Lessons Learned for Obesity Prevention and Care from Five Integrated Programs

Abstract
Since the publication of our integrated framework for the prevention and treatment of obesity and related chronic diseases in 2015, more than 140 Accountable Communities for Health (ACH) have been established in an effort to develop multi-sectoral partnerships to improve the health of people and their communities. All of these ACH represent potential models of integrated programs. A 2020 summit held by the Integrated Clinical and Social Systems for the Prevention and Management of Obesity Innovation Collaborative at the National Academies of Sciences, Engineering, and Medicine reviewed five case studies of such integrated programs and discussed their relevance for obesity programs. Among the five models of integration discussed, there was no consistent conceptual framework; a variety of heterogeneous factors contributed to the design of these models, including cost, self-interest, and contractual limitations. The extent to which the models mirrored the elements of the collaborative’s 2015 framework was highly variable and context-dependent. Although none of the models discussed explicitly focused on obesity, they offer insights into the adoption of integrated health and health care systems more broadly and identify some gaps and challenges that should be considered for obesity-focused integrated programs.
Introduction
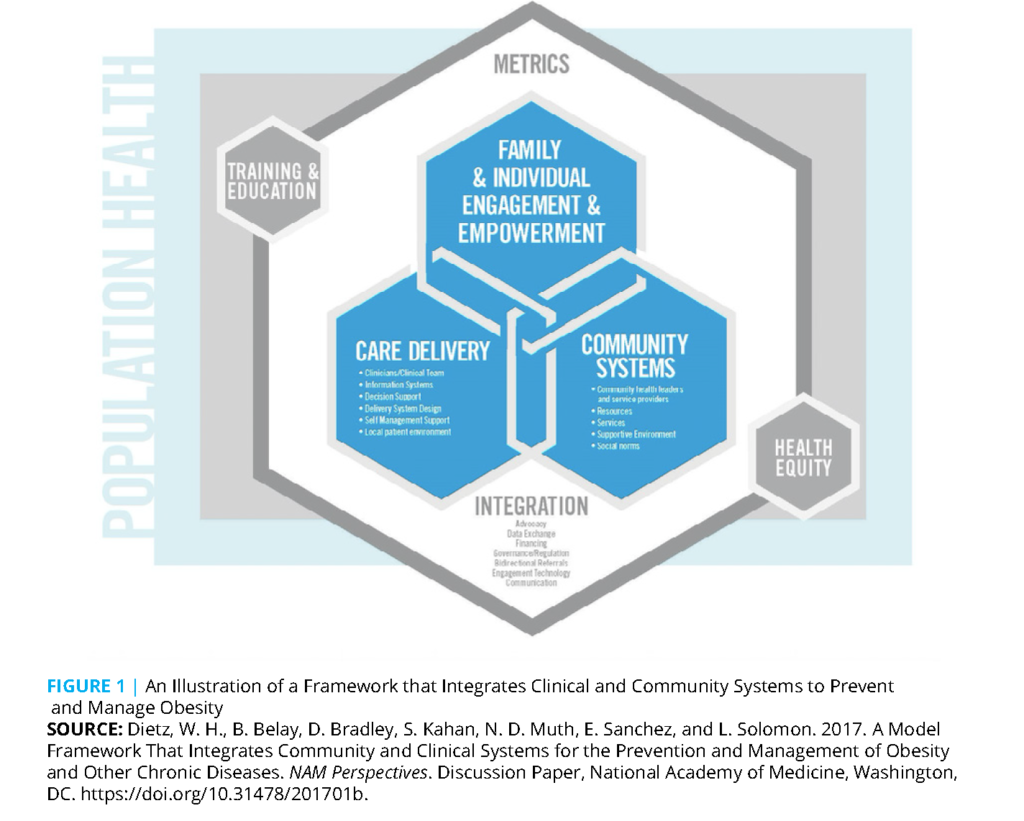
In 2015, several of the authors of this paper published an article in Health Affairs titled “An Integrated Framework for the Prevention and Treatment of Obesity and its Related Chronic Diseases” (Dietz et al., 2015). The article presented the third iteration of the Chronic Care Model (see Figure 1). The original Chronic Care Model focused on the integration and coordination of health care services to improve clinical outcomes in the care of chronic diseases (Kaiser Permanente Washington Health Research Institute, 2021). This model was subsequently revised to address obesity through changes in the care delivery system augmented by supportive changes in the physical environment (Dietz et al., 2007). The third iteration of the model, presented in the 2015 Health Affairs publication expanded on the elements necessary to integrate clinical and community services to prevent and treat obesity. Key elements included a trusted convener, a mechanism for bidirectional data exchange between the community organization and the clinical care delivery system; increased financing; improved governance; referral processes; and metrics to assess success.
