter on Professionalism for Health Care Organizations. Academic Medicine 92(8):1091-1099. https://doi.org/10.1097/ACM.0000000000001561
- Massachusetts General Hospital. 2018. Four Boston Coalitions Awarded MGH Grants. Available at: https://www.massgeneral.org/community-health/cchi/news/four-boston-coalitions-awarded-mghgrants (accessed September 18, 2019).
- Frampton, S. B., S. Guastello, L. Hoy, M. Naylor, S. Sheridan, and M. Johnston-Fleece. 2017. Harnessing Evidence and Experience to Change Culture: A Guiding Framework for Patient and Family Engaged Care. NAM Perspectives. Discussion Paper, National Academy of Medicine, Washington, DC. https://doi.org/10.31478/201701f
- Freeman, H. P. 2015. Patient Navigation as a Targeted Intervention: For Patients at High Risk for Delays in Cancer Care. Cancer 121(22):3930. https://doi.org/10.1002/cncr.29610.
- Freund, K. M., T. A. Battaglia, E. Calhoun, J. S. Darnell, D. J. Dudley, K. Fiscella, M. L. Hare, N. LaVerda, J.-H. Lee, P. Levine, D. M. Murray, S. R. Patierno, P. C. Raich, R. G. Roetzheim, M. Simon, F. R. Snyder, V. Warren-Mears, E. M. Whitley, P. Winters, G. S. Young, and E. D. Paskett. 2014. Impact of patient navigation on timely cancer care: The patient navigation research program. Journal of the National Cancer Institute 106(6):dju115. https://doi.org/10.1093/jnci/dju115.
- Friedman, D., D. Perry, and C. Menendez. 2016. The Foundational Role of Universities as Anchor Institutions in Urban Development: A Report of National Data and Survey Findings. Coalition of Urban Serving Universities. The Association of Public and Land-Grant Universities. Available at: https://usucoalition.org/images/APLU_USU_Foundational_FNLlo.pdf (accessed June 1, 2020).
- Halamka, J. D., and M. Tripathi. 2017. The HITECH Era in Retrospect. New England Journal of Medicine 377(10):907-909. https://doi.org/10.1056/NEJMp1709851.
- Harborview Medical Center. 2019. Hospital Overview. Available at: https://www.uwmedicine.org/locations/harborview-medical-center#main-tab-tab—clinic-overview-jump (accessed June 18, 2019.)
- Health Information Technology for Economic and Clinical Health (HITECH) Act. 2009. 111th Congress of the United States of America. Available at: https://www.hhs.gov/sites/default/files/ocr/privacy/hipaa/understanding/coveredentities/hitechact.pdf (accessed June 1, 2020).
- Health Resources and Services Administration. 2007. Community Health Worker National Workforce Study. U.S. Department of Health and Human Services. Available at: https://bhw.hrsa.gov/sites/default/files/bhw/nchwa/projections/communityhealthworkforce.pdf (accessed June 1, 2020).
- Health Resources in Action. 2019. Boston CHNA and CHIP Collaborative. https://hria.org/projects/boston-chna-chip-collaborative/ (accessed June 1, 2020).
- University of Washington Medicine. 2017. Healthcare equity blueprint. Available at: https://depts.washington.edu/uwmedptn/wp-content/uploads/UW-Medicine-Healthcare-Equity-Blueprint-2017.05.01.pdf (accessed June 18, 2019).
- Heath, S. 2017. How to Integrate the Patient Voice into Healthcare Decision-Making. Available at: https://patientengagementhit.com/news/how-to-integratethe-patient-voice-into-healthcare-decision-making (accessed June 18, 2019.)
- Henry Ford Health Care System. 2011. Healthcare Equity Campaign 2009-2011 Final Report. Available at: https://www.henryford.com/-/media/fi les/henry-ford/about/healthcare-equity-campaign-report.pdf?la=en (accessed June 1, 2020).
