A Journey to Construct an All-Encompassing Conceptual Model of Factors Affecting Clinician Well-Being and Resilience
 NOTE: This model may be continually updated post-publication. To view the latest version, please click here.
NOTE: This model may be continually updated post-publication. To view the latest version, please click here.
If you are suicidal and need emergency help, call 911 immediately or 1-800-273-8255 if in the United States. If you are in another country, find a 24/7 hotline at www.iasp.info/resources/Crises_Centres.
Introduction
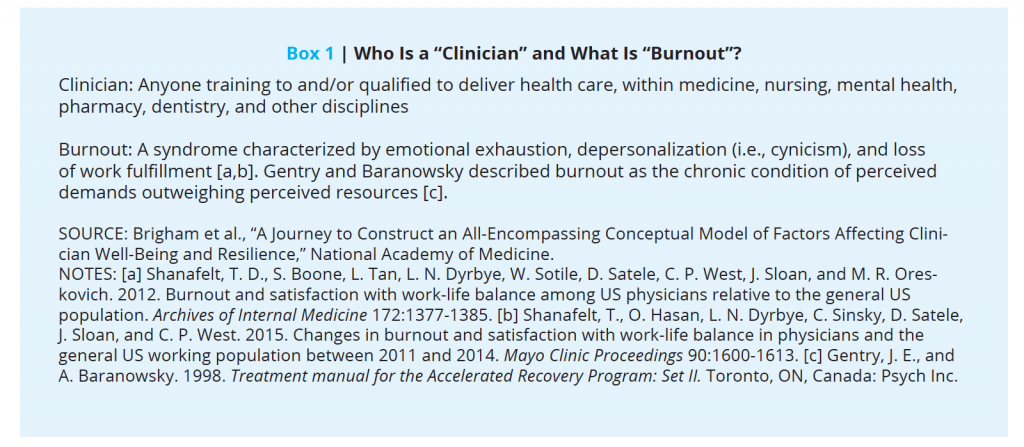
In 1999, the Institute of Medicine (IOM) released its landmark report, To Err Is Human: Building a Safer Health System [1], which revealed that a significant number of people die annually from medical errors. The report spurred two decades of action on the part of hospitals and health care professionals to improve patient safety. The IOM, renamed the National Academy of Medicine (NAM), is now addressing the issue of clinician well-being. The Action Collaborative on Clinician Well-Being and Resilience (the “action collaborative”) was launched in January 2017 in response to the burgeoning body of evidence that burnout is endemic and affects patient outcomes. The action collaborative has defined “clinician” and “burnout” in Box 1.
In the article “From Triple to Quadruple Aim: Care of the Patient Requires Care of the Provider,” Sinsky and Bodenheimer conclude that clinician burnout is associated with lower patient satisfaction and reduced health outcomes, and may increase costs, thereby endangering the Triple Aim [2]. Dyrybe et al. identified that the rapidly changing US health care environment, including new payment and delivery approaches, the electronic health record (EHR), and publicly reported quality metrics, have profoundly affected clinician well-being [3]. There is no question that the recent pressures to decrease the cost of health care, raise clinical quality, and improve the patient experience have greatly increased the load clinicians must carry. In a 2014 study, physicians displayed higher rates than the general US working population of emotional exhaustion (43.2 percent versus 24.8 percent), depersonalization (23.0 percent versus 14.0 percent), and overall burnout (48.8 percent versus 28.4 percent), and reported lower satisfaction with work-life balance (36.0 percent versus 61.3 percent), as measured by the Maslach Burnout Inventory (MBI) and two single-item measures adapted from the full MBI [4]. These effects were seen after controlling and adjusting for age, sex, relationship status, and hours worked per week. Despite recognition of the importance of clinician well-being, the ongoing exacerbation of burnout among physicians increased from 2012 to 2017 [5,6]. Nurses face similar challenges. Based on studies conducted in 1999, 2007, and 2012, nurses displayed a high prevalence of burnout and depression. Forty-three percent of in-patient nurses [7], 35 percent of hospital nurses, 37 percent of nursing home nurses, and 22 percent of nurses working in other settings had a high degree of emotional exhaustion [8]; 18 percent of in-patient nurses had depression compared with a national prevalence of approximately 9 percent [9].
