Partnering to Tackle the Obesity Epidemic: How Employers are Rethinking Obesity to Better Address Care, Treatment, and Engagement with Their Employees
Obesity, overweight, and associated chronic diseases continue to be major threats to the health of individuals and the greater population. There is now more evidence than ever that connects obesity and related diseases with downstream effects such as reduced productivity, threatening the economic viability of employers and larger society. Overweight and obesity have been linked with diabetes, sleep apnea, hypertension, and musculoskeletal issues such as back and knee disabilities [1]. All of these chronic health issues can cause increased absenteeism from work, reduce productivity, and add significantly to health care plan spending.
In addition to the personal costs of obesity on quality of life, the associated medical costs and impact to the health care system are astounding. A 2016 analysis estimates that direct medical costs for obesity and related conditions (such as diabetes) and these conditions’ indirect costs (such as absenteeism, presenteeism, and other lost work productivity) total $1.42 trillion yearly for the United States alone [2]. This figure far exceeds previous estimates of $147 to $210 billion attributed to obesity and related conditions [3].
The number of people in the United States who have been diagnosed with obesity has steadily increased, with recent prevalence estimated to be approximately 40 percent of the overall population. However, when including the number of people with overweight, the prevalence increases to nearly 70 percent of the overall population [4]. In response to these statistics, the authors suggest that individual employees, employers, third-party insurance payers, and health care providers play a major role in helping solve the current problem with obesity and overweight, to ensure both the health of their employees and the long-term health and prosperity of the nation’s workforce.
In this article, the authors outline key areas for education and recommendations for employers, specifically highlighting the My Healthy Weight program. These resources support employers, employees, and families in more actively addressing issues with obesity.
Current Obesity Care
The thinking around the development of obesity has changed dramatically in recent years. While obesity was previously seen as an issue of individual choice, emerging science has expanded understanding to include the contributions of behavior, genetics, and community environment, allowing development of new, more personalized care for those with obesity or overweight.
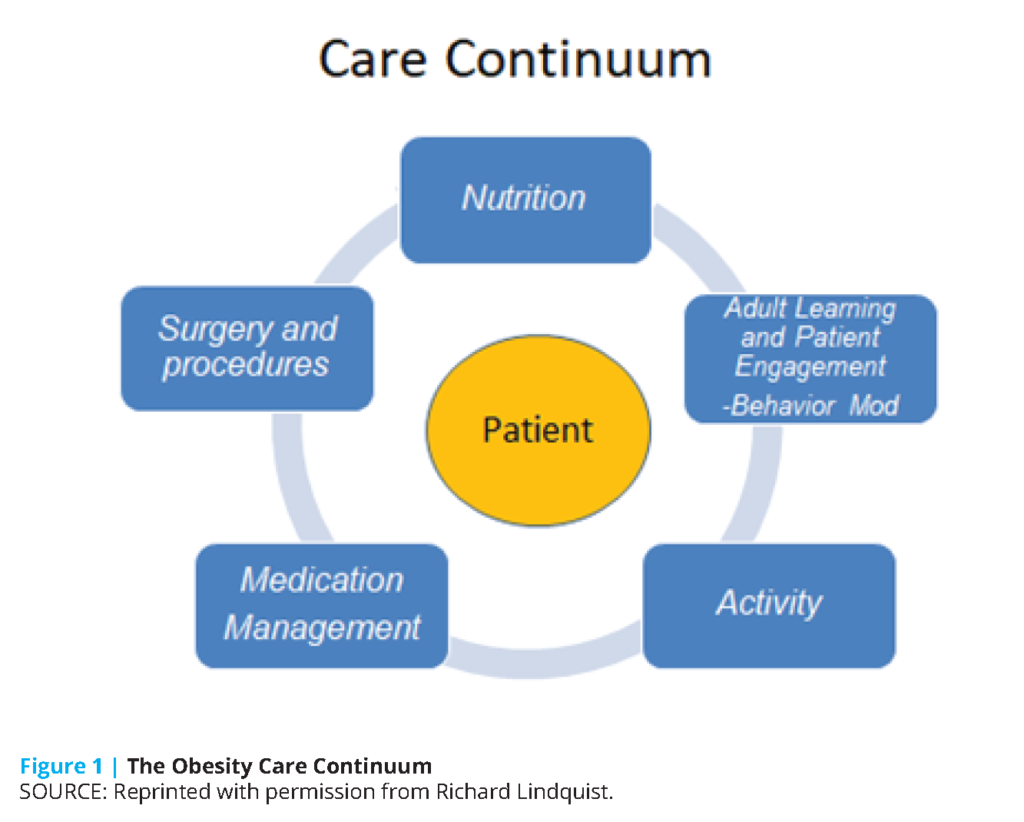
Changing awareness of the drivers and consequences of overweight and obesity allow use of improved strategies in prevention, treatment, and maintenance in clinical settings. Current best practices for obesity care include use of a Care Continuum model that allows a patient to comprehensively address their individual circumstances (see Figure 1). Improved understanding of nutritional and activity approaches is combined with knowledge of effective learning and behavior modification strategies to help provide practical weight management tools. Also, use of new medications to control hunger and improved bariatric and metabolic surgical approaches provide an array of useful tools not previously available.