- Herrin, J., K. G. Harris, E. Spatz, D. Cobbs-Lomax, S. Allen, and T. Leon. 2018. Hospital Leadership Diversity and Strategies to Advance Health Equity. Joint Commission Journal on Quality and Patient Safety 44(9):545-551. https://doi.org/10.1016/j.jcjq.2018.03.008.
- Institute of Medicine. 2001. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: The National Academies Press. https://doi.org/10.17226/10027.
- Institute of Medicine. 2003. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: The National Academies Press. https://doi.org/10.17226/12875.
- Institute of Medicine. 2009. Race, Ethnicity, and Language Data: Standardization for Health Care Quality Improvement. Washington, DC: The National Academies Press. https://doi.org/10.17226/12696.
- Kindig, D., and G. Stoddart. 2003. What is Population Health? American Journal of Public Health 93(3):380-383. https://doi.org/10.2105/AJPH.93.3.380
- Kirwan Institute for the Study of Race and Ethnicity. 2015. Understanding implicit bias. Available at: http://kirwaninstitute.osu.edu/research/understanding-implicit-bias/ (accessed June 1, 2020).
- LaVeist, T. A., D. Gaskin, and P. Richard. 2011. Estimating the Economic Burden of Racial Health Inequalities in the United States. International Journal of Health Services 41(2):231-238. https://doi.org/10.2190/HS.41.2.c.
- Martin, T., W. Barfi eld, H. Brown, A. Langer, S. Mann, and K. Scott. 2019. Deaths from Pregnancy and Childbirth: Why are More U.S. Mothers Dying and What Can Be Done? Available at: https://theforum.sph.harvard.edu/events/deaths-from-pregnancyand-childbirth/ (accessed June 1, 2020).
- Bullard, K. M., C. C. Cowie, S. E. Lessem, S. H. Saydah, A. Menke, L. S. Geiss, T. J. Orchard, D. B. Rolka, and G. Imperatore. 2018. Prevalence of Diagnosed Diabetes in Adults by Diabetes Type – United States, 2016. Morbidity and Mortality Weekly Report 67(12):359-361. http://dx.doi.org/10.15585/mmwr.mm6712a2
- Meghani, S. H., E. Byun, and R. M. Gallagher. 2012. Time to Take Stock: A Meta-Analysis and Systematic Review of Analgesic Treatment Disparities for Pain in the United States. Pain Medicine 13(2):150-174. https://doi.org/10.1111/j.1526-4637.2011.01310.x.
- Microaggression. 2017. In Oxford English Dictionary: Oxford University Press.
- Myers, R. E., M. DiCarlo, M. Romney, L. Fleisher, R. Sifri, J. Soleiman, E. Lambert, and M. Rosenthal. 2018. Using a Health System Learning Community Strategy to Address Cancer Disparities. Learning Health Systems 2(4):e10067. https://doi.org/10.1002/lrh2.10067
- National Academies of Sciences, Engineering, and Medicine. 2017. Communities in Action: Pathways to Health Equity. Washington, DC: The National Academies Press. https://doi.org/10.17226/24624.
- National Academies of Sciences, Engineering, and Medicine. 2016. Integrating Health Literacy, Cultural Competence, and Language Access Services: Workshop Summary. Washington, DC: The National Academies Press. https://doi.org/10.17226/23498.
- National Quality Forum. 2017. An Environmental Scan of Health Equity Measures and a Conceptual Framework for Measure Development. Washington, DC. Available at: https://www.qualityforum.org/Publications/2017/06/An_Environmental_Scan_ of_Health_Equity_Measures_and_a_Conceptual_Framework_for_Measure_Development.aspx (accessed June 1, 2020).
- National Quality Forum. 2017. Measuring What Matters to Patients: Innovations in Integrating the Patient Experience into Development of Meaningful Performance Measures. Available at: http://www.qualityforum.org/Publications/2017/08/Measuring_What_Matters_to_Patients__Innovations_in_Integrating_the_Patient_Experience_into_Development_of_Meaningful_Performance_Measures.aspx (accessed June 1, 2020).