In 2015, the concept of integrated clinical and community services was novel. Although the Health Affairs paper provided several examples of partially integrated systems, we were unable to identify any completely integrated systems that existed at the time. Since then, however, more than 140 Accountable Communities for Health (ACH) have been established that seek to develop multi-sectoral partnerships to improve the health of people and their communities (Mt. Auburn Associates, 2020). As a follow up to the 2015 publication, prior to the COVID-19 outbreak in 2020, the Integrated Clinical and Social Systems for the Prevention and Management of Obesity (ICSSPMO) Innovation Collaborative (an ad hoc activity affiliated with the Roundtable on Obesity Solutions at the National Academies of Sciences, Engineering, and Medicine) sponsored a summit (the Integration Summit) to explore progress in the development of integrated systems, and how such systems could better address the prevention and management of obesity. The issues discussed included:
- How to address obesity and the path forward for integrated clinical and community systems;
- How new models of “integrated obesity-related services” might modify the collaborative’s 2015 framework; and
- Model programs that integrated health care systems and the health of the public.
The Integration Summit considered five distinct programs, and the discussion that followed provided insights into how the framework proposed in our 2015 article could be modified. The summit made a deliberate attempt to capture thoughts, insights, and learnings regarding equity, value, power, and relationships in an effort to inform a revised framework. The five programs examined were:
- An integrated payer and care delivery system (Kaiser Permanente);
- A hospital-community partnership (Nationwide Children’s Hospital);
- Two plan-driven systems (Nemours Children’s Health System and AmeriHealth Caritas DC); and
- A community health plan partnership (Collaborative Cottage Grove in Greensboro, NC).
The authors of this paper recognize that these five programs are a diverse but limited sample. As a result, the models of integration that they represent offer no consistent conceptual framework. The factors that contributed to the design of these models were heterogeneous, and included cost, self-interest, and contractual limitations. In addition, the extent to which these models mirrored the elements of the 2015 framework also turned out to be highly variable and context-dependent. Still, the examples of these integrated programs provide valuable lessons as described in the following section.
Examples from the Field
Kaiser Permanente
Kaiser Permanente’s (KP) efforts to develop an integrated model for addressing the social determinants of health (SDoH) emerged from a 2019 survey of KP patients, which disclosed that 97% of respondents wanted medical providers to ask about their social needs. Throughout this manuscript, the term SDoH refers to the environmental conditions that affect a wide range of health functioning and quality of life outcomes and risks (ODPHP, 2021). To respond to this identified need, KP launched the “Thrive Local” initiative (https://permanente.org/tag/thrive-local/), which forms the core of the organization’s solution to addressing SDoH. Prior to this initiative, KP had undertaken more than 35 relatively unconnected programs to address the impact of SDoH.
KP is currently focusing on developing the infrastructure necessary to connect individuals with identified social needs to appropriate service providers through a network of community-based organizations, health care providers, and public agencies. The data produced at the individual, community, and organizational levels will allow KP to understand members’ and nonmembers’ social contexts and foster better partnerships with multi-sectoral community organizations.
This networked approach could theoretically identify gaps specific to obesity. For example, at the community level, it could provide data to multi-partner and multisectoral organizations that identify common assets and gaps. In addition, the approach could be applied to directly address issues of food insecurity, diabetes, and obesity.
The Thrive Local network features three components to provide integrated clinical and social care, supported by data integration and partnerships within the community:
- An online resource directory of social services within KP’s geographic footprint that can be filtered by geography, domain, service, and language spoken by the service provider;
- A community network tracking system that allows a community’s social service providers to share amongst themselves (with consent) information about individuals who use their services; and
- A technology platform that seamlessly integrates the data from a community network with KP’s electronic health records and other systems in a bidirectional information exchange.
Of the model programs presented at the summit, Kaiser Permanente’s example, which aggregates person-centered data to identify community needs, provides, in the opinions of the authors, the most innovative use of data to identify potential areas for partnerships that integrate health and health care partnerships. It remains unclear, however, how much community engagement will occur in the program’s design and implementation. It is also important to note that, to the authors, while KP’s Thrive Local program offers an interesting example of integration, it appears to address the consequences of SDoH rather than the determinants of SDoH.
Nationwide Children’s Hospital
Beginning in 2002, Nationwide Children’s Hospital (Nationwide) in Columbus, Ohio became a partner in a citywide effort to help Columbus flourish. The hospital is a large employer located next to an interstate highway and surrounded by a neighborhood with the highest rate of gun violence in the city, the third worst school in the state, and a 30% housing vacancy rate. The hospital’s decision to invest in its surrounding community was driven by its leadership’s conclusion that Nationwide could not claim to be a great health care system when “the situation next door is terrible.” In 2008, in partnership with United Way, city government, Ohio State University, a local church, and the non-profit Community Development for All People, the hospital initiated the “Healthy Neighborhoods Healthy Families” program, which targeted five areas:
1. Affordable housing;
2. Workforce development;
3. Education interventions;
4. Safe and accessible neighborhoods; and
5. Health and wellness.
The hospital established collateral funding that attracted additional investments to renovate and sell vacant and abandoned properties, provide homebuyer assistance, and provide existing homeowners with funds for home repair. These efforts have built over 370 homes and developed 55 rental units. Neighborhood vacancy rates have decreased by 70%, and limited data suggest that new homes have not gentrified the community. The expansion of hospital services has led to efforts to train and employ neighborhood residents, thereby reducing unemployment and poverty through the provision of local jobs. Eventual outcomes include school readiness and the elimination of racial disparities in infant mortality. Obesity has also been a target, and Nationwide has expanded beyond a bariatric surgery program to also include weight management programs in primary care and the provision of school-based services. Nationwide recognizes the connection of obesity to poverty and the need for broad-ranging interventions, and has begun to examine outcomes in the neighborhoods they have revitalized.
