Optimizing Health Outcomes for Children with Asthma in Delaware: A Population Health Case Report
Background
The transformation of the U.S. health care delivery system is under way. As health care providers and community-based partners recognize the impact of the multifaceted determinants of health that extend beyond the clinical setting, there is an “opportunity for health care delivery systems, public health agencies, community-based organizations, and many other entities to work together to improve health outcomes in the communities they serve” (Stoto, 2013, p. 2).
The Center for Medicare and Medicaid Innovation’s Health Care Innovation Awards (HCIA) Round 1 funded 107 awardees to implement the most compelling new ideas to deliver improved care, better health, and lower costs to Medicare, Medicaid, and Children’s Health Insurance Program enrollees, particularly those with the highest health care needs. Among the awardees was the Nemours Children’s Health System’s Optimizing Health Outcomes (OHO) for Children with Asthma in Delaware project, which tests a multifaceted model that incorporates a focus on the upstream determinants of health.
Nemours Children’s Health System’s interest in HCIA grew out of a long-standing commitment to child health. In 2004, Nemours established an operational division called Nemours Health and Prevention Services to focus on preventing disease and promoting health, broadening the focus from the patient panel to the health of all of Delaware’s children. For a decade, the division has operated alongside Nemours’s flagship Nemours/Alfred I. duPont Hospital for Children and Nemours’s primary and specialty care practices in the Delaware Valley. To enhance integration of clinical care and community-based prevention, as well as to achieve a broader mission of helping children grow up healthy, in 2011 Nemours established a leadership work group to develop a strategy to optimize health for Delaware’s children. When the Innovation Center announced its competition for the first round of HCIA, the Nemours team identified an opportunity to further catalyze transformation.
Description of the Optimizing Health Outcomes for Children with Asthma in Delaware Initiative
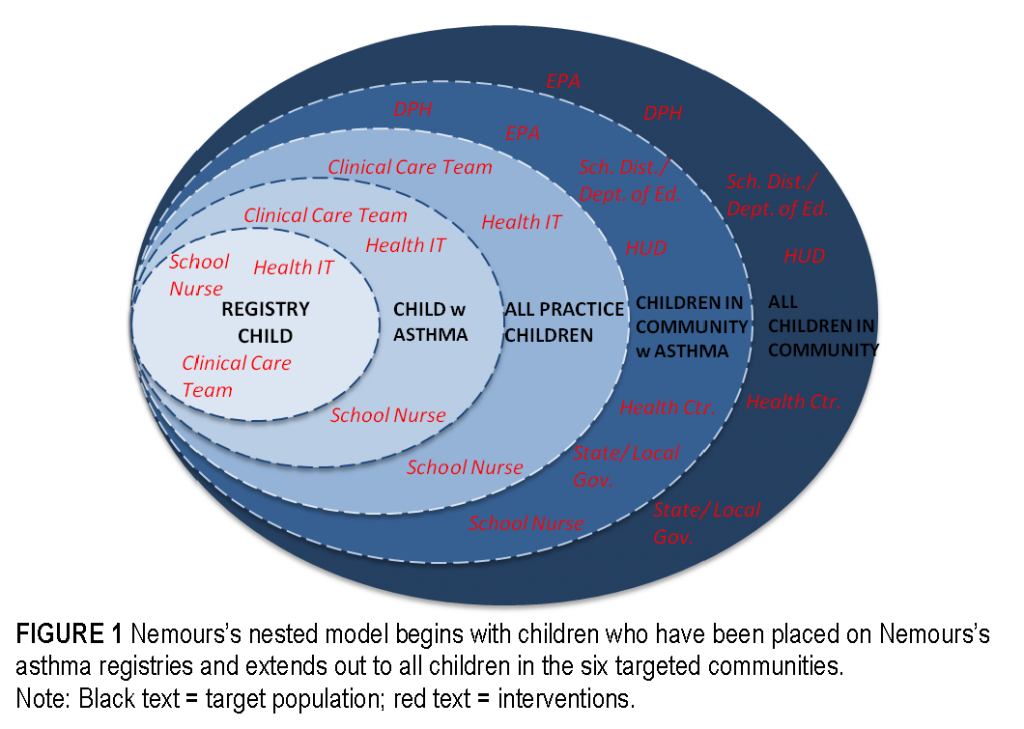
On July 1, 2012, as part of the Innovation Center’s HCIA Round 1, Nemours was awarded $3.7 million for a 3-year period to work with community partners in Delaware to better integrate clinical care with community-based prevention for children with asthma, including Medicaid beneficiaries. The target population comprises children with asthma receiving care in a family centered medical home at each of three Nemours primary care sites in Delaware, care that includes targeted clinical interventions for the more than 800 children enrolled in asthma registries. This nested model (see Figure 1) includes 42,000 children in six identified, associated communities who could be impacted by broader, community-based systems and changes in policy. The clinics are geographically diverse (urban and rural) and serve populations from a variety of racial and ethnic backgrounds.