- Spartanburg’s Way to Wellville. 2019. Neighborhood Engagement. Available at: https://www.spartanburgwellville.com/initiatives/neighborhoodengagement (accessed June 18, 2019.)
- National Heart, Lung, and Blood Institute. 2017. Health Disparities. Available at: https://www.nhlbi.nih.gov/health/educational/healthdisp/ (accessed June 1, 2020).
- Office of Disease Prevention and Health Promotion. 2020. The Secretary’s Advisory Committee for 2030: Committee Reports and Meetings. Available at: https://www.healthypeople.gov/2020/About-Healthy-People/Development-Healthy-People-2030/Committee-Meetings (accessed June 1, 2020).
- Olayiwola, J. N., S. Sheth, V. Mleczko, A. L. Choi, and A. E. Sharma. 2016. The impact of the patient-centered medical home on health disparities in adults: A systematic review of the evidence. Journal of Health Disparities Research and Practice 10(4):68-96. Available at: https://digitalscholarship.unlv.edu/cgi/viewcontent.cgi?article=1466&context=jhdrp (accessed June 1, 2020).
- Osborne, H. 2004. Health and literacy working together: A health literacy conference for new readers & health professionals. Available at: https://healthliteracy.com/2004/09/06/new-readers/ (accessed June 1, 2020).
- Osborne, H., and A. Willard. 2008. Health literacy out loud. In Archie Willard Talks about Struggling to Read (HLOL #3). Available at: https://healthliteracy.com/2008/10/20/archie-willard-talks-about-struggling-to-read-hlol-3/ (accessed June 1, 2020).
- Patient-centered outcomes research. 2010. Public Law 111-148, Statute 727, Code 124, Section 6301.
- PCORI. 2018. Glossary. Available at: https://www.pcori.org/glossary (accessed June 1, 2020).
- PCORI. 2019. Addressing Disparities. Available at: https://www.pcori.org/topics/addressing-disparities (accessed June 1, 2020).
- PFCCpartners. 2020. Health Systems. Available at: https://pfccpartners.com/los-angeles-countydepartment-of-health-services/ (accessed June 1, 2020).
- Project ECHO. 2020. ECHO Movement Overview. Available at: https://echo.unm.edu/data/movement (accessed June 1, 2020).
- Ramachandran, A., F. R. Snyder, M. L. Katz, J. S. Darnell, D. J. Dudley, S. R. Patierno, M. R. Sanders, P. A. Valverde, M. A. Simon, V. Warren-Mears, T. A. Battaglia, and the Patient Navigation Research Program Investigators. 2015. Barriers to Health Care Contribute to Delays in Follow-Up Among Women with Abnormal Cancer Screening: Data from the Patient Navigation Research Program. Cancer 121:4016-4024. https://doi.org/ 10.1002/cncr.29607
- Rambur, B. A. 2017. What’s at Stake in U.S. Health Reform: A Guide to the Affordable Care Act and Value-Based Care. Policy, Politics, and Nursing Practice 18(2):61-71. https://doi.org/10.1177/1527154417720935.
- Ramiah, K., B. Roberson, J. Schrag, K. Susman, B. Siegel, and M. White. 2016. Population Health at Essential Hospitals: Findings from Moving to Action for Hospitals and Population Health. America’s Essential Hospitals. Available at: https://essentialhospitals.org/wp-content/uploads/2016/11/RWJF-Roadmap_HighRes.pdf (accessed June 1, 2020).
- Rao, M. 2016. Talent, innovation, and place: A more relevant research university of the 21st century. Journal on Anchor Institutions and Communities 1:49-52. Available at: https://www.margainc.com/wp-content/uploads/2017/05/AITF_Journal_2016_Vol_1.pdf (accessed June 1, 2020).
- Robeznieks, A. 2019. New ICD-10 codes will help physicians tackle social barriers to care. Available at: https://www.ama-assn.org/practice-management/digital/new-icd-10-codes-will-help-physicians-tackle-social-barriers-care (accessed June 1, 2020).