Numerous barriers exist to providing effective financial support for addressing obesity management on both individual and population bases. Many insurance plans either directly exclude obesity care or require specific criteria that neither employers nor employees may know exists. The current health care system has only recently recognized obesity as a disease, and the lack of appropriate insurance coding of obesity to facilitate billing and reimbursement of services, as well as ineffective payment models, needs to be reviewed and addressed.
Additionally, both individuals with obesity and care providers are challenged by biases inherited from the health care approach. Patients know that weight loss is not easy, and with many having failed multiple times to sustain weight loss, they have mistakenly assumed the problem was unique to them, rather than understanding obesity as an environmental or genetic issue. Providers often want to help patients better manage their weight, but due to the provider’s limited education or lack of time, patients are often inadequately diagnosed or not regularly monitored for specific obesity-related medical visits [5].
The Employer Perspective
Employers have long focused on developing “healthy cultures” that support their workforce. The fact that 85 percent of organizations with 1,001-10,000 employees have implemented employee wellness programs shows significant interest in supporting employees in improving or maintaining a healthy lifestyle [6]. Research, however, has indicated that obesity prevalence remains a significant challenge for organizations. Despite the best intentions, traditional wellness programs have not been shown to be effective in helping care for individuals with obesity, and employees hold the widespread perception that they are ineffective [5]. This ineffectiveness is in part because a majority of wellness programs have focused on addressing obesity only through weight management programs, instead of taking a more holistic approach. Some employers do cover or partially subsidize the cost of onsite weight management programs, while others offer incentives for participation in their company’s weight management program. However, this will only go so far to continuously engage employees and help them maintain their health status.
Emerging science demonstrates that a more comprehensive—and fresh—approach to addressing obesity is needed to more effectively support individuals with obesity. This includes looking at obesity as a disease, viewing it in a similar manner to how employers see chronic diseases, such as diabetes or heart disease.
Employers are seeking effective strategies that will support their overall workforce. Such strategies include considering a combination of programs and policies and developing a culture that reduces stigma and promotes a more inclusive and positive environment for all employees. In addition, companies are addressing health data challenges and re-evaluating their benefit design approach, so employees can better navigate the health care system and become more proactive consumers in managing their health and that of their families.
My Healthy Weight Initiative
The My Healthy Weight Initiative (MHW) represents one initiative to align employers’ obesity benefit offerings to offer more consistent coverage across insurance benefit designs. Launched in November 2017, MHW is the first collective initiative offering insurance benefits to cover obesity prevention and treatment for both children and adults [7]. Funded by the Robert Wood Johnson Foundation and spearheaded by the Bipartisan Policy Center, MHW brought together employers, insurers, state Medicaid plans, and key stakeholder organizations to create a task force to effectively address obesity prevention and early treatment coverage through the workplace in the United States.
The yearlong work of the taskforce resulted in a signed pledge in which founding members committed to offering consistent and comprehensive obesity benefit coverage. The pledge aims to create a consistent set of reimbursable services that will increase the likelihood that primary care providers will refer individuals to additional services, including follow-up care. The pledge’s components include screening and follow-up visits that align with the current US Preventive Services Task Force recommendations, community-based and evidence-based programs, and a commitment to engage employees around obesity prevention and treatment. With over 10.5 million people currently in networks that offer MHW, the goal is to scale the program so that every individual has access to critical obesity care options. MHW lays the foundation for employers to engage their employees and ensure that obesity and overweight is addressed in a comprehensive way.
