Organizational Evidence-Based and Promising Practices for Improving Clinician Well-Being

Clinician burnout is an occupational syndrome driven by the work environment [1,2,3]. An organization seeking to reduce burnout and improve well-being among its clinicians can create a better work environment by aligning its commitments, leadership structures, policies, and actions with evidence-based and promising best practices. In this discussion paper, the authors outline organizational approaches that focus on fixing the workplace, rather than “fixing the worker,” and by doing so, advance clinician well-being and the resiliency of the organization [4,5]. A resilient organization, or one that has matched job demands with job resources for its workers and that has created a culture of connection, transparency, and improvement, is better positioned to achieve organizational objectives during ordinary times and also to weather challenges during times of crisis.
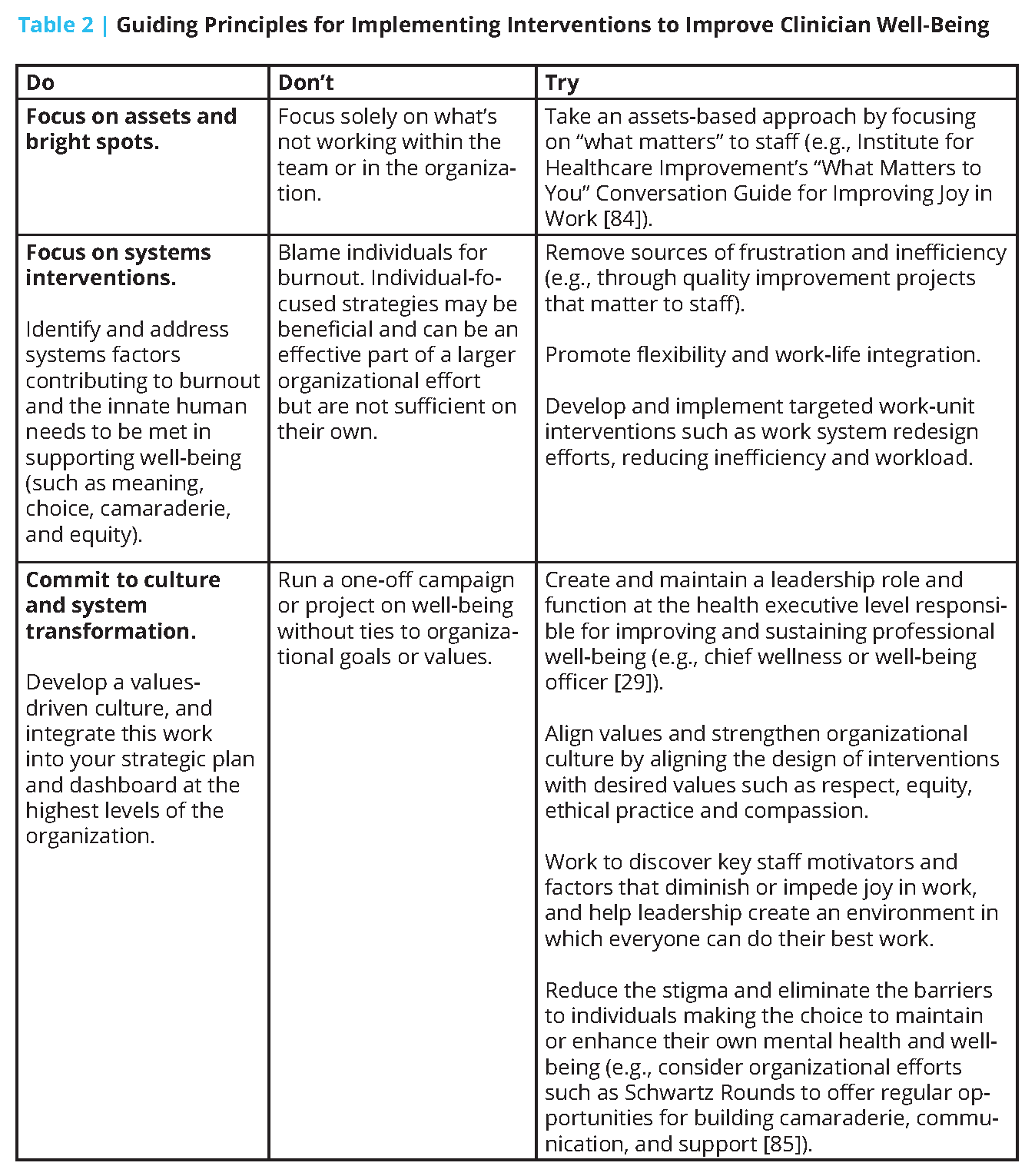
Evidence-based and promising practices shown to increase clinician well-being across six domains [6] are presented in this discussion paper: (1) organizational commitment, (2) workforce assessment, (3) leadership (including shared accountability, distributed leadership, and the emerging role of a chief wellness officer [CWO]), (4) policy, (5) efficiency of the work environment, and (6) support. We provide examples (see Table 1) along with principles of organizational action for clinician well-being (see Table 2).
This paper is intended for organizational leaders in health care settings, including governing boards, CWOs, Chief Medical Officers, Chief Nursing Officers, Chief Pharmacy Officers, service line directors, department chairs, and clinical learning environment directors. Drawing on recommendations from the recent National Academy of Medicine consensus study Taking Action Against Clinician Burnout: A Systems Approach to Professional Well-Being [1], this paper also aims to support the frontline clinician workforce, including physicians, dentists, advanced practice clinicians, nurses, pharmacists, occupational and physical therapists, and others, across all career stages and in diverse care settings.
Organizational Evidence-Based and Promising Practices
In this section, the authors describe the six domains of organizational evidence-based and promising practices and how they support organizational resiliency and improve clinician well-being. Specific tools for measurement and types of interventions that can be deployed are discussed in more detail in the following sections.
Domain 1: Organizational Commitment
A cross-cutting commitment to workforce well-being and organizational resilience is essential for preventing burnout within an organization. Just as the landmark report To Err is Human: Building a Safer Health System [7] called for a systems approach to patient safety, a systems-based commitment to clinician well-being is needed to create resilient organizations. This commitment can be manifested by adopting the principles of the Charter on Physician Well-Being [8], establishing a well-being program, appointing a CWO [9,10], and/or including measures of workforce well-being within the organization’s strategic plan and data dashboard.
Domain 2: Workforce Assessment
It is not possible to know how an organization—or any part of that organization—is performing without measurement of clinician well-being and burnout. Measurement is essential. Factors known to have an impact on well-being can also be measured, such as electronic health record (EHR)-use metrics of work outside of work and inbox volume [11,12,13], along with the costs of burnout [14,15] (including workforce turnover, early retirement, and reduced clinical effort). Additional leading indicators of clinician well-being, such as characteristic behaviors of leaders, including communicating transparently, nurturing career development, and expressing appreciation for completed work [16]; efficiency of the practice environment, such as team documentation and team order entry [17,18,19,20]; and aspects of organizational culture, such as teamwork and the availability and effectiveness of peer support, can also be measured. The results can be shared with stakeholders, such as unit leaders and the organization’s board, and, subsequently, leaders across the organization can be held mutually responsible for addressing and improving the results [21].