The focus of the action collaborative is not limited to the negative outcomes of burnout or its absence alone. The initiative has a broader focus of improving well-being and alleviating fatigue, moral distress, and suffering—components that are not included in the classic definition of burnout. A key outcome is to understand the broader phenomenon of clinician well-being, and to help clinicians achieve a state of personal fulfillment and engagement that leads to joy in practice, and ultimately, a connection to why one went into health care in the first place. The effort encompasses clinicians broadly because well-being is important to and clinical outcomes are affected by all members of the interprofessional health care team, including trainees and students.
Although there are widely used definitions of well-being and burnout, there has been no agreed-upon conceptual model of the underlying contributing factors, which could serve as the foundation to identify potential solutions to promote well-being, prevent and treat burnout, and guide further research. Earlier models, although having great utility, lack some important attributes and raise challenging questions [10]:
- Who or what should be at the center of the model?
- How should the model represent the effects of both external, systemic causes and internal, individual factors, and the interrelationship among the factors?
- How should the model convey that burnout exists at all stages of the clinician’s life cycle—from student to early career clinician, from mature clinician to nearing retirement?
- What is the most effective way to articulate that factors and solutions will differ among the clinical disciplines and may depend upon the learning and practice environment (e.g., academic, community, inpatient, or outpatient settings)?
Review of Existing Models
Resource/demand balance
There are many conceptual models for workplace well-being and related elements (e.g., burnout, engagement, resilience) [11-23]. A theme common across models is that well-being is a function of the relationship between demands and resources. An exemplar is the Job Demands–Resources model [14,20]. Resources are the work conditions that facilitate achieving work goals, stimulate worker growth, and attenuate accumulating costs of work demands. Although resources can be monetary, in most instances they are not—for example, a frequently cited resource is autonomy and control over practice. Demands are the work elements requiring physical, cognitive, or emotional efforts. There are different types of demands. Hindrance demands interfere with or undermine job satisfaction and quality-of-care goals. For example, excessive workloads for nurses have been linked to burnout and poor patient outcomes [7,24]. Similarly, time demands arising from electronic health record documentation requirements contribute to physician burnout [25]. Challenge demands require effort, but can be invigorating and make work rewarding. For example, working with patients at the end of life can be stressful and emotional, but in a supportive and resourced work environment, it can also be extraordinarily rewarding. Thus, great reward can come with the intensely interpersonal nature of clinical care and the clinician-patient relationship. However, even the most dedicated clinician, in the wrong context, can become demoralized and detached from patients to guard against the stress that comes, not from highly relational work in the abstract, but from specific organizational environments and cultures that are insufficiently resourced to sustain and refresh clinicians in their efforts. Clinicians pursue health care fully expecting challenging demands, but become frustrated when their efforts are thwarted by organizational failures and barriers that hinder their ability to provide good care.
Primacy of external factors
Most models reference both individual (e.g., internal) and external (e.g., environmental and organizational) resources and demands. The research suggests that external factors carry more weight in contributing to burnout [1,13]. Focusing on the individual suggests that burnout arises as individuals are unable to adapt to the learning and practice environment; focusing on the organization suggests that it is the environment that should adapt to promote quality of care and clinician well-being. Evidence suggests that system attributes such as workload, autonomy and control over practice, quality of the work environment, and shared governance are key organizational factors linked with clinician burnout and well-being [5,25,26,27,28,29]. Maslach and Leiter’s framework for burnout indicates that “it is paradoxical that most interventions to alleviate burnout focus on individuals since the research suggests that situational and organizational factors play a bigger role in burnout [11].”A similar conclusion was reached in To Err Is Human [1,30], which placed the responsibility for patient safety with systems rather than individuals and called for fixing what has been called the “sick system syndrome [25].” The same holds true for clinician well-being.
Outcomes
The focus of most models is worker well-being where outcomes include well-being, burnout, health, or engagement [5,25,26,27,28,29]. Research also points to effects on patients (e.g., poor outcomes) [8,31,32,33,34] as well as effects on the health system (e.g., productivity, turnover, and innovation) [35,36,37]. Little attention has been given to a holistic view of the problem, including addressing and altering the systemic environmental dynamics.