Although the Nationwide model blurs care delivery and community systems, it most directly addresses SDoH through health resources, political suasion of government agencies/donors, and capital investment. The authors believe this example is potentially scalable for health systems like Accountable Care Organizations.
Nemours Children’s Health System
Nemours Children’s Health System (Nemours) is a dominant player in Delaware serving child health. Based on a community needs assessment, Nemours initially targeted community concerns about obesity with efforts to shift its focus from the clinical care of individuals to the greater provision of community and population health. However, a 2012 grant from the Centers for Medicare and Medicaid Innovation provided the opportunity to develop an integrated approach to specifically prevent and reduce childhood asthma. This intervention started with efforts to educate clinicians in SDoH as they applied to asthma, for example, by organizing drive-by neighborhood tours. An asthma registry provided risk stratification. Patient navigators hired by Nemours provided the link between families and primary care clinics, conducted home environmental assessments, and reinforced asthma education. Nemours acted as the integrator, linking clinics to communities, facilitating partnerships with other stakeholders such as Housing and Urban Development and the Department of Health, and building connections between sectors that supported shared goals and advanced policy-level solutions to population issues.
The push to focus on policy solutions to environmental triggers led to a smoke-free ordinance in the city, a reduction of solvents that contributed to asthma in child care centers, a reduction of school bus idling in Wilmington, integrated pest management in homes, and changes in the Medicaid drug formulary to include metered dose inhalers. These changes benefitted thousands of children in Delaware, and led to a 60% reduction in emergency room visits, a 44% decrease in asthma-related hospital admissions, and an annual reduction in medical costs of $2,100 per child. Because Nemours operates on a fee-for-service basis, however, the hospital incurred substantial revenue losses. In interventions that require long time horizons to see improved outcomes, such as weight loss, value-based care systems may be more appropriate than fee-for-service.
This intervention demonstrates a number of valuable lessons, including the benefit of identifying a short-term return on investment; leveraging the moral imperative to act by connecting it to an organization’s mission; focusing on the model instead of the topic; building partnerships and trust; blending universal and targeted approaches to address impacts on equity; supporting the role of the integrator and using it to identify an approach’s value; securing the funding and capacity for sustainability; engaging clinicians early; and building spread and scale into the model. The authors believe this model is generalizable, but may be challenging to apply to obesity because the return on investment with obesity is so delayed.
AmeriHealth Caritas District of Columbia (DC)
AmeriHealth Caritas DC (AmeriHealth) collaborates with community organizations and network providers to offer metabolic syndrome, healthy eating, and nutrition health education programs to its enrollees living with obesity, diabetes, and/or hypertension. In the various iterations of AmeriHealth’s programs, certified health educators, nutritionists, and nurses facilitate multiple interactive learning sessions over a period of time to help participants gradually understand their underlying condition and how nutrition, fitness activities, and other lifestyle behaviors can be adjusted to better manage their condition and improve their overall health. Each session is led by a subject matter expert with participation by peer educators, who serve as informal coaches for the participants and also boost engagement between sessions.
Much of the program’s effectiveness lies in the support provided by the peer educators and the sharing that occurs among participants. To monitor the effectiveness of these programs, AmeriHealth works with program facilitators to capture pre- and post- program biometrics, and for some of the programs, pre- and post- knowledge quizzes to gauge potential improvements in health literacy and participants’ knowledge about their condition. The plan has recorded statistically significant reductions in one or more of the key measures—weight, body-mass index (BMI), blood pressure, and HbA1C—as well as improvements in participant understanding of their underlying health conditions and how to better manage them. Despite documented improvements in health outcomes, it has been challenging to secure ongoing funding and scale up these programs without evidence of a clear return on investment and linkages to a decrease in the overall health care costs for this population.
Collaborative Cottage Grove
Collaborative Cottage Grove is a community-based health program in Greensboro, North Carolina that started with partnerships with the Greensboro Housing Coalition, Cottage Grove Initiative, Mustard Seed Community Health Clinic, and the New Hope Community Development Group, and later expanded to also partner with Cone Health. Community members prioritized a reduction in emergency room visits related to diabetes and asthma, as well as remediation of housing conditions that exacerbated asthma. The intersection of poverty with these factors reflected the impact of
structural racism, which had begun with the redlining of the Black community in Greensboro. The program also sought a clinical partnership with Cone Health; to build trust, it required that Cone Health come to terms with its own history of racial discrimination.
The narratives of residents about their living conditions and site visits by policy makers persuaded the Greensboro housing authority and city government to make substantial improvements in housing that successfully reduced emergency room visits for asthma, while the focus on diabetes and obesity led to the hiring of two local residents (funded by Cone Health) to conduct a Diabetes Prevention Program (DPP). The popularity of the DPP led to additional volunteer DPP leaders, the establishment of a community market, and the engagement of Cone Health medical residents. In addition, the rehabilitation of a local park increased opportunities for physical activity.