The OHO project has four critical elements, or drivers: (1) enhancement of the existing family centered medical home; (2) use of technology to identify and stratify the patients at highest risk; (3) deployment of a “navigator” workforce (community health workers); and (4) development of an “integrator” model surrounding each site through community liaisons. The navigator and integrator models, along with the role of collaboration, are described in more detail as follows.
The Navigator Model
As part of the navigator model, community health workers (CHWs) work with children and families to identify triggers in patients’ homes and surrounding areas and coach families on how to eliminate or mitigate these triggers to avoid asthma attacks. CHWs also work with Nemours care coordinators and multisector partners to provide families with linkages to community and social services, such as housing, child care, and food, recognizing that these basic needs must be addressed in order to ultimately address underlying health issues. Through an innovative partnership with schools, school nurses have access to the Nemours electronic health record and asthma action plan for asthma registry patients, with parent permission. CHWs help to sign up patients to participate in this program.
The Integrator Model
The integrator’s work is fueled by the close bonds Nemours develops and maintains with other organizations from a variety of sectors, including public health, housing, child care, and other sectors that together can influence policy and systems changes in the places children live, learn, and play. Nemours employs community health liaisons to work at a systems level to identify and mitigate issues within the community, such as reducing bus idling that exacerbates asthma and reducing asthma triggers in public housing and in child care. The work of the community liaisons, which includes collaborating with community partners, is critical to improving population health within the context of community needs that go far beyond the walls of the health system.
Key Points of Collaboration
Collaboration within and across sectors is central to the model. Nemours has partnered with public health on big-picture strategy and implementation of the model. Regarding overarching strategy, Nemours has actively engaged in the clinical and community work streams of the State Innovation Model (SIM) and ensured that the Nemours Innovation Center award aligned with the Delaware SIM. Nemours also partnered with the Delaware Public Health Department on a convening to advance the role of CHWs in Delaware. Continued dialogue about including the CHW role occurs through the SIM work streams. In addition, Nemours engages with Medicaid to discuss lessons learned, including the importance of accessing data to assess impact and drive change. In implementing the Nemours Innovation Center award, the state public health department served as a critical partner. The health department linked Nemours with appropriate organizations to train CHWs prior to conducting home environmental assessments and referred Nemours to organizations that could address environmental remediation issues that CHWs uncovered during home visits. The health department also participated with Nemours and the U.S. Department of Housing and Urban Development in providing training on asthma trigger reduction in homes to landlords and residents of public housing. Nemours continues to partner with public health to assure healthy home environments for Delaware’s children.
One specific example of collaboration relates to the Delaware Medicaid formulary. On the basis of their direct contact with families during home visits, CHWs reported back to Nemours colleagues that families were having trouble tracking the number of doses of medicine left in quick-relief bronchodilators—the inhalers that patients with asthma rely on to open airway passages during a flare-up. Each inhaler has approximately 200 doses of medicine. Some inhalers have dose counters that track how many doses of active medication are left in the inhaler; however, the brand previously covered by Delaware Medicaid did not have the counters, leaving many families to guess how many doses were left. CHWs informed the Nemours asthma educator and policy team (acting as the integrator) about the difficulty families had in tracking doses. The policy team raised the issue to the chief of the Division of General Pediatrics at Nemours/Alfred I. duPont Hospital for Children, who subsequently testified before the Delaware Division of Medicaid and Medical Assistance Pharmacy and Therapeutics Committee, recommending that Delaware add a bronchodilator with a metered dose counter to its formulary of preferred drugs. Ultimately, the committee approved the addition to the formulary. Providers can now prescribe a bronchodilator inhaler with a dose counter to Medicaid beneficiaries, and Delaware Medicaid covers the cost. Critical information provided by the CHWs and linkages made by the integrator catalyzed a change that will benefit children across the state.
