Moral Distress and Moral Strength Among Clinicians in Health Care Systems: A Call for Research
Every day in clinical practice, health care clinicians make difficult decisions about appropriate treatment and care for their patients. Years of training prepare them for this responsibility, to choose the best course of action for a patient based on their clinical knowledge, the patient’s needs and wants, and the clinician’s professional and human values. Such daily decisions may be emotionally laden and are often made in challenging circumstances. There may be pressure from patients and families, burden from chronic understaff – ing, complicated organizational structures and hierarchies, system inefficiencies that shift attention away from patients, insurance or institutional policies that limit options, differences of opinion about appropriate care, and breakdowns in communication with interprofessional colleagues and administrators. These choices are often complex, and the best course of action may not be clear.
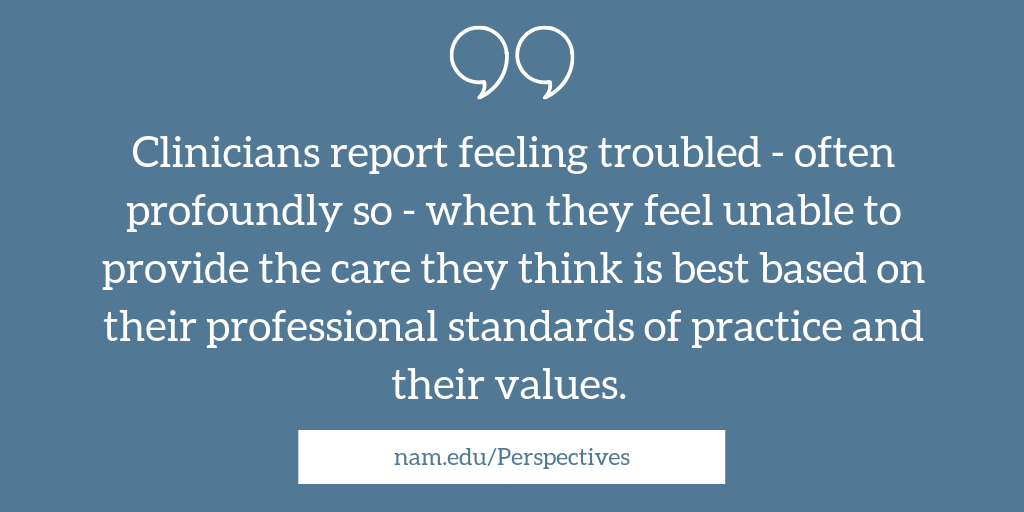
In some cases, clinicians find themselves taking part in a course of action—such as providing or withholding treatment—with which they do not fully agree and may even think is wrong. In such situations, clinicians can experience what has been called “moral distress,” the negative feeling that follows when clinicians believe they know the morally best action to take, but a different action is taken, often for a variety of reasons [1]. A phenomenon researched particularly among nurses, moral distress is reported by many health professional groups in the current health care environment [1]. Clinicians report feeling troubled—often profoundly so—when they feel unable to provide the care they think is best based on their professional standards of practice and their values. These morally distressing situations can leave clinicians susceptible to emotional and physical symptoms, including powerlessness and fatigue, depression, suicidal behaviors, burnout, and posttraumatic stress [1].
Moving Beyond Moral Distress
Much of the dialogue on clinician well-being recognizes increasing levels of burnout and has led to a renewed interest in the concept of resilience and building individual coping skills to help support well-being. The authors of this Commentary agree that such a focus is necessary and likely to be beneficial. However, placing the burden on individual clinicians to develop better coping skills and greater resilience while failing to address important organizational and systemic factors will do little to reduce burnout or increase well-being.
More attention must be paid to the connections between the type and frequency of ethical issues in health care practice, the emotional intensity and cognitive complexity of these issues, constraints on providers, and the resulting moral distress. Importantly, an understanding of moral distress can be a lens through which researchers view the myriad ways clinicians perceive and act on ethical challenges in their daily practices.