Achieving these goals has required multi-sector collaboration and the co-creation of methods and strategies with community members. The processes have prioritized resident voices and engagement in planning, decision-making, and implementation. Involving residents from the start has been integral to achieving equitable, win-win strategies and to ensuring that residents lead and sustain any changes. For example, a community advisory council is chaired by a local resident and co-chaired by a representative of an organizational partner. Representatives from Cone Health, the county Department of Health, the police department, and the Department of Parks and Recreation attend the advisory committee meetings. The degree of trust that has been achieved by Cone Health is exemplified by an extraordinary degree of access to Cone Health’s Healthy Community Director. The success of these collaborations has led to the diversification of funding from groups other than Cone Health.
Common Elements of the Five Programs
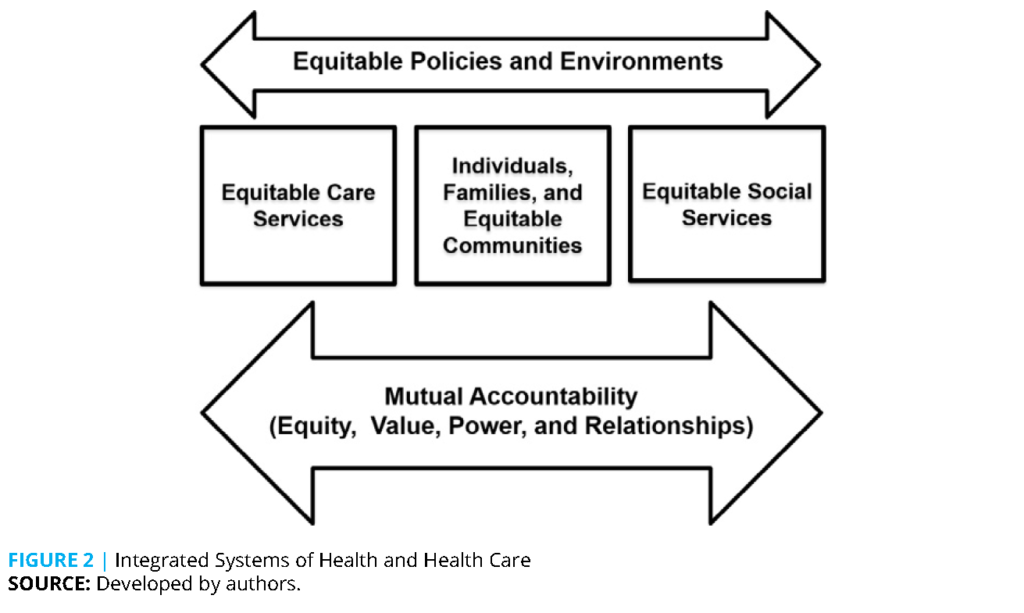
The original intent of the Integration Summit was to explore the extent to which new models of integration could inform and modify our 2015 framework for the prevention and management of obesity. While only one of the models discussed focused specifically on obesity, all programs offered a number of insights and lessons learned. The revised model created by the authors is illustrated in Figure 2.
First, concerns were raised during the discussion that the 2015 framework was overly clinical. Second, based on the observation that clinical and public health initiatives were converging, “social services” was deemed a more appropriate term than “social systems.” Finally, the authors felt that equity needed to permeate the model.
The 2015 framework included a number of elements of integration, including the convener, advocacy, data exchange, financing, governance, referral process, and communication. These are not elements that integrate systems, however, but rather characteristics of successfully integrated systems. Only those elements common to the 2015 framework and discussed during the summit are considered below.
The insights, outcomes, and conclusions that follow emerged from the presentations and discussions both before and during the summit.
The figure is an adaptation and simplification of the original ICSSPMO figure based on the recommendations of the summit attendees. Equity permeates the framework. The care delivery and community systems have been recast as care services and social services to emphasize their role in supporting individuals, families, and communities. The arrow formerly used to reflect integration, and the elements necessary to achieve integration (Dietz et al., 2015), now emphasize the mutual accountability of clinical and community services, which depend on equity, value, power, and relationships. Equity, value, power, and relationships are also determined by equitable policies and environments.
Compelling Rationale for Action
For all groups, local data—either qualitative or quantitative—informed their focus. For example, the Collaborative Cottage Grove used qualitative data in the form of stories about families living among sewage in a substandard housing complex to attract the attention of policy makers. Quantitative outcome data were used to monitor the success of the AmeriHealth program.
Another compelling rationale for action in several of the models was a focus on SDoH. In KP’s case, 35 prior efforts to focus on SDoH were unconnected. Recognizing the need for medical providers to ask about social needs during visits led to an effort to develop a system that connected members’ needs to services. In this way, KP’s actions focused on addressing the needs consequent to SDoH rather than addressing the SDoH directly. Nationwide’s decision was driven by the contrast between the high quality of services the hospital provided and the context of its immediate neighborhood, which was characterized by violence, poverty, and poor housing. The hospital board’s recognition that becoming a great health care system required addressing SDoH led to their local investments in housing.
