Browse all health-related publications released by the National Academies in April 2017 below. To receive updates from the NAM, please subscribe to our mailing list.
Reports document the evidence-based consensus of an authoring committee of experts. Proceedings chronicle the presentations and discussions at a workshop, symposium, or other convening event. Perspectives are individually-authored expert commentaries and discussion papers from leading voices in health and health care.
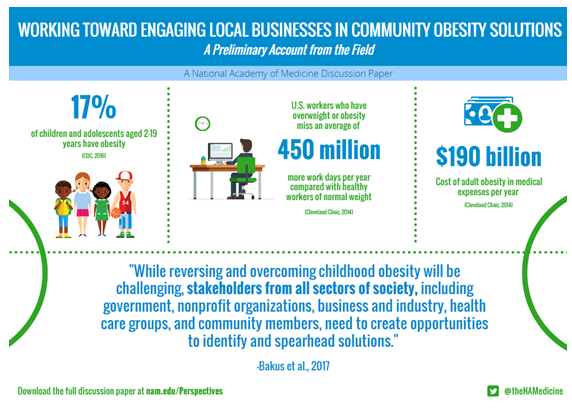
Working Toward Engaging Local Businesses in Community Obesity Solutions
April 3, 2017 | NAM Perspective
Childhood obesity continues to be a serious public health concern in the United States. About 12.7 million children and adolescents aged 2–19 years, or 17 percent of the population, have obesity. In addition to genetic and behavioral factors, the environments where children live, learn, and play impact their health and well-being. A lack of access to affordable, healthy foods; the absence of physical activity in schools and childcare centers; and a shortage of safe community spaces such as parks, sidewalks, and bike paths also contribute to obesity levels. While reversing and overcoming childhood obesity will be challenging, stakeholders from all sectors of society, including government, nonprofit organizations, business and industry, health care groups, and community members, need to create opportunities to identify and spearhead solutions.
Future Financial Economics of Health Professional Education
April 5, 2017 | NASEM Proceedings of a Workshop
The Government Accountability Office (GAO), World Health Organization (WHO), and the World Bank all agree that “an adequate, well-trained, and diverse health [care] workforce is essential for providing access to quality health [care] services.” However, according to the World Bank, efforts to scale up the supply of health workers are falling short. The resulting health workforce shortage affects people’s access to quality health care around the globe, and can result in untreated sickness, disability, and adverse economic consequences.Matching population health needs with the right number, mix, distribution, and skill set of health workers while considering how supply and demand drive decisions within education and health was the topic of a workshop hosted by the Global Forum on Innovation in Health Professional Education on October 6-7, 2016.
Integrating Clinical Research into Epidemic Response: The Ebola Experience
April 12, 2017 | NASEM Report
The 2014 Ebola epidemic in western Africa was the longest and deadliest Ebola outbreak in history, resulting in 28,616 cases and 11,310 deaths. In the midst of the rapidly spreading, highly dangerous contagious disease—with no Ebola-specific vaccines or therapeutics available to help curb the epidemic—the international community implemented clinical trials on investigational agents, not yet studied in humans for safety or efficacy. Within that context, the Office of the Assistant Secretary for Preparedness and Response, the National Institute of Allergy and Infectious Disease, and the U.S. Food and Drug Administration, supported the National Academies of Sciences, Engineering, and Medicine to convene a committee to analyze the clinical trials that were conducted during the epidemic and consider the many scientific, ethical and practical issues related to the conduct of research in similar contexts.
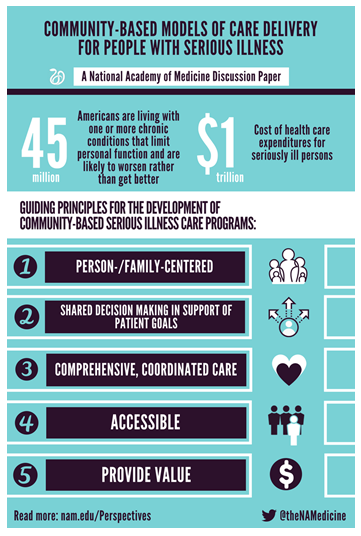
Community-Based Models of Care Delivery for People with Serious Illness
April 13, 2017 | NAM Perspective
The 20th century saw remarkable improvements in life expectancy. Improvements in access to clean water, disease screening and prevention, the discovery of antibiotics and vaccines, development of organ transplantation, and advances in treatment for heart disease and cancer have all contributed to an expectation that Americans will live long lives in generally good health. A concomitant change has been that most Americans will now experience a substantial period of living with serious illness, mostly progressive and life-limiting. An estimated 45 million Americans are living with one or more chronic conditions that limit personal function and are likely to worsen rather than get better. Although representing only 14 percent of the population, these seriously ill persons account for 56 percent of all health care expenditures—almost $1 trillion.