The NAM Model
Despite the utility and applicability of existing models of well-being and burnout, the Conceptual Model working group did not find a model that depicts the factors associated with burnout and well-being, applies them across all health care professions and career stages, and clearly identifies the link between clinician well-being and outcomes for clinicians, patients, and the health system. For this reason, the working group agreed to develop a new model. Several elements from earlier designs were incorporated into the NAM model, and the working group members are indebted to the organizations, authors, and researchers for their foundational work.
In creating the model, the working group took into account the diversity of the health care team, types of practice setting, and career stage. The resultant model is not used to measure or assess burnout; rather it reflects the factors affecting clinician well-being and resilience. In this way, the model can be applied to a range of disciplines, settings, and career stages. Despite being career-naïve, students are experiencing burnout at a frequency similar to that of clinicians who have completed their training, indicating that significant attention should focus on the learning and practice environments to promote well-being for future generations in all health professional fields. Therefore, the NAM model considers the learning and practice environment as well as learner-specific and practice-specific factors, and creates a broad system approach applicable across all health care professions, learning environments, and stages of clinician career development. The working group was further guided by the principle to avoid stigmatizing clinicians for being burned out, and to instead draw attention to the external factors that decrease well-being.
Model shape
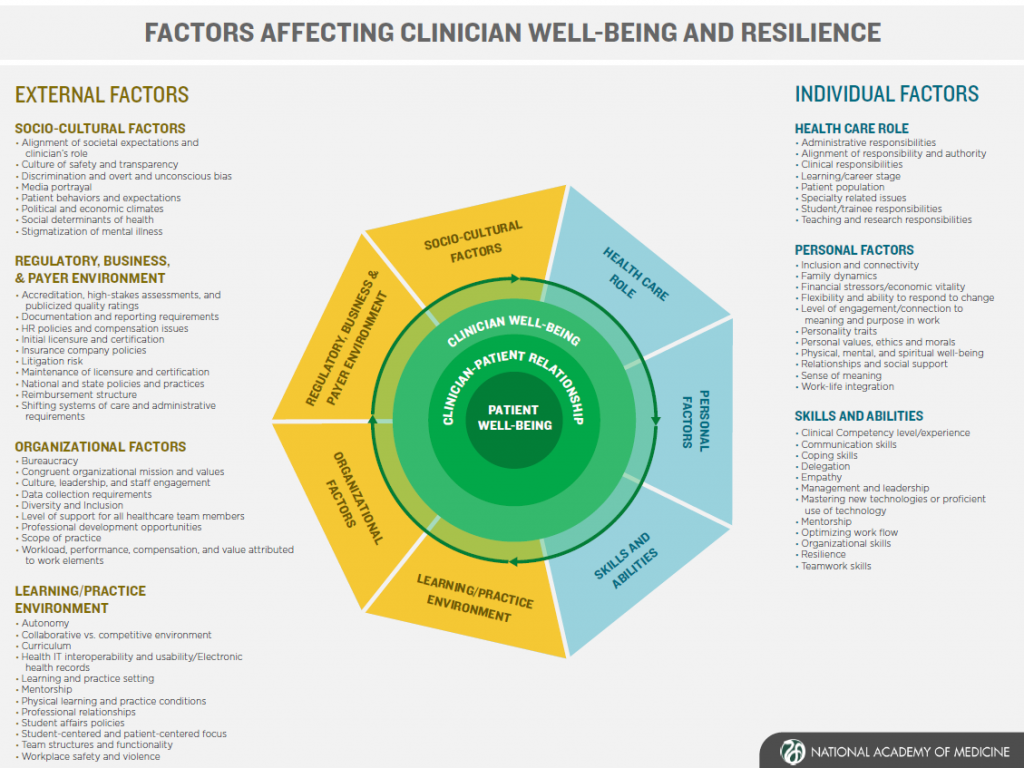
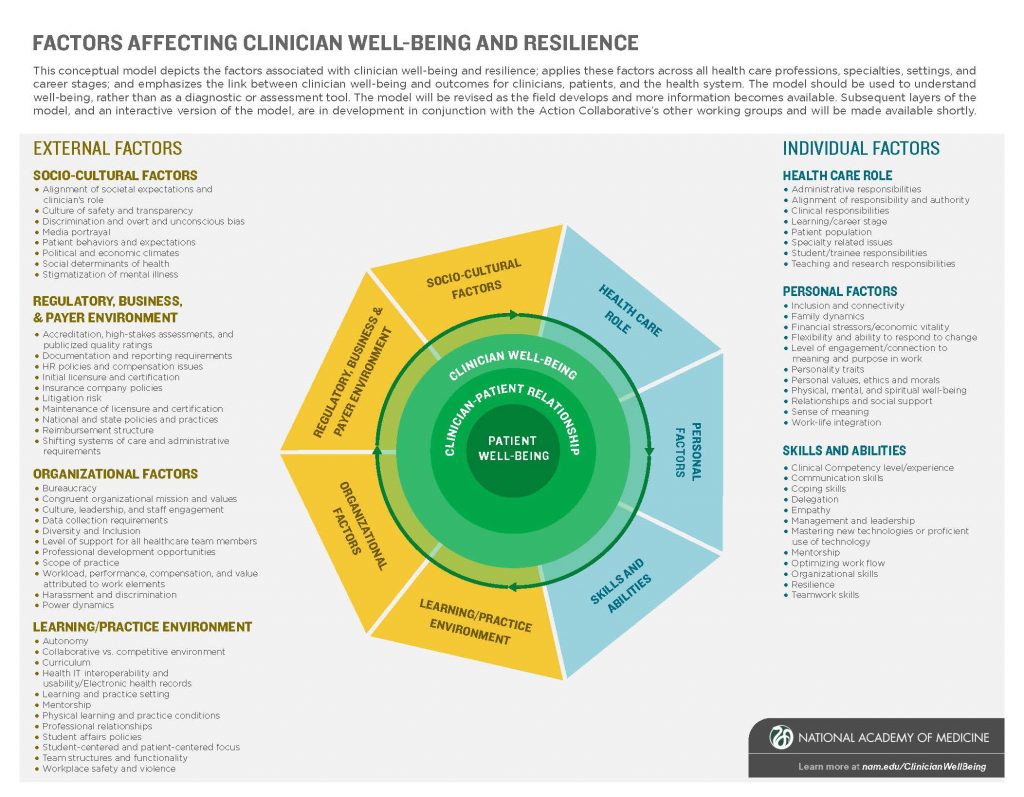