Equity
There was wide agreement at the summit in 2020 that equity, which was an all-encompassing principle in the 2015 framework, needed to permeate any future model. A truly integrated model would need to establish an equitable balance of power and provide resources as well as free information interchange between health care and community systems. A focus on equity also has clear implications for governance, with equal weight accorded to clinical and community organizations. Another suggestion was to place equity, value, power, and relationships at the center of the model. Of the five models, Cottage Grove provides the best example of equity, shared power, and relationships. There was also a suggestion that “Care Delivery” be changed to “Service Delivery” to reflect the expansion of traditional care delivery to include human and social service providers and other types of people who provide care. These points were incorporated into Figure 2.
Role of the Integrator
The integrator functions as a bridge between different components of the framework, and has the critical ability to listen, learn, and integrate service delivery and community systems while authentically engaging residents. Integration is central to the framework, and must be considered alongside all other framework elements. In addition to connecting elements of the framework, the integrator is responsible for providing enhanced alignment of purpose, shared ownership, shared leadership, and shared decision-making. Responsibilities include monitoring and ensuring shared power in how decisions are made, as well as safeguarding trustworthiness of the process. Integration should occur at multiple levels— individual, organizational, and policy and systems. Because integration is built on trust and takes time to evolve, the framework could also include a time element.
All integration functions do not need to exist within a single entity, and the choice of a leader or leaders is context-specific. It is particularly important to include representatives from the involved community who can share its historical and present context, because authentic community representation is essential to build trust and inform decision-making processes, such as allocation of resources. It is more difficult to establish, however, whether representatives truly represent the community. The concerns that initiated these examples of integration were quite diverse—addressing SDoH by KP and Nemours, the Board of Nationwide, and housing in Greensboro.
Governance
Governance is critical to integration, especially with regards to who determines the integrator or backbone organization. As discussed at the summit, one of the limitations of the 2015 framework is that it appeared overly clinical and lacked flexibility. This limitation appeared to apply especially to the examples driven by payers or plans, like KP and Nationwide, in which decision-making appeared weighted toward the system rather than the community. The community-driven model appeared much more agile. For example, Collaborative Cottage Grove could rapidly hire community health workers from their community (community credentialed) without the human resources restrictions of health plans or hospitals (plan credentialed). In addition, a community-based integrated approach such as the one undertaken by Cottage Grove may be more likely to achieve equity, and more likely to directly address issues like structural racism.
The success of the Collaborative Cottage Grove program also required building trust between the community and the partner health system, Cone Health. Such trust is essential to holding partners mutually accountable. Here, Collaborative Cottage Grove played a key role as an integrator. Although not considered at the Integration Summit, the “Invest Health initiative,” a project of the Reinvestment Fund focused on small to mid-size cities (with support from the Robert Wood Johnson Foundation), noted several elements that have been critical to successfully impacting precursors of systems change and targeting investments to communities that may improve the health and wellbeing of their residents. These include having strong leaders with a clear and aligned vision, working across sectors with an understanding of the connection between health and the built environment (Mt. Auburn Associates, 2020). There are a number of challenges here. First, it is difficult to develop and nurture leadership if it does not yet exist. In other cases, there may be nascent leaders that require a structure to empower them. However, medical systems may not recognize that their success depends on shared decision-making, and may be reluctant to share or accede power. Power sharing depends on trust, and trust depends on the strength of relationships. The extent to which medical systems share power in decision-making with their communities is a major, and often implicit, challenge (Franz et al., 2018; Skinner et al., 2018).
In these case examples, the processes for decisionmaking were quite variable, and were either outside in (top down), inside out (community-based), or some balance of the two, depending on the issue. For example, Nationwide Children’s process began when the hospital board committed to devote resources to a community program, whereas Collaborative Cottage Grove was community-based from the outset, and Nemours utilized a mix of the models.
Collecting and Using Data
Payer- and plan-driven systems tend to focus on clinical outcomes that may not align with the outcomes of interest to communities. For example, in Greensboro, Cone Health wanted to see a reduction in ER visits, while the Cottage Grove community wanted changes in housing. In addition, clinical outcomes typically lead to results much more quickly than changes in population metrics (as demonstrated by the short-term results for reduced asthma ER visits in Nemours vs. the longer-term health related changes achieved in Columbus). Cottage Grove combined qualitative and quantitative metrics to help tell its story and demonstrate a return on investment.
The differences in priorities between partners emphasizes the need to agree on and prioritize outcomes. Clinical outcomes are important, and their effects on costs can be readily demonstrated. Nonetheless, behavioral and quality-of-life outcomes that reflect current and future health are also critical metrics for both health plans and communities. Prevention metrics are more population-based. Finances, jobs, productivity, life satisfaction, or social connectedness can be used as measures of health and well-being, but their effects on costs are less immediate. These are outcomes that may be higher priorities for health plan members than for the health plan. The challenge is whether and how health plans can agree on the same priorities as their population, and how shorter-term clinical outcomes can be linked to longer-term improvements in population health or SDoH. For example, Nationwide’s most immediate focus has been on the physical, social, and economic determinants of health, and they recognize that there may be a significant time delay before their efforts to address the SDoH are reflected in improved clinical outcomes, like obesity.