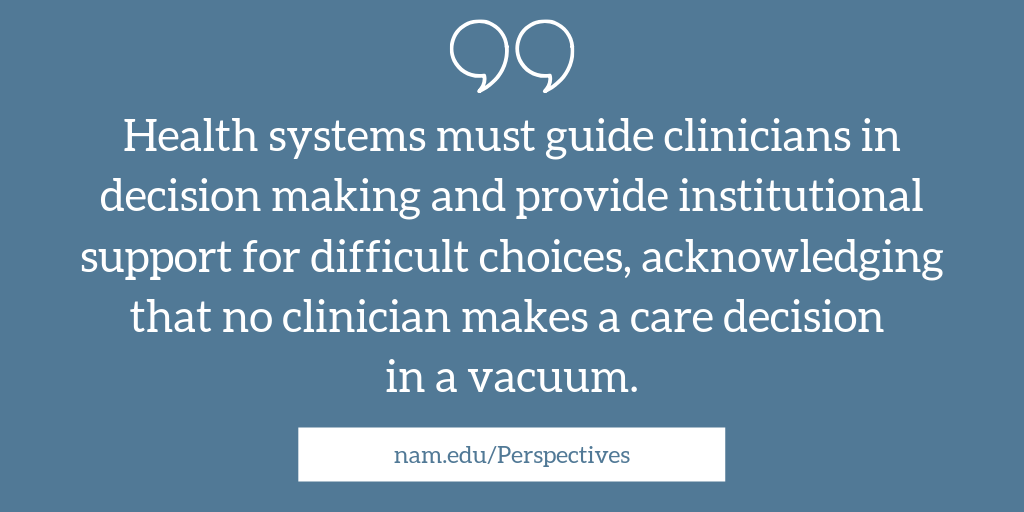
Identifying individual and institutional training needs and introducing system reforms could help to mitigate moral distress. Health systems must guide clinicians in decision making and provide institutional support for difficult choices, acknowledging that, in today’s systems, no individual clinician makes a care decision alone or in a vacuum.
Training and experience can often give clinicians the confidence, moral clarity, and self-efficacy to make difficult decisions without feelings of moral distress—a characteristic we call “moral strength.” But even clinicians who regularly demonstrate moral strength encounter situations that can engender moral distress.
Hannah and Avolio write that feeling a responsibility to act ethically, along with a sense of confidence and courage that one can enact the desired ethical behavior, provides an individual with the moral strength to act ethically despite challenges and perceived adverse consequences [2]. Health systems must find ways to foster clinicians’ moral strength.
Hamric, Arras, and Mohrmann caution, however, that courage should not be necessary for a clinician to ask questions or make suggestions regarding a patient’s care, and if one must evoke such inner strength on a routine basis to advocate for patients, there is a system-wide problem [3]. They note, “Courage is the virtue of approaching realistic fears or threats with appropriate confidence” [3].
The authors of this Commentary believe that the erosion of a clinician’s hard-earned clinical and moral confidence about difficult decisions (moral strength) usually comes from a lack of institutional support and that it is imperative for systems to change, as outlined below.
Research, Education, and Institutional Change
Evidence shows that dissatisfaction and wanting to leave one’s job—and the profession altogether—often follow morally distressing encounters [4]. Ethics education that builds cognitive and communication skills, teaches clinicians ethical concepts, and helps them gain communication skills and confidence may be essential in building moral strength. One study found, for example, that among practicing nurses and social workers, those with the least ethics education were also the least confident, the least likely to use ethics resources (if available), and the least likely to act on their ethical concerns. In this national study, as many as 23 percent of nurses reported having had no ethics education at all [5]. But the question remains—is ethics education enough?