Creating a conceptual model that captures the complexity of clinician well-being and resilience without oversimplifying the contributing factors was a challenge. Indeed, the figure was created via an iterative process and is expected to change and evolve as new research emerges and contributes to our understanding of burnout, resilience, and well-being (see Figure 1, “Factors Affecting Clinician Well-Being and Resilience”). Starting from the inside out, the nucleus is composed of three distinct but related elements. At the center is patient well-being; without the patient, there is no clinician. Next is the clinician-patient relationship, followed by clinician well-being. Encircling the nucleus are external and individual domains that affect clinician well-being and resilience. Among the external factors are Socio-Cultural Factors; the Regulatory, Business, and Payer Environment; Organizational Factors; and the Learning/Practice Environment. On the individual side, contributing factors are Health Care Role, Personal Factors, and Skills and Abilities. Each domain is further subdivided by elements that have significance for clinician well-being and burnout. In recognition of the complexity of clinician well-being, these elements are listed in alphabetical order. Subsequent discussion papers will describe the domains in more detail. The intent was not to prescribe a hierarchy; instead, users will determine the salience of the elements on a situation-by-situation basis. This integrated approach creates an opportunity to identify potential leverage points and generate solutions at the individual, organizational, and systems level. Based on this model, more granular models can be developed for particular specialties and environments.
Figure 1 | Factors Affecting Clinician Well-Being and Resilience
SOURCE: NAM Action Collaborative on Clinician Well-Being and Resilience, 2017.
NOTE: This model may be continually updated post-publication. To view the latest version, please click here.