Financing
Fee-for-service reimbursement drives patient volume rather than clinical outcomes, whereas value-based systems provide flexibility about how to achieve those outcomes, and metrics can include key steps to improved care. The multiple dimensions of money flows may not be fully represented in the 2015 and revised frameworks. For example, money flows from Medicaid to providers and also from organizations to community individuals who are involved in the system. Cottage Grove and Nationwide provide useful examples of local investment achieved through local hiring.
A broader issue is how to sustain funding for these programs. For example, Accountable Communities for Health provide a funding mechanism that could allow health plans to focus on long-term health outcomes that may ultimately save costs. However, a major challenge is that it is easier to pay for specific interventions than for the infrastructure necessary to sustain these organizations (Hughes and Mann, 2020). Furthermore, successful interventions conducted by a fee-for-service system, like those employed by Nemours, provide a disincentive for continued investments when the health care system loses money. The Nemours experience suggests that value-based systems may be better suited for interventions like obesity because the benefits of weight loss require a longer time horizon to see improved outcomes and reductions in comorbidity. Payers, such as AmeriHealth Caritas, may also benefit from a shift to a value on investment framing rather than a positive balance sheet and consider partnering on a collectively funded infrastructure to support interventions for a shared member-base between multiple payers.
The COVID-19 Opportunity
The SARS-CoV-2 outbreak erupted shortly after the summit, and led health care organizations to redirect their resources to address the acute demands of the pandemic. Alongside this, the adverse course and increased mortality of COVID-19 infections in people with obesity and people of color have highlighted the health inequities that have contributed to these disparities. The pandemic has emphasized the need for effective obesity prevention and mitigation strategies, and has renewed awareness of the need to address the social, physical, and economic determinants of health. Beyond the acute response to the pandemic is the opportunity to rebuild health and social systems to address equity and to implement health, social, and economic strategies to make individuals and communities more resilient in the face of future threats. Any post-COVID-19 system redesign will benefit from the identification of systemic changes that address equity, social determinants, and the important comorbidity of obesity.
Summary and Application to Obesity
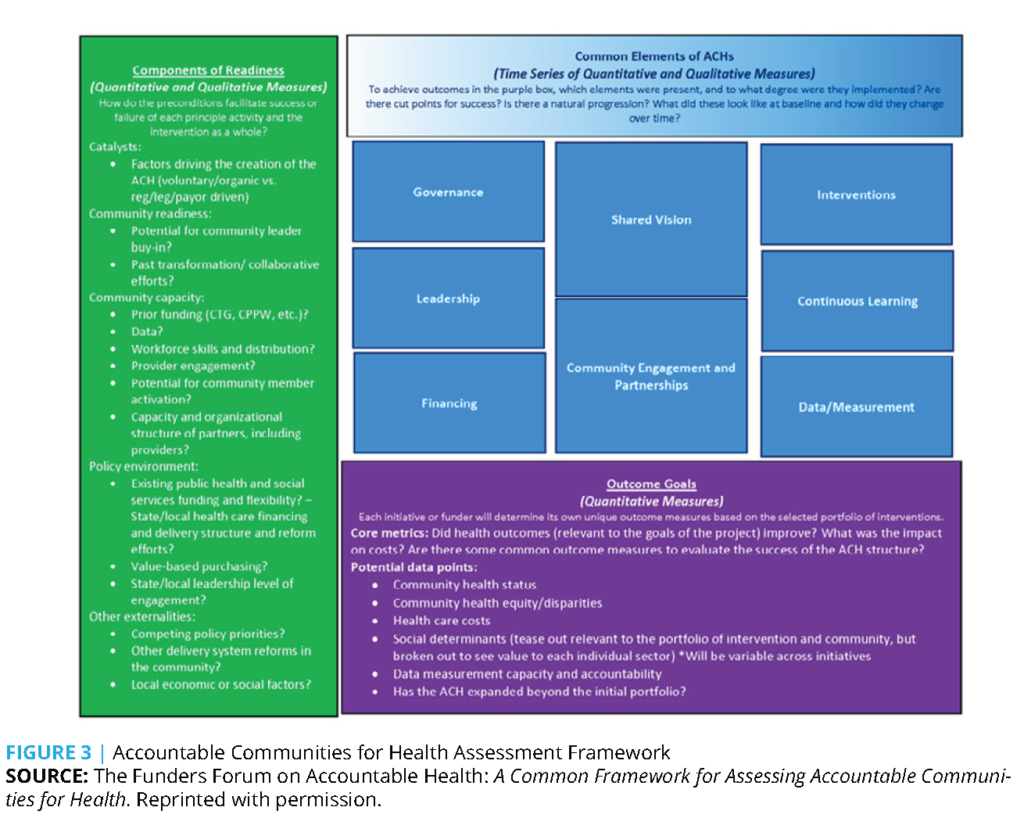
The common elements of the integrated systems reviewed here overlap considerably with the common elements of Accountable Communities for Health (Figure 3) and elements of our 2015 framework. These include leadership, governance, financing, and data. These preconditions for an integrated system are not universal, however, and strongly depend on the local context, such as who will lead the initiative and whether local resources are available. The five examples presented here varied substantially in their approach, depending on the local context and needs, and had variable community engagement, with only the Collaborative Cottage Grove initiative originating within the community itself. The variability across the five models presented at the summit emphasizes that these integrated models may not be readily spread or scaled. Furthermore, without local investments to create the preconditions necessary for change, integrated systems will only be possible in a limited number of communities.