The underlying theory of change for this model is that by linking clinical interventions and community-based approaches, there will be improved outcomes at both the individual and population levels. The model also builds on the diffusion of innovation theory, which posits that an idea or product gains momentum and diffuses, or spreads, through a specific population or social system over time. It is expected that, over time, the changes made by the innovators and early adopters in the Nemours system will spread and scale throughout the Nemours health system and beyond.
Preliminary Findings
Nemours’s self-monitoring plan tracks approximately 50 measures to assess the impact of the intervention and includes process and outcome measures focused on improving health care, improving health outcomes, and reducing costs. The intervention utilized a pre-post cohort methodology to monitor and measure outcomes. The preliminary findings, which have not been verified by the independent evaluator, reflect an overall improvement in patient health, health care integration, and the quality of health care provided. Nemours is using the data captured in the self-monitoring plan to provide feedback to members of the clinical care teams; Nemours Informatics, which played a critical role in making adjustments to Nemours’s health information technology system to retrieve data; and executive level leadership for the Nemours Health System, including Delaware Valley senior leaders. The National Opinion Research Center (NORC) at the University of Chicago is conducting a formal evaluation of the intervention on behalf of the Innovation Center. The NORC evaluation is based on the analysis of Medicaid claims data for registry children who were enrolled in Medicaid at the start of the intervention. NORC conducted a pre-post comparison with a matched control group of children not on the asthma registry. Below, we outline preliminary findings under each dimension of the Triple Aim: better health, better health care, and lower cost.
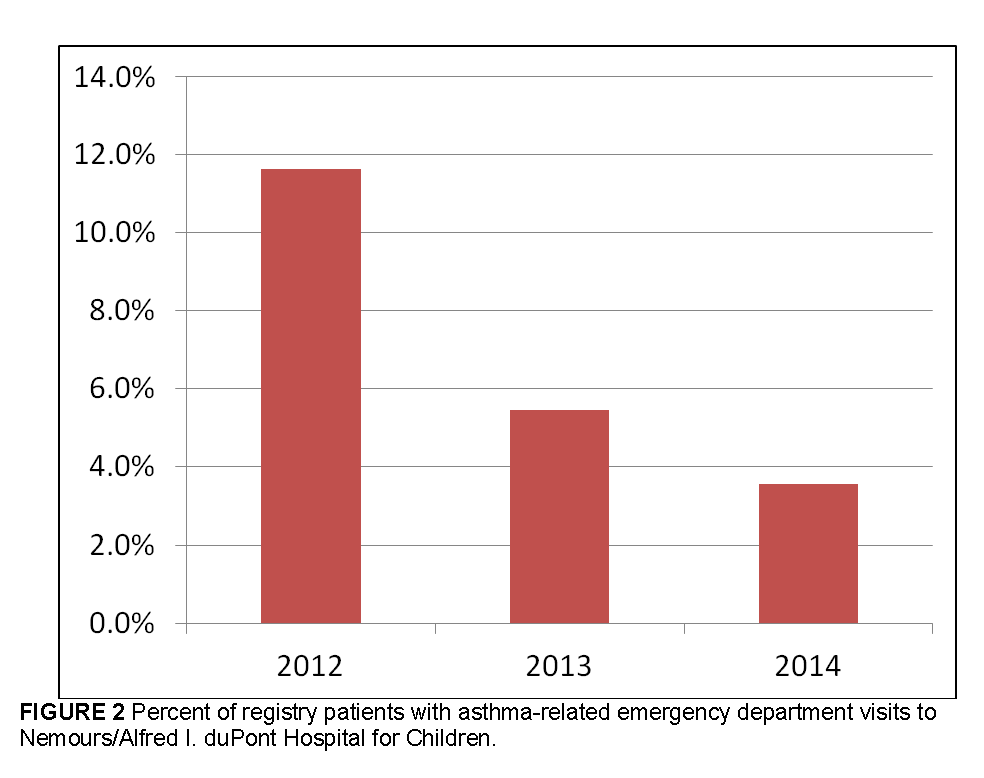
Better Health: Reduce Asthma-Related Emergency Department Visits
Preliminary self-monitoring findings indicate that the number of asthma-related emergency department (ED) visits for patients on the Nemours asthma registry has decreased considerably over the 3-year timeline of the award (see Figure 2). The cumulative number of asthma-related ED visits to Nemours/Alfred I. duPont Hospital for Children for registry patients shows a decrease of more than 40 percent from 2012 to 2013 and a decrease of more than 30 percent from 2013 to 2014, according to preliminary findings. There was an overall decrease from 2012 to 2014 of more than 60 percent, according to preliminary findings. Although the findings indicate improved asthma management for patients on the Nemours registry over time, we should note that asthma-related ED visits may not (and in some cases, should not) be completely eliminated. Nemours’ ED data is based on patient records, and was mined from the Nemours data warehouse. The NORC evaluation also found a reduction in ED visits. NORC observed 60 fewer children with ED visits per 1,000 for children on the Nemours asthma registry. It is important to note that NORC’s findings regarding ED utilization were based on all causes, and were not specific to asthma-related ED visits.