Domain 3: Leadership
Shared Accountability
By establishing shared accountability among an organization’s executive leadership team to achieve Quadruple Aim [22] outcomes (better care, better health, lower cost, and better workforce experience), an organization can structurally support a healthy work environment. For example, instead of a compliance officer and a chief information officer independently making decisions to protect the organization from an audit failure or technology security breach, their decisions could change and be better informed if they shared accountability for all critical aims of the organization, including patient access to care, productivity, workforce recruitment and retention, safe and reasonable clinical workloads, and clinician well-being. In addition, shared accountability means that responsibility for clinician well-being does not solely rest with one leader, but rather is embedded within the organizational structure/operations, and will persist across leadership changes.
Distributed Leadership
A corollary of shared accountability is distribution of a portion of authority and accountability to the professionals closest to the patients. As argued by submarine commander David Marquet, professionals respond better to an approach of “empower and encourage” rather than “command and control” [23]. This approach can be viewed as expressing intent instead of orders, a concept that has also been stated as “wide guardrails, thin rulebook.” In health care, this concept could be translated to “minimizing rules and focusing on only a few high-level outcomes.” Marquet emphasizes the importance of giving control to others, ensuring first that they have the competency and clarity of mission to safely assume that control, which in health care could mean training and empowering nurses to manage information within the EHR, apply independent judgment, and act on verbal orders. Marquet also highlights the need to provide regular feedback and suggests appropriate responses to those who are empowered to act, which in health care could mean encouraging teams to use Plan-Do-Study-Act cycles or lean approaches to design and continually improve their local workflows [24].
Balance of Standardization and Customization
Wise distribution of authority entails balancing the inherent tension between customization and standardization in optimizing clinical workflows [25,26]. The ideal balance varies by situation. Too much customization can be chaotic, time-consuming, and unpredictable in outcomes. Providing enough standardization of common work ensures that it is done reliably and, by default, frees clinicians to spend their cognitive bandwidth on the unique situations that require their expertise and can contribute to professional satisfaction.
On the other hand, too much standardization can be oppressive, disrespectful, and result in the inability of clinicians to adjust to their patients’ and their individual needs [27]. Standard design is built with the mean use case in mind. Yet, patients and clinicians present with wide variation in circumstances, clinical conditions, and preferences. At times, the care provider may be caught as the translator between the standard use case that drove the design and the unique individual who presents for care. The impossibility of serving both imperatives can contribute to moral distress and burnout.
Chief Wellness Officer
Organizations that strategically commit to building capacity and infrastructure to support clinician well-being through formal leadership positions, such as a CWO [28,29] with the expertise, resources, and authority to influence leaders and practices across the organization, will be more impactful than those whose investment is limited to informal champions and stand-alone committees. Without a CWO, ad hoc efforts to support clinician well-being often result in siloed initiatives and frustrated efforts. As the body of knowledge related to risk factors for burnout and interventions to promote well-being evolves and expands, there is a demand for specialization of personnel prepared to carry out transformative change within and across their organization. As such, organizations need centralized roles dedicated to well-being, elevated to the level of the executive leadership team [29,30].
An adaptive leadership approach is critical, given the complex and dynamic nature of ensuring well-being in the workforce. Identifying or developing the right leader with competencies and relational strengths for such an approach is essential. In addition to having the acumen for preserving and bolstering human capital within their organizations, such as emotional intelligence, innovation and strategic vision, executive presence, business skills, and change management expertise, the role requires experience in patient care delivery within the health care system. Adaptive leaders mobilize these strengths to transform processes and culture while embedding change capacity and resilience across the organization.
The transformative change and competency building needed to create a resilient organization requires time, resources, and patience. Organizations committed to addressing burnout and promoting a culture of well-being and resilience in their health care workforce may benefit from identifying and progressing through the following three phases of growth and maturation:
- Developing (resources and programming dedicated to education and mentoring);
- Improving (meaningful steps taken at the systems level to advance solutions); and
- Sustaining (a culture of commitment with adequately resourced infrastructure).
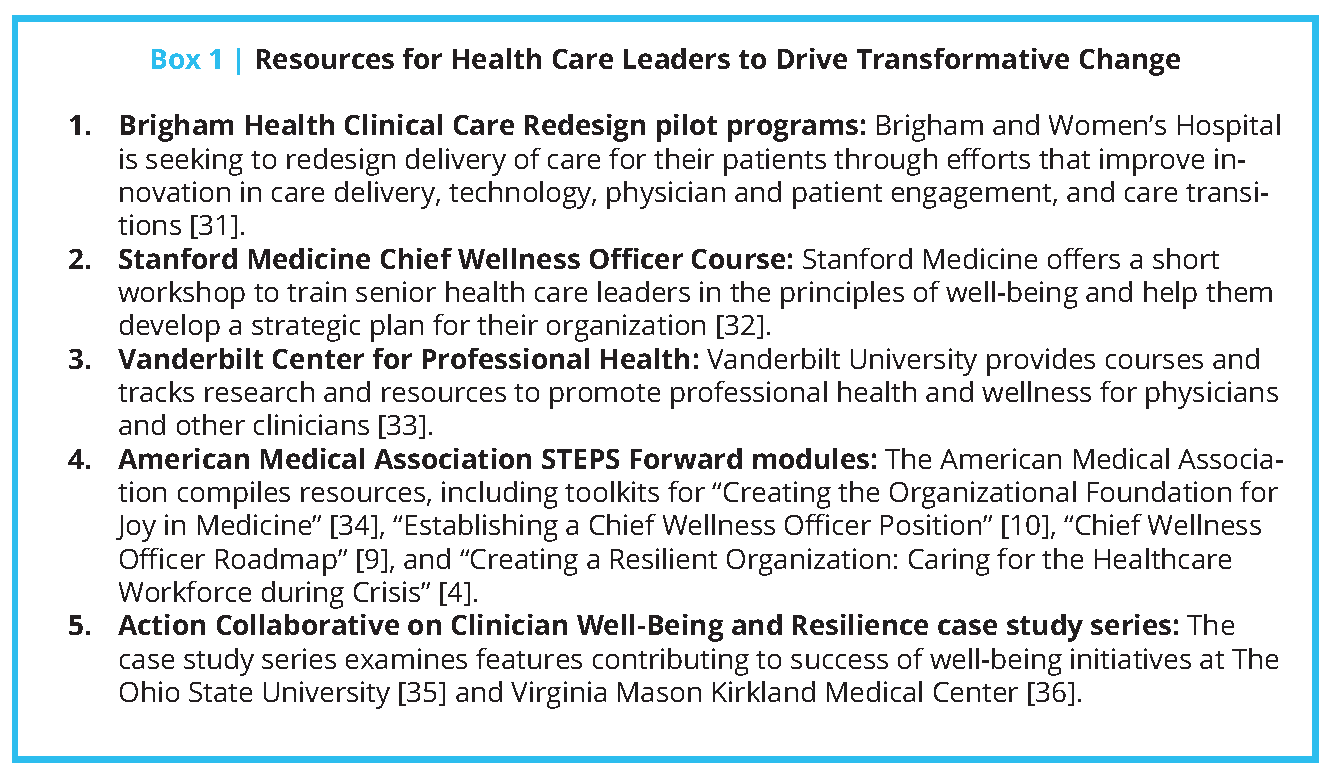
The authors have identified several promising case studies and tools that are available to leaders to apply and adapt to their organizations depending on their growth phase (see Box 1).