- Rocque, G. B., M. Pisu, B. E. Jackson, E. A. Kvale, W. Demark-Wahnefried, M. Y. Martin, K. Meneses, Y. Li, R. A. Taylor, A. Acemgil, C. P. Williams, N. Lisovicz, M. Fouad, K. M. Kenzik, and E. E. Partridge. 2017. Resource Use and Medicare Costs During Lay Navigation for Geriatric Patients with Cancer. JAMA Oncology 3(6):817-825. https://doi.org/10.1001/jamaoncol.2016.6307.
- Rosenbaum, S. 2016. Hospitals as community hubs: Integrating community benefit spending, community health needs assessment, and community health improvement. Brookings Institute. Available at: https://www.brookings.edu/research/hospitals-as-community-hubs-integrating-community-benefit-spending-community-health-needsassessment-and-community-health-improvement/ (accessed June 1, 2020).
- Office of Disease Prevention and Health Promotion. 2018. Secretary’s Advisory Committee on National Health Promotion and Disease Prevention Objectives for 2030 Report #2. Available at: https://www.healthypeople.gov/2020/About-Healthy-People/Development-Healthy-People-2030/Advisory-Committee (accessed June 1, 2020).
- Singh, S. R., G. J. Young, L. Loomer, and K. Madison. 2018. State-Level Community Benefit Regulation and Nonprofit Hospitals’ Provision of Community Benefits. Journal of Health Politics, Policy and Law 43(2):229-269. https://doi.org/10.1215/03616878-4303516.
- Smith, J. C. and C. Medalia. 2015. Health Insurance Coverage in the United States: 2014. Current Population Reports: 60-253. Available at: https://www.census.gov/content/dam/Census/library/publications/2015/demo/p60-253.pdf (accessed June 1, 2020).
- House of Representatives. 2019. Social Determinants Accelerator Act of 2019. H.R. 4004. Available at: https://www.congress.gov/bill/116th-congress/house-bill/4004?s=1&r= (accessed June 1, 2020).
- Robert Wood Johnson Foundation. 2015. Spartanburg County, SC: 2015 Culture of Health Prize Winner. Available at: https://www.rwjf.org/en/library/articles-and-news/2015/10/coh-prize-spartanburg-sc.html (accessed June 1, 2020).
- University of Vermont Medical Center. 2019. Strategic Initiatives. Available at: https://www.uvmhealth.org/medcenter/pages/quality-of-care/hospital-report-card/strategic-initiatives.aspx (accessed June 1, 2020).
- Strongwater, S., L. Martino, and W. Boyd. 2018. How to integrate empathy into daily care. New England Journal of Medicine Catalyst. Available at: https://catalyst.nejm.org/integrate-empathy-forums-daily-work/ (accessed June 1, 2020).
- Sulzer, S. H. 2017. Moving into Relational Empathy to Address Health Disparities. Medical Education 51(11):1097-1098. https://doi.org/10.1111/medu.13451.
- Swensen, S., A. Kabcenell, and T. Shanafelt. 2016. Physician-Organization Collaboration Reduces Physician Burnout and Promotes Engagement: The Mayo Clinic Experience. Journal of Healthcare Management 61(2):105-127. Available at: https://pubmed.ncbi.nlm.nih.gov/27111930/ (accessed June 1, 2020).
- The Aspen Institute. 2020. Glossary for Understanding the Dismantling Structural Racism/Promoting Racial Equity Analysis. Available at: https://assets.aspeninstitute.org/content/uploads/fi les/content/docs/rcc/RCC-Structural-Racism-Glossary.pdf (accessed June 1, 2020).
- Tsasis, P., N. Nadesan, K. Kuttiyappan, and L. D. Lin. 2017. Lessons Learned in Implementing Patient Family Advisory Councils in Ontario. Journal of Participatory Medicine May 9( 9:e10). Available at: https://participatorymedicine.org/journal/evidence/research/2017/05/09/lessons-learned-inimplementing-patient-family-advisory-councils-inontario/ (accessed June 1, 2020.)