The 2015 framework emerged from the recognition that an integrated approach was necessary to address obesity. Because the prevalence of obesity is 42% in adults and 19% in children, we will not be able to treat our way out of the obesity epidemic (Hales et al., 2020; Fryar, Carroll, and Afful, 2020). Furthermore, because many people with obesity blame themselves for their disease, there is not a demand for services to address obesity, as there is with other chronic illnesses. Most interventions have been driven by clinical systems, and a number of carefully designed randomized trials to prevent childhood obesity have failed, in part because the community context was not adequately addressed (Dietz, 2019; Kumanyika, 2017). Community-based initiatives that partner with health systems are rare. However, health care delivery systems can become models for community initiatives by modeling the strategies that communities can adopt. For example, prompted by the Boston Public Health Commission, a group of hospitals collectively reduced the availability of sugary drinks because of their association with obesity (Block et al., 2010; Boston Public Health Commission, n.d.). KP has made physical activity a vital sign in an effort to prompt providers to ask and potentially counsel their patients about the importance of physical activity (Sallis, 2017).
Multiple community-based services and strategies are required to reinforce clinical efforts to address obesity, and none of the five models discussed here provides the broad array of partners needed to adequately address obesity. For example, strategies that promote physical activity and improve access to healthful foods in schools, worksites, and communities must complement clinical efforts. Some of these strategies directly address SDoH, such as the availability of supermarkets and safe places for physical activity. Federal programs that were not explicitly identified in the 2015 framework, such as the National School Lunch Program and the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC), have successfully reduced the prevalence of obesity in low income children and adolescents (Dietz, 2021). However, community programs that directly address obesity may be less effective, or perceived as a lower priority, because of the stigma and bias associated with obesity. For example, in Cone Health’s partnership with Cottage Grove, Cone Health wanted to focus on obesity while the community’s priorities were asthma, diabetes, and housing. The resulting collaboration initiated the Diabetes Prevention Program (DPP)—more appealing to patients than a focus on weight loss, although the DPP is clearly a weight control program (Diabetes Prevention Program Research Group, 2002).
Notably, health departments—which were not explicitly included in the 2015 framework—were only involved in one of the five models discussed. Yet health departments are ideally suited to be conveners because of their mission and their broad community contacts. Although integrated programs should engage health departments, collaboration is often hampered by the limited funding for health departments, leadership turnover, local politics, and sudden shifts in priorities and resources like those required for COVID-19 often limit their engagement.
One critical area that the 2015 framework did not address is the elements of readiness, which include a catalyst, community capacity, the policy environment, and other externalities like competing policies and community readiness, community capacity, competing policy priorities, and local economic and social factors (Figure 3).
An additional concern is funding. Because fee-for-service plans generally require an early return on investments, they are less likely to invest in diseases, such as obesity, for which a longer time horizon for positive outcomes is required. Value-based care investments are better suited for obesity (and other similar) programs, but to date, we are not aware of any integrated system or ACH which has directly focused on obesity.
In summary, with respect to applying lessons learned to obesity, the 2015 framework is universal in that it can be applied to a variety of health issues. However, as the five models discussed at the summit demonstrate, the specific approach and messaging must be tailored to a community’s context and needs. Furthermore, investments in upstream SDoH such as housing and transportation could create more stable social and physical environments that better support people’s abilities to make healthy lifestyle choices. Although none of the five examples presented at the summit specifically addressed obesity, they all point to the need for equity, shared power, and long-term investments like value-based care. Investing in authentic community engagement, equitable policies and strategies, the lived experience of people with obesity, and sustained engagement and coordination among multiple services will be required to address the widespread and costly disease of obesity.
Join the conversation!
![]() Tweet this! “A truly integrated model needs to have an equitable balance of power and provide resources as well as free information interchange between health care & community systems.” A new #NAMPerspectives centers equity in obesity prevention & care: https://doi.org/10.31478/202111a
Tweet this! “A truly integrated model needs to have an equitable balance of power and provide resources as well as free information interchange between health care & community systems.” A new #NAMPerspectives centers equity in obesity prevention & care: https://doi.org/10.31478/202111a
![]() Tweet this! Authors of a new #NAMPerspectives highlight that successfully integrated community health programs involve residents from the start to create equitable strategies and support residents to lead and sustain changes: https://doi.org/10.31478/202111a
Tweet this! Authors of a new #NAMPerspectives highlight that successfully integrated community health programs involve residents from the start to create equitable strategies and support residents to lead and sustain changes: https://doi.org/10.31478/202111a
![]() Tweet this! “Investments in upstream SDoH such as housing and transportation could create more stable social and physical environments that better support people’s abilities to make healthy lifestyle choices.” Read more in a new #NAMPerspectives: https://doi.org/10.31478/202111a
Tweet this! “Investments in upstream SDoH such as housing and transportation could create more stable social and physical environments that better support people’s abilities to make healthy lifestyle choices.” Read more in a new #NAMPerspectives: https://doi.org/10.31478/202111a
Download the graphics below and share them on social media!