Domain 4: Policy
Clinicians may experience moral distress when the policies and practices of their organization conflict with their professional commitment to patient care and ability to do their work. A resilient organization will periodically reassess its policies and practices and eliminate those that are no longer relevant or no longer required [21,37,38]. Such practices and policies are generally well-intended, and may individually seem intuitive or innocuous, yet many are not evidence-based, and when taken in sum, can create an untenable work environment. For example, nurses spend nearly an hour of every four-hour shift charting or reviewing information in the EHR [40]; EHRs add to frustration for nurses [42] as well as physicians [12,13,43]. Much of this administrative work for nurses and physicians is driven by requirements that each add “only a few minutes” to the task, but multiplied over the hundreds of tasks per day, become hours of time away from patients.
Overly conservative interpretation of regulations, standards, and external guidance in the name of safety can paradoxically result in a less safe environment for patient care. When clinician time and cognitive bandwidth are diverted from clinical care to administrative tasks, quality and safety may suffer. Similarly, prioritizing the protection of the organization against an audit failure above other values, often by virtue of leadership structures (e.g., who is at the table, how accountability is distributed, the existence of a chief compliance officer but not a CWO) can leave clinicians adjudicating the tension between the needs of their patients and the policies of the organization.
Much of the burnout and frustration experienced by clinicians may originate in local over-interpretation of external regulations and guidance [44]. For example, some compliance professionals have concluded that the safest path around ambiguous or uncertain regulation is to create a local policy that only the licensed independent practitioner can record the visit note, manually enter orders, or make entries into the problem list within the EHR. Furthermore, some technology professionals have set short time-out intervals for all computer workstations no matter the location, whether a busy public hallway or a private office. In addition, some compliance professionals have adopted a nonbinding and non-evidence-based opinion that nurses and medical assistants (MAs) are required to sign in and out of the medical record when switching between clinical and clerical activities, fragmenting workflow and thought flow and interrupting teamwork. Such compartmentalized decision-making focuses the organization only on a narrow set of values or goals, putting at risk broader objectives, including safe and personalized patient care. This tension at the individual clinician level is also a source of moral distress.
During the COVID-19 public health emergency, the Centers for Medicare and Medicaid Services (CMS) issued emergency declaration blanket waivers [45], removing many nonessential policy barriers to teamwork and efficiency. For example, this waiver provides clinicians with additional flexibility related to verbal orders [37], reducing one of the major sources of administrative burden and burnout [37,43]. In addition, administrative hurdles for licensing, credentialing, and reappointments have been drastically reduced during the pandemic. Before the health care system and health care practitioners return to “business as usual,” institutions should systematically assess which processes and procedures are necessary for ensuring timely, high-quality patient care and which ones should be permanently retired.
Domain 5: Efficiency of Work Environment
Clinical excellence depends on operational efficiency. When systems are designed to support reliability and efficiency and when the right action happens by default, the humans within the system can use their finite cognitive bandwidth and emotional energy for what Cal Newport calls “deep work” [46]. Deep work is defined as “the ability to focus without distraction on a cognitively demanding task” [46]. When administrative tasks are intentionally minimized, there is more time for the important work of careful listening, nursing assessment, medical decision making, and relationship building with patients and colleagues. Yet, many clinicians believe that administrative and technology-focused tasks dominate their days [47]. This “shallow work” is logistical-style work, often performed while distracted. Arndt and colleagues determined that family physicians spend nearly as much time on security issues (i.e., user names and passwords) as they do reviewing their patients’ problem lists [48]. Furthermore, these physicians spend nearly an hour per day manually entering orders, another hour processing through a series of drop-down boxes for prescription renewal, nearly 90 minutes per day on inbox work, and hours per week on prior authorization requirements [49]. All of this time could be reduced by re-engineering workflows and empowering teamwork, allowing physicians to spend more time with their patients and engaging in “deep work.”
Inbasket messages, i.e., secure messages received from EHR systems, have become a drag on efficiency and a source of burnout. Adler-Milstein and colleagues found that primary care physicians and advanced practice providers (APPs) with more than 300 messages per week have six times the odds of burnout compared with those with less than 150 messages per week [12]. For comparison, the average family physician has approximately 100 inbox messages per day. Likewise, the hours that clinicians spend on computer work after hours is also predictive of burnout. Those with more than three hours per day of work outside of work (a.k.a. “pajama time”) had 13 times the odds of burnout compared with those who had less than 30 minutes per day of work outside of work [12].
EHR log data can be used to characterize the clinical work environment and measure the impact of policy and practice changes [11]. Intermountain Healthcare in Utah piloted an advanced team-based care model, increasing staffing ratios from one MA per physician to two MAs and providing real-time, in-room documentation and order-entry support. EHR log data demonstrated that after six months, physicians spent 20 percent less time documenting and 47 percent less time on order entry, while accommodating 20 percent more patient visits. Burnout in this small sample also decreased [50].
Domain 6: Support
The primary means by which an organization supports its clinicians is by giving them the ability to do their jobs—creating workflows and structures that foster teamwork, efficiency, and quality of care—and then allowing them to return safely home with time and emotional energy to engage in their personal lives with family, friends, and community.
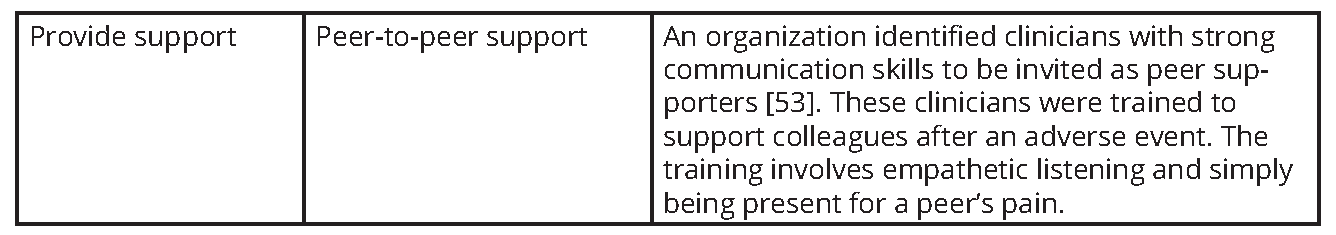
Another important means of support is by creating a culture of connection at work. This culture can be accomplished by structurally facilitating the organic development of friendships at work (i.e., by human-centered team meetings that begin with a few minutes of voluntary sharing or fun), by supporting peer-to-peer discussions (i.e., a buddy system [51] or small group dinners [52]) and by more formal structures, such as peer-to-peer support [53] and peer coaching [54] programs.