Next Steps
Offering consistent obesity benefits is just the beginning of a sustainable solution for employers to effectively address obesity, but other strategies addressing payment structures should also be considered. For example, current payment structures, such as high-deductible health plans, often create a barrier for many employees, particularly those with lower wages. The authors suggest that self-insured employers consider either reducing or eliminating copays, or offer a health savings account (HSA) to encourage use of services that directly benefit health and productivity. Furthermore, employers should consider using obesity competencies as a guide to offer support to employees, so they can be empowered with current knowledge and skills and better manage their obesity. A set of obesity competencies has been developed to improve training of health care providers to prevent, manage, and treat obesity [8]. Provider training under these competencies includes information on the correlation among obesity, co-morbid conditions, and the impact of long-term toxic stress to employees.
With My Healthy Weight, employers have an opportunity to cover obesity prevention and treatment benefit offerings that are evidence-based, align with current expert recommendations, and are consistent with other employers across the United States. The cost of not doing anything far outweighs any investment to engage employees on obesity prevention and treatment.
Join the conversation!
![]() Tweet this! Obesity and associated chronic diseases continue to be major threats to the health of individuals and the greater population. This #NAMPerspectives discusses what employers can do to engage with their employees and support their workforce: https://doi.org/10.31478/201906a
Tweet this! Obesity and associated chronic diseases continue to be major threats to the health of individuals and the greater population. This #NAMPerspectives discusses what employers can do to engage with their employees and support their workforce: https://doi.org/10.31478/201906a
![]() Tweet this! Individuals with obesity and their care providers are often challenged by biases inherited from a traditional health care approach. How employers can contribute to a more holistic and inclusive approach to care: https://doi.org/10.31478/201906a #NAMPerspectives
Tweet this! Individuals with obesity and their care providers are often challenged by biases inherited from a traditional health care approach. How employers can contribute to a more holistic and inclusive approach to care: https://doi.org/10.31478/201906a #NAMPerspectives
![]() Tweet this! Emerging science demonstrates that a more comprehensive approach is needed to support people with obesity — including acknowledging it as a chronic disease. This #NAMPerspectives discusses how employers can work to support their employees: https://doi.org/10.31478/201906a
Tweet this! Emerging science demonstrates that a more comprehensive approach is needed to support people with obesity — including acknowledging it as a chronic disease. This #NAMPerspectives discusses how employers can work to support their employees: https://doi.org/10.31478/201906a
Download the graphics below and share them on social media!
References
- Centers for Disease Control and Prevention (CDC). 2018. Adult obesity facts. Available at: https://www.cdc.gov/obesity/data/adult.html (accessed December 13, 2018).
- Waters, H., and R. J. M. I. DeVol. 2016. Weighing down America: The health and economic impact of obesity. Santa Monica, CA: Milken Institute. Available at: https://milkeninstitute.org/reports/weighing-down-america-health-and-economic-impact-obesity (accessed September 2, 2020).
- Cawley, J., and C. Meyerhoefer. 2012. The medical care costs of obesity: An instrumental variables approach. Journal of Health Economics 31(1):219-230. https://doi.org/10.1016/j.jhealeco.2011.10.003
- CDC. 2018. Obesity and overweight. Available at: https://www.cdc.gov/nchs/fastats/obesity-overweight.htm (accessed December 13, 2018).
- Kaplan, L. M., A. Golden, K. Jinnett, R. L. Kolotkin, T. K. Kyle, M. Look, J. Nadglowski, P. M. O’Neil, T. Parry, K. J. Tomaszewski, B. Stevenin, S. K. Lilleore, and N. V. Dhurandhar. 2018. Perceptions of barriers to effective obesity care: Results from the national action study. Obesity 26(1):61-69. https://doi.org/10.1002/oby.22054
- Mattke, S., H. Liu, J. Caloyeras, C. Huang, K. Van Busum, D. Khodyakov, and V. Shier. 2013. Workplace wellness programs study: Final report. Santa Monica, CA: Rand Corporation. Available at: rand.org/pubs/research_reports/RR254.html (accessed September 2, 2020).
- Bipartisan Policy Center. 2017. My healthy weight. Available at: https://bipartisanpolicy.org/events/my-healthy-weight (accessed December 13, 2018).
- Bradley, D. W., W. H. Dietz, and Provider Training and Education Workgroup. 2017. Provider competencies for the prevention and management of obesity. Washington, DC: Bipartisan Policy Center. Available at: https://bipartisanpolicy.org/wp-content/uploads/2019/03/Provider-Competencies-for-the-Prevention-and-Management-of-Obesity.pdf (accessed September 2, 2020).