Building Health Literacy and Family Engagement in Head Start Communities: A Case Study
April 14, 2017 | NAM Perspective
Policy makers, government agencies, and community organizations seeking to improve health outcomes in vulnerable populations are paying increased attention to family engagement and health literacy as key elements of a population health approach. To capitalize on the promise of prevention and create a culture of health, families need a supportive environment that enables them to make informed health decisions and lifestyle choices. Low health literacy is associated with poor health outcomes and is considered a social determinant of health. To create a culture of health, families with young children need to be engaged as partners and advocates for their children. Family engagement is critical not only to maximizing a child’s academic success but also to fostering positive health outcomes. To accomplish this, sustainable health literacy and family engagement strategies need to be integrated into the core of organizations working to improve health.
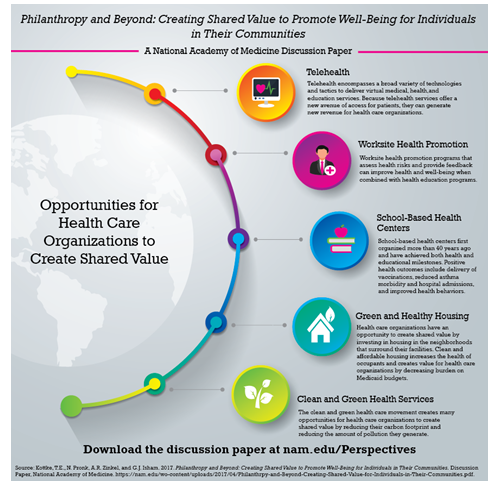
Philanthropy and Beyond: Creating Shared Value to Promote Well-Being for Individuals in Their Communities
April 21, 2017 | NAM Perspective
Health care organizations can magnify the impact of their community service and other philanthropic activities by implementing programs that create shared value. By definition, shared value is created when an initiative generates benefit for the sponsoring organization while also generating societal and community benefit. Because the programs generate benefit for the sponsoring organizations, the magnitude of any particular initiative is limited only by the market for the benefit and not the resources that are available for philanthropy.
In this article we use three initiatives in sectors other than health care to illustrate the concept of shared value. We also present examples of five types of shared value programs that are sponsored by health care organizations: telehealth, worksite health promotion, school-based health centers, green and healthy housing, and clean and green health services.
Case Study: Improving Population and Individual Health Through Health System Transformation in Washington State
April 24, 2017 | NAM Perspective
Empowered by federal, state, and community funding, Washington State has been working for years to enact delivery system transformation to improve the health and well-being of its 7 million residents. In fact, in the 1990s Washington State passed legislation offering universal coverage for its residents. But when the individual mandate was repealed just a year after implementation, insurance premiums spiked, and many plans left the state. Then-governor Chris Gregoire shared her state’s lessons with President Barack Obama during his presidential campaign, advising that universal coverage without an individual mandate is a recipe for failure. When the Affordable Care Act (ACA) was signed into law in 2010 with an individual mandate, Washington was already well poised for implementation, having attempted, and learned from, its previous universal coverage experiment.
Case Study: Medicaid and Public Health Collaboration in Oregon
April 24, 2017 | NAM Perspective
Oregon is one of the leading states engaged in innovative health care delivery system reform that includes population health as a central component. Collaboration among key agencies and stakeholders is an important feature of Oregon’s reform efforts, and it occurs at many levels. This case study will highlight the state’s efforts to link the Medicaid delivery system and public health system to support prevention initiatives. Oregon’s experience may be helpful to other states as they consider reforms under Medicaid to advance population health and other prevention strategies.

Case Study: Nationwide Children’s Hospital: An Accountable Care Organization Going Upstream to Address Population Health
April 24, 2017 | NAM Perspective
As managed care organizations (MCOs) and accountable care organizations (ACOs) begin to invest in population health improvement, they are faced with significant and diverse challenges. This is especially true in pediatric care; without the leverage of a national payment system and standard-setting authority like Medicare, those providing and paying for pediatric care must navigate complex political, cultural, and financial environments that are unique to each state and local community. Though many MCOs and ACOs already engage in population health and prevention work, not all invest in upstream interventions that address the root social determinants of health. These social determinants of health contribute to long-term wellness—or sickness—and play a large role in chronic disease development. A key question remains: what are the factors that influence leadership in MCOs and ACOs to move upstream and invest in the social determinants of health?