Measurement
Shared accountability for clinician well-being is dependent on measurement of burnout, its potential drivers, and its consequences. Organizations should perform periodic assessments of the following:
- Clinician well-being, using one of several validated instruments (i.e., Maslach Burnout Inventory [55], Mayo Well-Being Index [56], Stanford Professional Fulfillment Index [57], or the Mini-Z burnout assessment [58,59]);
- Departmental or business unit-level leadership qualities [16] (i.e., a survey of leaders’ direct reports);
- The efficiency of the practice environment [60] (i.e., by EHR-use metrics [11] and assessing team structure and function [20]);
- Culture and trust in the organization (i.e., Agency for Healthcare Research and Quality Patient Safety Culture Surveys [61]; Mini-Z [62]);
- Organizational cost of clinician burnout [15]; and
- Workforce recruitment and retention [63] (i.e., through measures of intention to cut back clinical effort or leave the organization).
Organizations should also be transparent regarding the results of these measurements. Furthermore, it could be considered best practice for leaders to share the results of these annual measures of burnout, its drivers, and consequences with their governing board as well as with their workforce.
Interventions
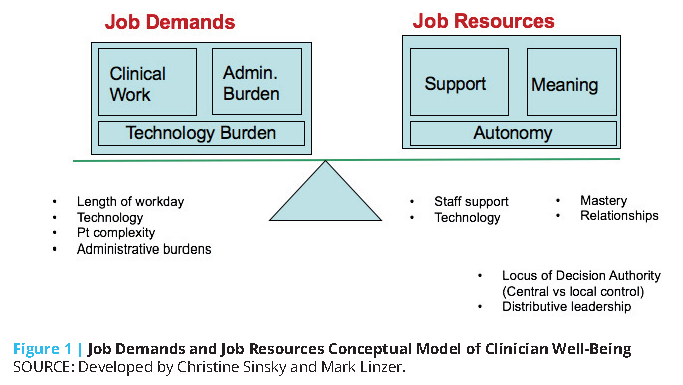
Clinician well-being is enhanced when there is a balance between job demands and job resources (see Figure 1). Job demands include clinical workload (i.e., work hours, patient volume, and patient complexity) along with administrative and technology burdens (i.e., EHR documentation, quality measurement attestation, and forms completion). Job resources include support (i.e., team-based care models, staffing ratios, optimized technology), meaning (i.e., relationships with patients and team, clinical mastery, ability to deliver optimal care) and autonomy (i.e., control over the work environment, schedule, workflows).
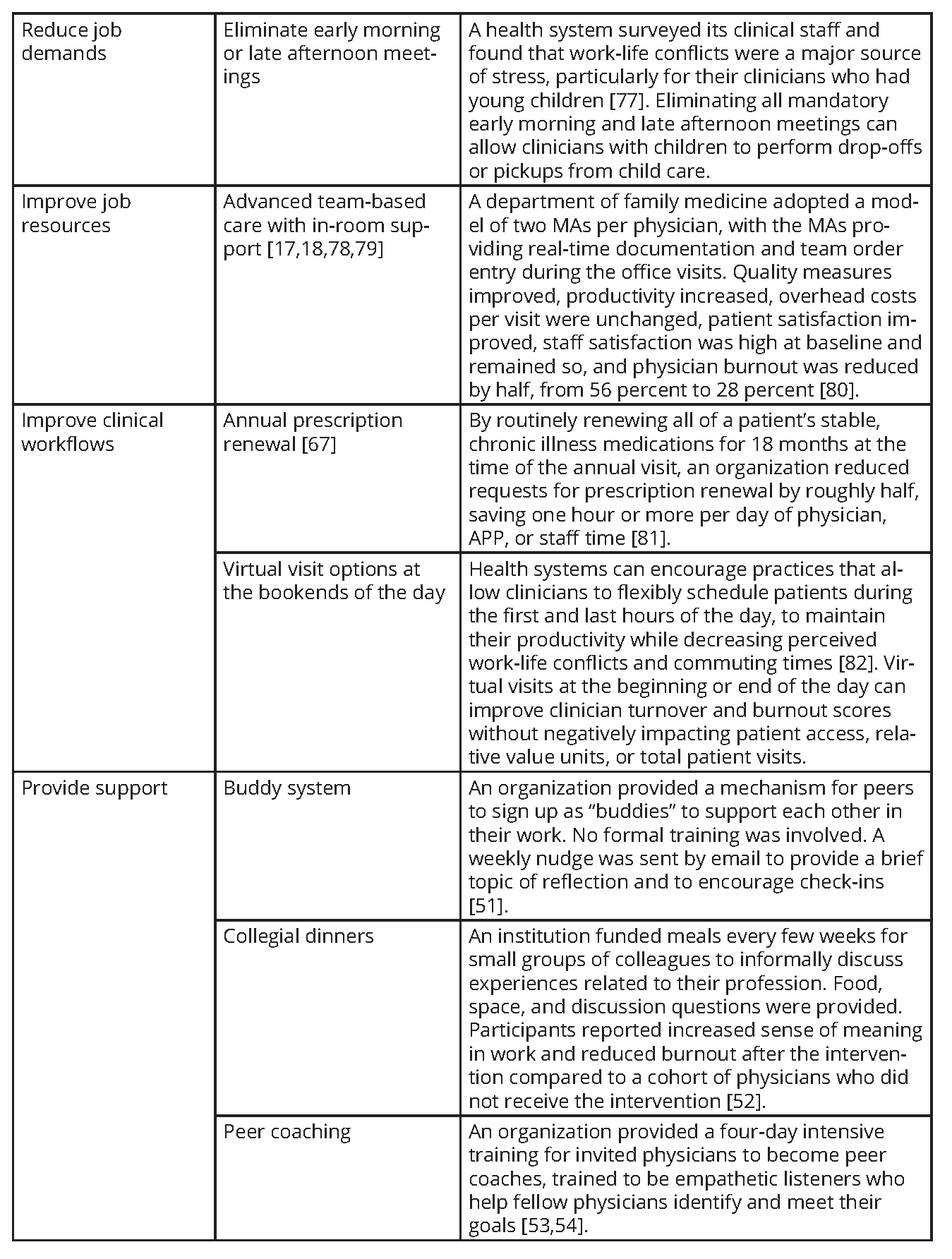
Clinician well-being can be improved by interventions directed toward the individual worker and toward the organization [64]. Two systematic reviews found that both types of interventions were associated with reductions in burnout, but that organization-level interventions were more effective [52,65]. Individual-level interventions include mindfulness training, gratitude practices, stress management training, health coaches, and small group curricula [66]. Organizational interventions included reducing job demands, improving job resources, fostering communication between clinicians, cultivating a sense of teamwork, increasing job control, and improving clinical workflows. As highlighted in Taking Action Against Clinician Burnout: A Systems Approach to Professional Well-Being [1], the overall quality of the existing evidence for effective interventions is relatively low, with few randomized trials, limited measurement of long-term effects, and few multisite studies. To address the overall lack of high-quality evidence, large organizations and professional associations can be involved in the design and funding of implementation research to help build the evidence base.