Many factors likely support or hinder a clinician’s capacity and willingness to act with moral strength. More research is needed to investigate how interdisciplinary ethics education and institutional resources can help nurses, physicians, and others voice their ethical concerns, help them agree on morally acceptable actions, and support their capacity and propensity to act with moral strength and confidence. Research on moral distress and ethical concerns in everyday clinical practice can begin to build a knowledge base that will inform clinical training—in both educational and health care institutions—and that will help create organizational structures and processes to prepare and support clinicians to encounter potentially distressing situations with moral strength. Research can help tease out what is important and predictive for taking (or not taking) ethical action in morally distressing circumstances. This knowledge would be useful for designing strategies to support clinician well-being. Indeed, studies should focus on the influences that affect clinicians’ ability and willingness to become involved or take ownership of ethically-laden patient care issues, and their level of confidence in doing so.
Strategies, training, and institutional support are needed to reinforce clinicians’ engagement in morally complex situations and their sense of what is morally right. These components are also necessary to bolster clinicians’ confidence in their ability to work around unavoidable constraints and perform as their knowledge and values suggest [2].
Further, there is a need to identify effective interventions and strategies to prevent the experience of moral distress from leading to self-doubt and to the erosion of moral strength. Such interventions would advance organizational and systemic supports to bolster clinicians’ ability to handle stressors in a more nuanced and positive way.
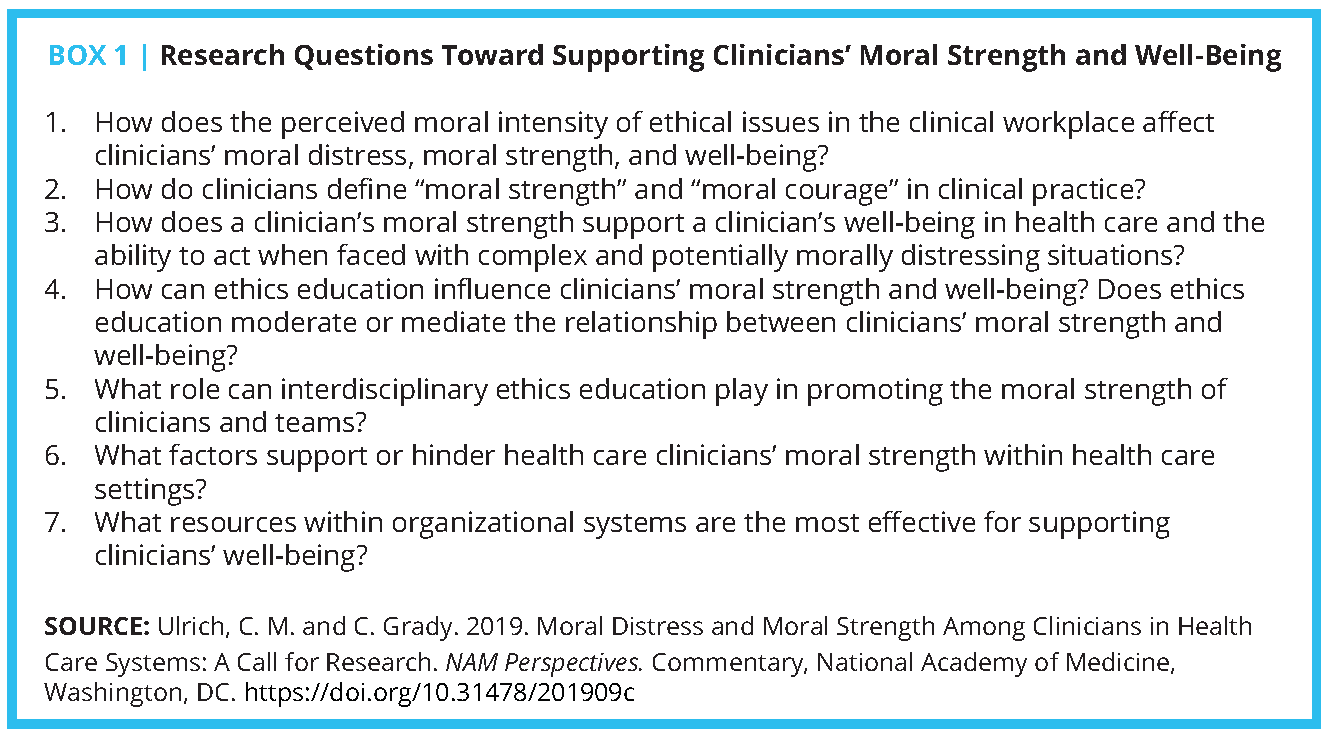
Moral distress may be inevitable in the multifaceted and ethically complicated arena of meeting the health care needs and preferences of diverse patients, but such distress need not inevitably lead to negative outcomes. The authors of this Commentary propose focusing on the following areas for future dialogue, research, and interventions: 1) identifying factors that support or hinder clinicians’ moral strength and ability to act in health care organizations; 2) advancing ethics education, with a focus on enhancing moral strength and confidence; and 3) identifying and changing organizational and systemic factors that result in clinicians’ moral distress and bolstering those that foster moral strength (see Box 1).