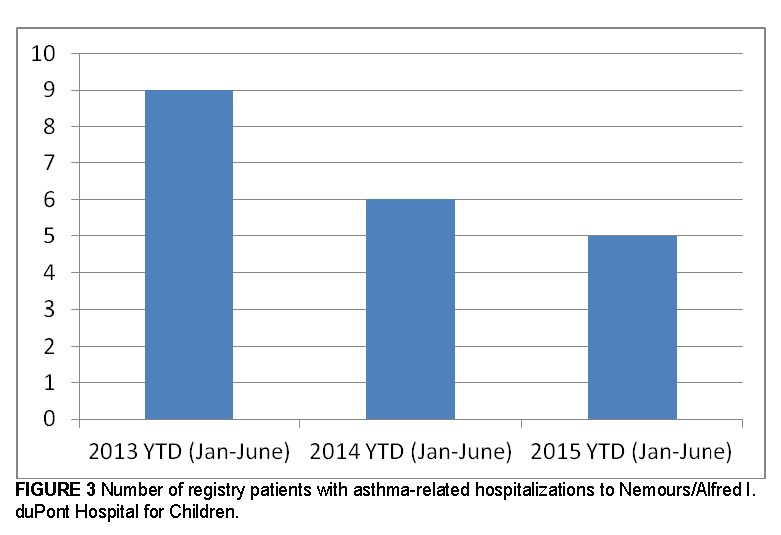
Better Health: Reduce Asthma Hospitalizations and Readmissions
Preliminary self-monitoring findings indicate that the total number of asthma-related hospitalizations at Nemours/Alfred I. duPont Hospital for Children has decreased for patients on the asthma registry (see Figure 3). Preliminary findings indicate that there were 44 percent fewer asthma hospitalizations at Nemours/Alfred I. duPont Hospital for Children in 2015 (January – June) than in 2013 (January – June). Nemours data is based on patient records, and was mined from the Nemours data warehouse. Nemours data does not reflect patients who have been hospitalized at facilities other than Nemours. Findings from NORC indicate that there were 13 fewer children with asthma related hospitalizations per 1,000 for children on the asthma registry, compared to children in a comparison group from the pre-intervention period to the post-intervention period. NORC’s findings showed a smaller change in the number of asthma-related hospitalizations, and the differences in findings between Nemours and NORC can likely be attributed to the differences in methodologies. However it is important to note that both sets of findings indicated a reduction in asthma-related hospitalizations.
Better Health Care: Increase Connection to Community Resources for Nonmedical Needs
The number of registry patients with a referral to a community resource increased considerably in the initial months following the launch of this component of the Nemours Innovation Center award (increasing from zero referrals in January–March 2013 to 19 referrals in January–March 2014). Data regarding referrals to community resources was obtained via a cohort review process, as it was determined that the existing EHR could not be queried for this data element. The CHWs used their records, as well as the EHR, to answer the questions posed in the cohort review. The initial increase may be attributed to the extensive needs of the children and families served by the award and the growing familiarity that CHWs had with the resources in their communities. In 2014, there was a decrease in the number of connections to community resources to 7 referrals in April–June 2014, indicating a decrease in the need for resources by patients on the registry. There may be a “saturation point” at which patients and families have been linked to the majority of nonclinical support needed. In addition, fewer new patients were added to the registry in later months.
Reduction of Costs: Overall Cost of Care for Medicaid-Covered Registry Patients
Training on the development of economic models (and modeling) and cost analyses has launched at Nemours under the direction of a health economist from the Thomas Jefferson University School of Pharmacy. Initial results and the fiscal implications of implementing the intervention are expected in late 2016. While Nemours’ cost-related findings are pending, NORC observed a significant reduction in cost in the amount of $533 per child per quarter for patients on the Nemours asthma registry relative to the patients in the comparison group.