The set of principles below can help guide organizations in the selection and implementation of interventions to improve clinician well-being. A step-wise approach to selecting and implementing interventions to improve clinician well-being includes:
- Solicit ideas from all levels of stakeholders, including front-line clinical staff (e.g., via surveys, interviews, focus groups, or existing data sources like employee engagement surveys and exit interviews);
- Identify interventions that align with other organizational priorities (e.g., advanced team-based care reduces burnout and improves patient access [18]);
- Look for interventions that simultaneously improve clinician well-being and patient experience (e.g., workflow improvements such as annual prescription renewal can reduce clinician workload and improve patient medication adherence [67];
- Identify metrics to assess the impact of implementing the intervention;
- Engage front-line clinicians in the planning, implementation, and assessment of the pilot;
- Pilot interventions with small groups of clinicians and patients before rolling out more broadly; and
- Transparently share learnings from the pilot with staff and iterate to improve the effectiveness of the intervention.
In Table 1, the authors provide an overview of selected organizational interventions that are focused on improving clinician well-being. These interventions were drawn from the expertise of individual members of the NAM Action Collaborative on Clinician Well-Being and Resilience, in addition to published reports.
In Table 2, the authors provide guiding principles for implementation of evidence-based and promising practices based on the experiences of the authors and adapting the Institute for Healthcare Improvement’s framework for improving joy in work [83].
Conclusion
Akin to the patient safety and quality movement of the 1990s that transformed care delivery, not by asking individual clinicians to try harder, but by building safer systems, today’s growing clinician well-being movement will be most successful not by admonishing individual clinicians to be more resilient, but by creating more resilient organizations. Now more than ever, health care institutions should become more resilient by committing to workforce well-being as an organizational priority, regularly assessing and reporting burnout and its drivers, sharing accountability for organizational outcomes across leadership roles, periodically evaluating and de-implementing non-evidenced based policies, intentionally measuring and improving the efficiency of the work environment, and creating a culture of connection and support for clinicians.
Join the conversation!
![]() Tweet this! “Today’s growing clinician well-being movement will be most successful not by admonishing individual clinicians to be more resilient, but by creating more resilient organizations.” Read more strategies in a new #NAMPerspectives: https://doi.org/10.31478/202011a #ClinicianWellBeing
Tweet this! “Today’s growing clinician well-being movement will be most successful not by admonishing individual clinicians to be more resilient, but by creating more resilient organizations.” Read more strategies in a new #NAMPerspectives: https://doi.org/10.31478/202011a #ClinicianWellBeing
![]() Tweet this! Shared accountability ensures responsibility for #ClinicianWellBeing doesn’t rest with 1 leader but is embedded within the organizational structure/operations. Learn how an org can structurally support a healthy work environment: https://doi.org/10.31478/202011a #NAMPerspectives
Tweet this! Shared accountability ensures responsibility for #ClinicianWellBeing doesn’t rest with 1 leader but is embedded within the organizational structure/operations. Learn how an org can structurally support a healthy work environment: https://doi.org/10.31478/202011a #NAMPerspectives
![]() Tweet this! Improving #ClinicianWellBeing requires commitment at the organizational level, but also the involvement of employees throughout the system to co-create realistic solutions. Read more guiding principles in a new #NAMPerspectives: https://doi.org/10.31478/202011a
Tweet this! Improving #ClinicianWellBeing requires commitment at the organizational level, but also the involvement of employees throughout the system to co-create realistic solutions. Read more guiding principles in a new #NAMPerspectives: https://doi.org/10.31478/202011a
Download the graphics below and share them on social media!
References
- National Academies of Sciences, Engineering, and Medicine. 2019. Taking Action Against Clinician Burnout: A Systems Approach to Professional Well-Being. Washington, DC: The National Academies Press. https://doi.org/10.17226/25521
- Dzau, V. J., D. G. Kirch, and T. J. Nasca. 2018. To Care Is Human—Collectively Confronting the Clinician-Burnout Crisis. New England Journal of Medicine 378(4):312-314. https://doi.org/10.1056/NEJMp1715127
- Dyrbye, L. N., T. D. Shanafelt, C. A. Sinsky, P. F. Cipriano, J. Bhatt, A. Ommaya, C. P. West, and D. Meyers. 2017. Burnout among health care professionals: A call to explore and address this underrecognized threat to safe, high-quality care. NAM Perspectives. Discussion Paper, National Academy of Medicine, Washington, DC. https://doi.org/10.31478/201707b
- Shanafelt T. D., J. Ripp, M. Brown, and C. A. Sinsky. 2020. Creating a Resilient Organization: Caring for Healthcare Workers during Crisis. American Medical Association. Available at: https://www.ama-assn.org/system/files/2020-05/caring-for-health-careworkers-covid-19.pdf (accessed September 24, 2020).
- West C. P., L. N. Dyrbye, P. J. Erwin, and T. D. Shanafelt. 2016. Interventions to prevent and reduce physician burnout: a systematic review and meta-analysis. Lancet 388(10057):2272-2281. https://doi.org/10.1016/S0140-6736(16)31279-X
- American Medical Association. 2020. Joy in Medicine: Health System Recognition Program. American Medical Association: Washington, DC.
- Institute of Medicine. 2000. To Err Is Human: Building a Safer Health System. Washington, DC: The National Academies Press. https://doi.org/10.17226/9728
- Thomas, L. R., J. A. Ripp, and C. P. West. 2018. Charter on Physician Well-being. JAMA 319(15):1541-1542. https://doi.org/10.1001/jama.2018.1331
- Shanafelt T. D., and C. A. Sinsky. 2020. Chief Wellness Officer Roadmap: Implement a Leadership Strategy for Professional Well-Being. AMA STEPS Forward. Available at: https://edhub.ama-assn.org/steps-forward/module/2767764 (accessed June 25, 2020).
- Shanafelt T. D., and C. A. Sinsky. 2020. Establishing a Chief Wellness Officer Position: An Organizational Roadmap: Create the Organizational Groundwork for Professional Well-Being. AMA STEPS Forward. Available at: https://edhub.ama-assn.org/steps-forward/module/2767739 (accessed June 25, 2020).