Conclusion
The authors of this Commentary have argued previously that the peril of having fewer or less-engaged health care clinicians as a result of moral distress will negatively affect patient care [1]. Society should be alarmed at the loss of clinicians to moral distress, burnout, and other emotional struggles, and be proactive. Prioritizing the efforts of health care leadership, educational bodies, and other stakeholders toward finding solutions that support moral strength and overall well-being for those working within health care systems requires empirical work on the increasing ethical complexities within these institutions.
If we do nothing to mitigate the stress, moral distress, and emotional damage endured by health care clinicians, we fail to honor the skills and expertise they bring to patients and families, their roles in society advocating for the public’s health, and, importantly, their humanity and vulnerability to the internal and external stressors that surface in addressing ethical challenges within their workplaces.
Join the conversation!
![]() Tweet this! Health care professionals regularly face complex ethical challenges and are not always able to make choices that they feel are correct. Read a new #NAMPerspectives about finding solutions to support clinicians’ moral strength: https://doi.org/10.31478/201909c
Tweet this! Health care professionals regularly face complex ethical challenges and are not always able to make choices that they feel are correct. Read a new #NAMPerspectives about finding solutions to support clinicians’ moral strength: https://doi.org/10.31478/201909c
![]() Tweet this! A new #NAMPerspectives Commentary calls for more research on how individual health care providers perceive and act on ethical challenges in their practice, and on the impact of moral distress on clinicians. Read it here: https://doi.org/10.31478/201909c
Tweet this! A new #NAMPerspectives Commentary calls for more research on how individual health care providers perceive and act on ethical challenges in their practice, and on the impact of moral distress on clinicians. Read it here: https://doi.org/10.31478/201909c
![]() Tweet this! Organizational and systemic factors can help to mitigate the moral distress that can result from ethical challenges faced in practice, but more research is needed. Learn more in this #NAMPerspectives Commentary: https://doi.org/10.31478/201909c
Tweet this! Organizational and systemic factors can help to mitigate the moral distress that can result from ethical challenges faced in practice, but more research is needed. Learn more in this #NAMPerspectives Commentary: https://doi.org/10.31478/201909c
Download the graphics below and share them on social media!
References
- Ulrich, C., and C. Grady. 2018. Moral distress in the health professions. New York: Springer.
- Hannah, S. T., and B. J. Avolio. 2010. Moral potency: Building the capacity for character-based leadership. Consulting Psychology Journal Practice and Research 62(4):291-310. https://doi.org/10.1037/a0022283
- Hamric, A. B., J. D. Arras, and M. E. Mohrmann. 2015. Must we be courageous? Hastings Center Report 45(3):33-40. https://doi.org/10.1002/hast.449
- Whitehead, P. B., R. K. Herbertson, A. B. Hamric, E. G. Epstein, and J. M. Fisher. 2014. Moral distress among healthcare professionals: Report of an institution-wide survey. Journal of Nursing Scholarship 47:117-125. https://doi.org/10.1111/jnu.12115
- Grady, C., M. Danis, K. L. Soeken, P. O’Donnell, C. Taylor, A. Farrar, and C. Ulrich. 2008. Does ethics education influence the moral action of practicing nurses and social workers? The American Journal of Bioethics 8(4):4-11. https://doi.org/10.1080/15265160802166017