- U.S. Department of Health and Human Services. 2018. Social Determinants of Health. Available at: https://www.healthypeople.gov/2020/topics-objectives/topic/social-determinants-of-health (accessed June 1, 2020).
- U.S. Department of Veterans Affairs. 2020. Office of Health Equity. Available at: https://www.va.gov/healthequity/ (accessed June 1, 2020.)
- University of Vermont Medical Center. 2019. 2019 Community Health Needs Assessment: Chittenden and Grand Isle Counties, Vermont. Available at: https://www.uvmhealth.org/medcenter/pages/about-uvm-medical-center/the-community/needs-assessment.aspx (accessed June 1, 2020).
- Van Winkle, L. J., B. D. Schwartz, and N. Michels. 2017. A Model to Promote Public Health by Adding Evidence-Based, Empathy-Enhancing Programs to All Undergraduate Health-Care Curricula. Frontiers in Public Health 5:339. https://doi.org/10.3389/fpubh.2017.00339
- Vartorella, L. 2017. Diversity and inclusion in 2017: 5 questions with Kaiser Permanente CDIO Dr. Ronald Copeland. Available at: https://www.beckershospitalreview.com/hospital-management-administration/diversity-and-inclusion-in-2017-5-questionswith-kaiser-permanente-cdo-dr-ronald-copeland.html (accessed June 1, 2020).
- Weinberger, A. H., M. Gbedemah, A. M. Martinez, D. Nash, S. Galea, and R. D. Goodwin. 2018. Trends in depression prevalence in the USA from 2005 to 2015: Widening disparities in vulnerable groups. Psychological Medicine 48(8):1308-1315. https://doi.org/10.1017/S0033291717002781
- Wells, K. J., P. Valverde, A. E. Ustjanauskas, E. A. Calhoun, and B. C. Risendal. 2018. What are patient navigators doing, for whom, and where? A national survey evaluating the types of services provided by patient navigators. Patient Education and Counseling 101(2):285-294. https://doi.org/10.1016/j.pec.2017.08.017
- Wesson, D., H. Kitzman, K. H. Halloran, and K. Tecson. 2018. Innovative population health model associated with reduced emergency department use and inpatient hospitalizations. Health Affairs 37(4):543-550. https://doi.org/10.1377/hlthaff .2017.1099.
- White, M., Deborah Roseman, Brian Roberson, and K. Ramiah. 2019. Outside the Hospital Walls: An Update on Essential Hospitals’ Efforts to Improve the Health of Their Communities. Essential Hospitals Institute. Available at: https://essentialhospitals.org/wp-content/uploads/2020/01/EHI-CIHC-Progress-Report-December-2019.pdf (accessed June 1, 2020).
- White, M., H. Lambalot, B. Roberson, D. Roseman, and K. Ramiah. 2019. Milestones for community-integrated health care at essential hospitals. Essential Hospitals Institute. Available at: https://essentialhospitals.org/wp-content/uploads/2020/01/EHI-Milestones-to-CIHC-December-2019.pdf (accessed June 1, 2020).
- Office of Disease Prevention and Health Promotion. 1999. Wired for health and well-being: The emergence of interactive health communication. Washington, D.C.: U.S. Dept. of Health and Human Services.
- World Health Organization. 1946. Constitution of the world health organization. World Health Organization. Available at: https://www.who.int/governance/eb/who_constitution_en.pdf (accessed June 1, 2020).
- Wyatt, R., M. Laderman, L. Botwinick, K. Mate, and J. Whittington. 2016. Achieving health equity: A guide for health care organizations. Cambridge, Massachusetts: Institute for Healthcare Improvement. Available at: http://www.ihi.org/resources/Pages/IHIWhitePapers/Achieving-Health-Equity.aspx (accessed June 1, 2020).