- Sinsky, C. A., A. Rule, G. Cohen, B. G. Arndt, T. D. Shanafelt, C. D. Sharp, S. L. Baxter, M. Tai-Seale, S. Yan, Y. Chen, J. Adler-Milstein, and M. Hribar. 2020. Metrics for assessing physician activity using electronic health record log data. Journal of the American Medical Informatics Association 27(4):639-643. https://doi.org/10.1093/jamia/ocz223
- Adler-Milstein, J., W. Zhao, R. Willard-Grace, M. Knox, and K. Grumbach. 2020. Electronic health records and burnout: Time spent on the electronic health record after hours and message volume associated with exhaustion but not with cynicism among primary care clinicians. Journal of the American Medical Informatics Association 27(4):531-538. https://doi.org/10.1093/jamia/ocz220
- Tai-Seale, M., E. C. Dillon, Y. Yang, R. Nordgren, R. L. Steinberg, T. Nauenberg, T. C. Lee, A. Meehan, J. Li, A. S. Chan, and D. L. Frosch. 2019. Physicians’ Well-Being Linked To In-Basket Messages Generated By Algorithms In Electronic Health Records. Health Affairs 38(7):1073-1078. https://doi.org/10.1377/hlthaff .2018.05509
- Han, S., T. D. Shanafelt, C. A. Sinsky, K. M. Awad, L. N. Dyrbye, L. C. Fiscus, M. Trockel, and J. Goh. 2019. Estimating the Attributable Cost of Physician Burnout in the United States. Annals of Internal Medicine 171(8):600-601. https://doi.org/10.7326/M18-1422
- Shanafelt, T., J. Goh, and C. Sinsky, 2017. The Business Case for Investing in Physician Well-being. JAMA Internal Medicine 177(12):1826-1832. https://doi.org/10.1001/jamainternmed.2017.4340
- Shanafelt, T. D., G. Gorringe, R. Menaker, K. A. Storz, D. Reeves, S. J. Buskirk, J. A. Sloan, and S. J. Swensen. 2015. Impact of organizational leadership on physician burnout and satisfaction. Mayo Clinic Proceedings 90(4):432-440. https://doi.org/10.1016/j.mayocp.2015.01.012
- Smith, P. C., C. Lyon, A. F. English, and C. Conry. 2019. Practice Transformation Under the University of Colorado’s Primary Care Redesign Model. Annals of Family Medicine 17(Suppl 1):S24-S32. https://doi.org/10.1370/afm.2424
- Sinsky, C. A., and T. Bodenheimer. 2019. Powering-Up Primary Care Teams: Advanced Team Care With In-Room Support. Annals of Family Medicine 17(4):367-371. https://doi.org/10.1370/afm.2422
- Linzer, M., S. Poplau, E. Grossman, A. Varkey, S. Yale, E. Williams, L. Hicks, R. L. Brown, J. Wallock, D. Kohnhorst, and M. Barbouche. 2015. A Cluster Randomized Trial of Interventions to Improve Work Conditions and Clinician Burnout in Primary Care: Results from the Healthy Work Place (HWP) Study. Journal of General Internal Medicine 30(8):1105-1111. https://doi.org/10.1007/s11606-015-3235-4
- Willard-Grace, R., D. Hessler, E. Rogers, K. Dube, T. Bodenheimer, and K. Grumbach. 2014. Team structure and culture are associated with lower burnout in primary care. Journal of the American Board of Family Medicine 27(2):229-238. https://doi.org/10.3122/jabfm.2014.02.130215
- Sinsky, C. A., and M. R. Privitera. 2018. Creating a “Manageable Cockpit” for Clinicians: A Shared Responsibility. JAMA Internal Medicine 178(6):741-742. https://doi.org/10.1001/jamainternmed.2018.0575
- Bodenheimer, T. and C. Sinsky. 2014. From Triple to Quadruple Aim: Care of the Patient Requires Care of the Provider. Annals of Family Medicine 12(6):573-576. https://doi.org/10.1370/afm.1713
- Marquet, L. D. 2013. Turn the Ship Around!: A True Story of Turning Followers into Leaders. New York: Penguin Publishing Group.
- Agency for Healthcare Research and Quality. 2020. Ways To Approach the Quality Improvement Process (Page 2 of 2). Agency for Healthcare Research and Quality. Available at: https://www.ahrq.gov/cahps/quality-improvement/improvement-guide/4-approach-qi-process/sect4part2.html (accessed September 24, 2020).
- Sinsky C. A., R. Roberts, and J. Beasley. In Press. Standardization vs Customization: Time to Rebalance Health Care. Annals of Family Medicine.
- Linzer, M., R. Levine, D. Meltzer, S. Poplau, C. Warde, and C. P. West. 2014. 10 Bold Steps to Prevent Burnout in General Internal Medicine. Journal of General Internal Medicine 29(1):18-20. https://doi.org/10.1007/s11606-013-2597-8
- Berwick, D. M., S. Loehrer, and C. Gunther-Murphy. 2017. Breaking the Rules for Better Care. JAMA 317(21):2161-2162. https://doi.org/10.1001/jama.2017.4703
- Ripp, J. and T. Shanafelt. 2020. The Health Care Chief Wellness Officer: What the Role Is and Is Not. Academic Medicine 95(9):1354-1358. https://doi.org/10.1097/ACM.0000000000003433
- Kishore, S., J. Ripp, T. Shanafelt, B. Melnyk, D. Rogers, T. Brigham, N. Busis, D. Charney, P. Cipriano, L. Minor, P. Rothman, J. Spisso, D. G. Kirch, T. Nasca, and V. Dzau. 2018. Making The Case For The Chief Wellness Officer In America’s Health Systems: A Call To Action. Health Affairs Blog. https://doi.org/10.1377/hblog20181025.308059
- Shanafelt, T., M. Trockel, J. Ripp, M. L. Murphy, C. Sandborg, and B. Bohman. 2019. Building a Program on Well-Being: Key Design Considerations to Meet the Unique Needs of Each Organization. Academic Medicine 94(2):156-161. https://doi.org/10.1097/ACM.0000000000002415
- Brigham and Women’s Hospital. n.d. Redesigning Care Across the Continuum. Available at: https://www.brighamandwomens.org/medical-professionals/clinical-care-redesign/redesigning-careacross-the-continuum (accessed September 24, 2020).
- Stanford Medicine WellMD. n.d. Chief Wellness Officer Course. Available at: https://wellmd.stanford.edu/center1/cwocourse.html (accessed September 24, 2020).
- Vanderbilt University Medical Center. n.d. Center for Professional Health. Available at: https://medsites.mc.vanderbilt.edu/cph/home (accessed September 24, 2020).
- Sinsky, C. A., T. D. Shanafelt, M. M. Murphy, P. de Vries, B. Bohman, K. Olson, R. J. Vender, S. Strongwater, and M. Linzer. 2019. Creating the Organizational Foundation for Joy in Medicine. AMA STEPS Forward. Available at: https://edhub.ama-assn.org/steps-forward/module/2702510 (accessed September 24, 2020).