Discussion
The Nemours OHO project has been a catalyst for positive change and deeper integration of clinical and community-based prevention activities in Delaware. A key element of this model is the focus on making changes at the individual level while simultaneously working at a systems level to address nonmedical factors influencing health. Following are lessons learned that may be relevant to future innovators.
Lesson 1: It is necessary to engage key clinical and community-based stakeholders upfront to facilitate practice transformation; the development of interdisciplinary teams, organizational culture change; and patient, family, and community engagement. To successfully link clinical care and community health, health care systems have to include team members who bring both a clinical perspective and a public health perspective to meet the needs of the child and family holistically. Nemours’s CHWs and community liaisons are integrated into the care teams at the three participating primary care practices. This integration of nonclinical team members who have a deep understanding of the larger community context did not occur immediately and was initially met with some resistance. However, embedding community liaisons within the primary care practices is critical. Future innovators should consider how to optimize collaboration and engagement of critical clinical, public health, and community stakeholders upfront.
Lesson 2: To sustain what works, begin sustainability planning early and pursue multiple pathways. Determining how to sustain an initiative after award funds end can be challenging. Early on, even as the model is being developed and implemented, it is important to identify and engage partners (including payers) who may be critical to sustaining the most effective elements of the project in the long run. This planning should include determining a method for establishing which project elements should be sustained, assessing how frequently to make adjustments in the model, and working with partners to sustain the critical elements.
Nemours is pursuing multiple sustainability pathways. These pathways include the following: (1) utilizing our own funding to sustain critical roles, such as hiring psychologists and care coordinators for each primary care practice and continuing to fund community liaisons; (2) working closely with community partners who, moving forward, can take a leadership role in policy and systems change; the establishment of community leadership teams and community action plans helped promote sustainable relationships and partnerships that will live on beyond the end of the award; (3) engaging with the State of Delaware regarding the SIM planning process, including sharing information regarding our lessons learned; and (4) exploring early discussions with a private payer regarding a potential payment pilot. Including an intentional focus on sustainability planning is critical.
The OHO project and other innovative projects focusing on the three-part aim (The equivalent of the Triple Aim concept of better care, better health, at lower cost (Berwick et al., 2008) have significant potential to accelerate the rate of transformation of the U.S. health care delivery system. Integration of clinical and population-based prevention and a greater awareness of how one’s community environment influences health can, and should, become part and parcel of the way health care is provided in the United States. A transformed health system will encompass true partnerships among providers, payers, community partners, patients, and families, creating a realignment to ensure that they are working toward the Triple Aim.
Note: The project described was supported by Grant Number 1C1CMS331017 from the U.S. Department of Health and Human Services (HHS), Centers for Medicare & Medicaid Services (CMS), to Nemours. The contents of this publication are solely the responsibility of the authors and do not necessarily represent the official views of HHS or any of its agencies. Research findings presented reflect both awardee self-monitoring data and findings of the independent evaluation contractor. Awardee findings and analysis have not been confirmed by the independent evaluation contractor and do not represent the views of CMS.
Download the graphic below and share it on social media!
References
- Berwick, D. M, T. W. Nolan, and J. Whittington. 2008. The Triple Aim: Care, health, and cost. Health Affairs 27(3):759–769. Available at: http://content.healthaffairs.org/content/27/3/759.abstract (accessed March 1, 2016).
- Boston University School of Public Health. 2013. Diffusion of innovation theory. Available at: http://sphweb.bumc.bu.edu/otlt/MPH-Modules/SB/SB721-Models/SB721-Models4.html (accessed March 1, 2016).
- Centers for Medicare & Medicaid Services. Health Care Innovation Awards. Available at: http://innovation.cms.gov/initiatives/Health-Care-Innovation-Awards (accessed March 1, 2016).
- NORC Second Annual Report: HCIA Disease-Specific Evaluation. 2016. Bethesda: NORC at the University of Chicago. Available at: http://downloads.cms.gov/files/cmmi/hcia-diseasespecificsecondevalrpt.pdf (accessed May 17, 2016).
- Stoto, M. A. 2013. Population health in the Affordable Care Act era: AcademyHealth brief. Washington, DC: AcademyHealth. Available at: http://www.academyhealth.org/files/AH2013pophealth.pdf (accessed March 1, 2016).