References
- Dietz, W. H., L. S. Solomon, N. Pronk, S. K. Ziegenhorn, M. Standish, M. M. Longjohn, D. D. Fukuzawa, I. U. Eneli, L. Loy, N. D. Muth, E. J. Sanchez, J. Bogard, and D. W. Bradley. 2015. An Integrated Framework For The Prevention And Treatment Of Obesity And Its Related Chronic Diseases. Health Affairs (Millwood) 34(9):1456-63. https://doi.org/10.1377/hlthaff.2015.0371.
- Kaiser Permanente Washington Health Research Institute. 2021. Improving Chronic Illness Care. Available at: http://improvingchroniccare.org/index.php?p=The_Chronic_Care_Model&s=2 (accessed September 30, 2021).
- Dietz, W., J. Lee, H. Wechsler, S. Malepati, and B. Sherry. 2007. Health plans’ role in preventing overweight in children and adolescents. Health Affairs (Millwood) 26(2):430-40. https://doi.org/10.1377/hlthaff.26.2.430.
- Mt. Auburn Associates. 2020. Evaluation of Invest Health: Findings. Available at: https://www.investhealth.org/wp-content/uploads/2020/01/Invest-Health-Final-Public-Report_8-31-2018-1.pdf (accessed September 30, 2021).
- ODPHP (Office of Disease Prevention and Health Promotion). 2021. Social Determinants of Health. Available at: https://health.gov/healthypeople/objectives-and-data/social-determinants-health (accessed September 30, 2021).
- Franz, B., D. Skinner, A. M. Kerr, R. Penfold, and K. Kelleher. 2018. Hospital-Community Partnerships: Facilitating Communication for Population Health on Columbus’ South Side. Health Communication 33(12):1462-74. https://doi.org/10.1080/10410236.2017.1359033.
- Skinner, D., B. Franz, M. Taylor, C. Shaw, and K. J. Kelleher. 2018. How U.S. children’s hospitals define population health: a qualitative, interview-based study. BMC Health Services Research 18(1):494. https://doi.org/10.1186/s12913-018-3303-7.
- Hughes, D. L., and C. Mann. 2020. Financing The Infrastructure Of Accountable Communities For Health Is Key To Long-Term Sustainability. Health Affairs (Millwood) 39(4):670-8. https://doi.org/10.1377/hlthaff.2019.01581.
- Hales, C. M., M. D. Carroll, C. D. Fryar, and C. L. Ogden. 2020. Prevalence of obesity and severe obesity among adults: United States, 2017-2018. Available at: https://www.cdc.gov/nchs/products/databriefs/db360.htm (accessed September 30, 2021).
- Fryar, C. D., M. D. Carroll, and J. Afful. 2020. Prevalence of overweight, obesity, and severe obesity among children and adolescents aged 2–19 years: United States, 1963–1965 through 2017–2018. Available at: https://www.cdc.gov/nchs/data/hestat/obesity-child-17-18/obesity-child.htm (accessed September 30, 2021).
- Dietz, W. H. 2019. We Need a New Approach to Prevent Obesity in Low-Income Minority Populations. Pediatrics 143(6). https://doi.org/10.1542/peds.2019-0839.
- Kumanyika, S. 2017. Getting to Equity in Obesity Prevention: A New Framework. NAM Perspectives. Discussion Paper, National Academy of Medicine, Washington, DC. https://doi.org/10.31478/201701c.
- Block, J. P., A. Chandra, K. D. McManus, and W. C. Willett. 2010. Point-of-purchase price and education intervention to reduce consumption of sugary soft drinks. American Journal of Public Health 100(8):1427-33. https://doi.org/10.2105/AJPH.2009.175687.
- Boston Public Health Commission. n.d. Healthy Beverages. Available at: http://www.bphc.org/whatwedo/healthy-eating-active-living/healthy-beverages/Pages/Healthy-Beverages.aspx (accessed September 30, 2021).
- Sallis, R. 2017. The physical activity vital sign and electronic health records: the Kaiser Permanente experience. Integrating EIM into Healthcare. Available at: https://www.aspetar.com/journal/upload/PDF/20175417940.pdf (accessed September 30, 2021).
- Dietz, W. H. 2021. Better Diet Quality in the Healthy Hunger-Free Kids Act and WIC Package Reduced Childhood Obesity. Pediatrics 147(4). https://doi.org/10.1542/peds.2020-032375.
- Diabetes Prevention Program Research Group. 2002. The Diabetes Prevention Program (DPP): description of lifestyle intervention. Diabetes Care 25(12):2165-71. https://doi.org/10.2337/diacare.25.12.2165.
- Dietz, W. H., B. Belay, D. Bradley, S. Kahan, N. D. Muth, E. Sanchez, and L. Solomon. 2017. A Model Framework That Integrates Community and Clinical Systems for the Prevention and Management of Obesity and Other Chronic Diseases. NAM Perspectives. Discussion Paper, National Academy of Medicine, Washington, DC. https://doi.org/10.31478/201701b.