- Cappelucci, K., M. Zindel, H. C. Knight, N. Busis, and C. Alexander. 2019. Clinician well-being at the Ohio State University: A case study. NAM Perspectives. Discussion Paper, National Academy of Medicine, Washington, DC. https://doi.org/10.31478/201908b
- Zindel, M., K. Cappelucci, H.C. Knight, N. Busis, and C. Alexander. 2019. Clinician well-being at Virginia Mason Kirkland Medical Center: A case study. NAM Perspectives. Discussion Paper, National Academy of Medicine, Washington, DC. https://doi.org/10.31478/201908c
- Sinsky, C. A., and M. Linzer. 2020. Practice and Policy Reset Post-COVID: Reversion, Transition or Transformation. Health Affairs 39(8). https://doi.org/10.1377/hlthaff .2020.00612
- Ashton, M. 2018. Getting Rid of Stupid Stuff. New England Journal of Medicine 379(19):1789-1791. https://doi.org/10.1056/NEJMp1809698
- Erickson, S. M., B. Rockwern, M. Koltov, R. M. McClean, and Medicine Practice and Quality Committee of the American College of Physicians. 2017. Putting Patients First by Reducing Administrative Tasks in Health Care: A Position Paper of the American College of Physicians. Annals of Internal Medicine 166(9):659-661. https://doi.org/10.7326/M16-2697
- Sinsky C., L. Colligan, L. Li, M. Prgomet, S. Reynolds, L. Goeders, J. Westbrook, M. Tutty, and G. Blike. 2016. Allocation of Physician Time in Ambulatory Practice: A Time and Motion Study in 4 Specialties. Annals of Internal Medicine 165(11):753-760. https://doi.org/10.7326/M16-0961
- Hendrich, A., M. P. Chow, B. A. Skierczynski, and Z. Lu. 2008. A 36-hospital time and motion study: how do medical-surgical nurses spend their time? The Permanente Journal 12(3):25-34. https://doi.org/10.7812/tpp/08-021
- Harris, D. A., J. Haskell, E. Cooper, N. Crouse, and R. Gardner. 2018. Estimating the association between burnout and electronic health record-related stress among advanced practice registered nurses. Applied Nursing Research 43:36-41. https://doi.org/10.1016/j.apnr.2018.06.014
- Shanafelt, T. D., L. N. Dyrbye, C. Sinsky, O. Hasan, D. Satele, J. Sloan, and C. P. West. 2016. Relationship Between Clerical Burden and Characteristics of the Electronic Environment With Physician Burnout and Professional Satisfaction. Mayo Clinic Proceedings 91(7):836-848. https://doi.org/10.1016/j.mayocp.2016.05.007
- American Medical Association. 2020. Debunking Regulatory Myths. American Medical Association. Available at: https://www.ama-assn.org/amaone/debunking-regulatory-myths (accessed April 22, 2020).
- Centers for Medicare and Medicaid Services. 2020. COVID-19 Emergency Declaration Blanket Waivers for Health Care Providers. US Department of Health and Human Services: Washington, DC.
- Newport, C. 2016. Deep Work: Rules for Focused Success in a Distracted World. New York: Grand Central Publishing.
- Sunstein, C. R. 2019. Sludge Audits. Harvard Public Law Working Paper. https://doi.org/10.1017/bpp.2019.32
- Arndt, B. G., J. W. Beasley, M. D. Watkinson, J. L. Temte, W. Tuan, C. A. Sinsky, and V. J. Gilchrist. 2017. Tethered to the EHR: Primary Care Physician Workload Assessment Using EHR Event Log Data and Time-Motion Observations. Annals of Family Medicine 15(5):419-426. https://doi.org/10.1370/afm.2121
- Casalino, L. P., S. Nicholson, D. N. Gans, T. Hammons, D. Morra, T. Karrison, and W. Levinson. 2009. What Does It Cost Physician Practices To Interact With Health Insurance Plans? Health Affairs 28(Suppl 1):w533-w543. https://doi.org/10.1377/hlthaff .28.4.w533
- Faatz, J. 2019. Personal Communication. November 16, 2019.
- Greenawald, M. 2020. PeerRxMed. Available at: https://www.peerrxmed.com/ (accessed April 26, 2020).
- West, C. P., L. N. Dyrbye, J. T. Rabatin, T. G. Call, J. H. Davidson, A. Multari, S. A. Romanski, J. M. Henriksen Hellyer, J. A. Sloan, and T. D. Shanafelt. 2014. Intervention to promote physician well-being, job satisfaction, and professionalism: a randomized clinical trial. JAMA Internal Medicine 174(4):527-533. https://doi.org/10.1001/jamainternmed.2013.14387
- Shapiro, J. 2020. Peer Support Programs for Physicians: Mitigate the Effects of Emotional Stressors Through Peer Support. AMA STEPS Forward. Available at: https://edhub.ama-assn.org/steps-forward/module/2767766 (accessed June 25, 2020).
- Berg, S. 2019. Cleveland Clinic’s doctor peer coaches build physician resiliency. American Medical Association. Available at: https://www.ama-assn.org/practice-management/physician-health/clevelandclinic-s-doctor-peer-coaches-build-physician (accessed April 26, 2020).
- Maslach, C., S. E. Jackson., M. P. Leiter, W. B. Schaufeli, and R. L. Schwab. 2019. Maslach Burnout Inventory (MBI). Available at: https://www.mindgarden.com/117-maslach-burnout-inventory (accessed April 25, 2020).
- Mayo Clinic. 2020. Well-Being Index. MedEd Web Solutions. Available at: https://www.mededwebs.com/well-being-index (accessed April 25, 2020).
- Stanford Medicine WellMD Center. 2020. Physician Wellness Research/Surveys. Available at: https://wellmd.stanford.edu/center1/survey.html (accessed April 25, 2020).
- Linzer, M., L. Guzman-Corrales, and S. Poplau. 2015. Physician Burnout: Improve Physician Satisfaction and Patient Outcomes. AMA STEPS Forward. Available at: https://edhub.ama-assn.org/steps-forward/module/2702509 (accessed May 27, 2020).
- Dyrbye, L. N., D. Meyers, J. Ripp, N. Dalal, S. B. Bird, and S. Sen. 2018. Pragmatic approach for organizations to measure health care professional wellbeing. NAM Perspectives. Discussion Paper, National Academy of Medicine, Washington, DC. https://doi.org/10.31478/201810b
- AMA STEPS Forward. 2018. Practice assessment: Find modules to optimize your practice. Available at: https://edhub.ama-assn.org/steps-forward/interactive/16830409 (accessed April 25, 2020).
- Linzer, M., S. Poplau, D. Khullar, R. Brown, A. Varkey, S. Yale, E. Grossman, E. Williams, and C. Sinsky. 2019. Characteristics of Health Care Organizations Associated With Clinician Trust: Results From the Healthy Work Place Study. JAMA Network Open 2(6):e196201. https://doi.org/10.1001/jamanetworkopen.2019.6201
- Agency for Healthcare Research and Quality. 2019. Medical Office Survey on Patient Safety Culture. Agency for Healthcare Research and Quality, Rockville, MD. Available at: https://www.ahrq.gov/sops/surveys/medical-office/index.html (accessed September 24, 2020).
- Sinsky, C. A., L. N. Dyrbye, C. P. West, D. Satele, M. Tutty, and T. D. Shanafelt. 2017. Professional Satisfaction and the Career Plans of US Physicians. Mayo Clinic Proceedings 92(11):1625-1635. https://doi.org/10.1016/j.mayocp.2017.08.017
- West, C. P., L. N. Dyrbye, and T. D. Shanafelt. 2018. Physician burnout: contributors, consequences and solutions. Journal of Internal Medicine 283(6):516-529. https://doi.org/10.1111/joim.12752
- Panagioti, M., E. Panagopoulou, P. Bower, G. Lewith, E. Kontopantelis, C. Chew-Graham, S. Dawson, H. van Marwijk, K. Geraghty, and A. Esmail. 2017. Controlled Interventions to Reduce Burnout in Physicians: A Systematic Review and Meta-analysis. JAMA Internal Medicine 177(2):195-205. https://doi.org/10.1001/jamainternmed.2016.7674
- Melnyk, B. M., S. A. Kelly, J. Stephens, K. Dhakal, C. McGovern, S. Tucker, J. Hoying, K. McRae, S. Ault, E. Spurlock, and S. B. Bird. 2020. Interventions to Improve Mental Health, Well-Being, Physical Health, and Lifestyle Behaviors in Physicians and Nurses: A Systematic Review. American Journal of Health Promotion. https://doi.org/10.1177/0890117120920451
- Sinsky, T. A., and C. A. Sinsky. 2012. A streamlined approach to prescription management. Family Practice Management 19(6):11-13. Available at: https://pubmed.ncbi.nlm.nih.gov/23317126/ (accessed October 13, 2020).
- Ashton, M. 2019. Getting Rid of Stupid Stuff: Reduce the Unnecessary Daily Burdens for Clinicians. AMA STEPS Forward. Available at: https://edhub.amaassn.org/steps-forward/module/2757858 (accessed May 27. 2020).
- Sinsky, C. A., P. Basch, and J. F. Fogg. 2018. Electronic Health Record Optimization: Strategies for Thriving; Strategies to help health care organizations maximize the benefits and minimize the burdens of the EHR. AMA STEPS Forward. Available at: https://edhub.ama-assn.org/steps-forward/module/2702761 (accessed May 27, 2020).
- Sieja, A., K. Markley, J. Pell, C. Gonzalez, B. Redig, P. Kneeland, and C. Lin. 2019. Optimization Sprints: Improving Clinician Satisfaction and Teamwork by Rapidly Reducing Electronic Health Record Burden. Mayo Clinic Proceedings 94(5):793-802. https://doi.org/10.1016/j.mayocp.2018.08.036
- Murphy, D. R., T. Satterly, T. D. Giardina, D. F. Sittig, and H. Singh. 2019. Practicing Clinicians’ Recommendations to Reduce Burden from the Electronic Health Record Inbox: a Mixed-Methods Study. Journal of General Internal Medicine 34(9):1825-1832. https://doi.org/10.1007/s11606-019-05112-5
- Jerzak, J., and C. Sinsky. 2017. EHR In-Basket Restructuring for Improved Efficiency: Efficiently manage your in-basket to provide better, more timely patient care. AMA STEPS Forward. Available at: https://edhub.ama-assn.org/steps-forward/module/2702694 (accessed May 27, 2020).
- Murphy, D. R., A. N. D. Meyer, E. Russo, D. F. Sittig, L. Wei, and H. Singh. 2016. The Burden of Inbox Notifications in Commercial Electronic Health Records. JAMA Internal Medicine 176(4):559-560. https://doi.org/10.1001/jamainternmed.2016.0209
- Murphy, D. R., B. Reis, D. F. Sittig, and H. Singh. 2012. Notifications received by primary care practitioners in electronic health records: a taxonomy and time analysis. American Journal of Medicine 125(2):209.e1-7. https://doi.org/10.1016/j.amjmed.2011.07.029
- AMA STEPS Forward. 2017. Restructuring EHR Inbaskets in Minneapolis—St. Paul, MN: A Case Study. AMA STEPS Forward. Available at: https://edhub.ama-assn.org/steps-forward/module/2702709 (accessed April 26, 2020).
- Resneck, J. S. 2020. Refocusing Medication Prior Authorization on Its Intended Purpose. JAMA 323(8):703-704. https://doi.org/10.1001/jama.2019.21428
- Carr, P. L., A. S. Ash, R. H. Friedman, A. Scaramucci, R. C. Barnett, L. Szalacha, A. Palepu, and M. A. Moskowitz. 1998. Relation of Family Responsibilities and Gender to the Productivity and Career Satisfaction of Medical Faculty. Annals of Internal Medicine. https://doi.org/10.7326/0003-4819-129-7-199810010-00004
- Funk, K. and M. Davis. 2015. Enhancing the Role of the Nurse in Primary Care: The RN “Co-Visit” Model. Journal of General Internal Medicine 30(12):1871-1873. https://doi.org/10.1007/s11606-015-3456-6
- Hopkins, K. and C. A. Sinsky. 2014. Team-based care: saving time and improving efficiency. Family Practice Management 21(6):23-29. Available at: https://pubmed.ncbi.nlm.nih.gov/25403048/ (accessed October 13, 2020).
- Lyon, C., A. F. English, and P. Chabot Smith. 2018. A Team-Based Care Model That Improves Job Satisfaction. Family Practice Management 25(2):6-11. Available at: https://pubmed.ncbi.nlm.nih.gov/29537246/ (accessed October 13, 2020).
- AMA STEPS Forward. 2019. Four Interventions Stemmed the Tide of Refill Requests. Available at: https://edhub.ama-assn.org/steps-forward/module/2757862 (accessed May 27, 2020).
- Shanafelt, T. D., and J. H. Noseworthy. 2020. Executive Leadership and Physician Well-being: Nine Organizational Strategies to Promote Engagement and Reduce Burnout. Mayo Clinic Proceedings 92(1):129-146. http://dx.doi.org/10.1016/j.mayocp.2016.10.004
- Perlo, J., B. Balik, S. Swensen, A. Kabcenell, J. Landsman, and D. Feeley. 2017. IHI Framework for Improving Joy in Work. IHI White Paper. Cambridge, Massachusetts: Institute for Healthcare Improvement. Available at: http://www.ihi.org/resources/Pages/IHIWhitePapers/Framework-Improving-Joy-in-Work.aspx (accessed September 24, 2020).
- Perlo, J., and B. Balik. 2017. “What Matters to You?” Conversation Guide for Improving Joy in Work. Institute for Healthcare Improvement. Boston, MA. Available at: http://www.ihi.org/resources/Pages/Tools/Joy-in-Work-What-Matters-to-You-Conversation-Guide.aspx (accessed September 24, 2020).
- Pepper, J. R., S. Jaggar, M. J. Mason, S. J. Finney, and M. Dusmet. 2012. Schwartz Rounds: reviving compassion in modern healthcare. Journal of the Royal Society of Medicine 105(3):94–95. https://doi.org/10.1258/jrsm.2011.110231
- Smith, C. D., C. Balatbat, S. Corbridge, A. Legreid Dopp, J. Fried, R. Harter, S. Landefeld, C. Y. Martin, F. Opelka, L. Sandy, L. Sato, and C. Sinsky. 2018. Implementing optimal team-based care to reduce clinician burnout. NAM Perspectives. Discussion Paper, National Academy of Medicine, Washington, DC. https://doi.org/10.31478/201809c