Key considerations for the model
Clinician well-being, resilience, and burnout are complex, multidisciplinary issues [3] that require a systems-thinking approach [38] to realize the full scope, identify pressure points, and drive action needed for meaningful and sustainable improvements. The model captures the magnitude and urgency of challenges to clinician well-being while simultaneously conveying a vision and solutions. The Conceptual Model working group incorporated several qualities into the model. First, the model captures the relationship between the clinician and the patient; without the patient, the clinician does not exist. Second, the model accounts for the individual and external factors that contribute to burnout or well-being [4] and depicts the complex interconnectivity of the various dimensions affecting well-being, demonstrating that well-being is most often affected by the interaction of external and individual forces. Simultaneously, the more numerous external factors illustrate that external factors in systems and culture often have a larger effect on clinician well-being than individual factors do [13]. The arrows around the nucleus convey the interconnectivity and fluidity of the factors that affect well-being.
Notable Lessons Learned in the Creation Process
While developing the model, working group members learned many lessons—some expected and some unexpected. The group initially planned to adopt an existing explanatory model of clinician well-being and resilience, but quickly realized that no single model covered the spectrum of environments, health professions, and learner/practitioner developmental stages that were intended to be reflected in this holistic model. A major challenge arose in designing a model that was detailed enough to serve as a tool for understanding and to develop interventions, yet not so detailed that it was overwhelming. Achieving the desired balance of external and individual factors, and identifying the appropriate terminology for those factors, took more time than anticipated. Issues related to terminology included avoiding terms that might stigmatize individuals, such as lack of resilience.
To ensure utility across a range of stakeholders, working group members assessed the model’s responsiveness to eight scenarios that reflect real-life situations experienced by health care professionals. Scenarios ranged from a trainee threatening suicide to an administrator seeking guidance toward creating an environment that promotes resilience among health professions students. In each case, the model was deemed useful if it helped stakeholders achieve three objectives:
- understand individual and systemic contributors to burnout and lack of well-being;
- identify methods for addressing an individual or systems-level barrier to well-being; and
- recommend pathways to prevent or treat burnout, and promote well-being for clinicians and the environments in which they learn and practice.
Based on the scenario exercise, the model emerged as a useful tool across situations, environments, health professions, and career stages. In particular, it can be employed by individuals and organizations to understand the factors driving burnout, to potentially prevent burnout, and to increase clinician well-being and resilience. However, the true potential of the model will not be realized without a layered approach that links the explanatory model to up-to-date research and useful tools and strategies for diagnosis, prevention, and treatment.
Intersections with the Other Action Collaborative Working Groups
The Conceptual Model working group is one of four action collaborative work streams, all of which are intimately linked and reinforce one another. The model proposes a comprehensive set of domains and factors that affect clinician well-being and resilience. Many of these factors are further expounded upon in an accompanying legend. Most terms are defined using definitions from seminal literature, whereas others have no commonly agreed-upon definition and are described based on the intent with which they were included in the model. The legend is meant to provide further context for factors in the conceptual model and those used throughout the collaborative. This legend of terms forms the basis of a common taxonomy used across the working groups and helps guide resource development.
The Research, Data, and Metrics group aggregated a list of valid and reliable instruments that can be used to assess clinician burnout across several factors included in the conceptual model. The group is also creating an annotated bibliography of interventions that address many of those model’s factors. Similarly, the External Factors and Workflow group is developing two papers, “Care-Centered Clinical Documentation in the Digital Environment” and “Implementing Team-Based Care to Reduce Clinician Burnout.” These papers address several external domains and factors that affect well-being, as reflected in the model. The Messaging and Communications group uses the conceptual model as a foundation for communicating with multiple stakeholders. Group members are also developing a knowledge hub, which will be an open-access repository that collates research and resources informed by the conceptual model and produced by the action collaborative and other organizations committed to improving clinician well-being. The hub is expected to launch in winter 2018.
Conclusion
The Conceptual Model working group set out to create a model that could be used by individuals and organizations to understand the causes and effects of burnout, identify strategies to prevent and treat burnout and promote well-being, and improve health care delivery and patient outcomes. The model depicts the domains and factors associated with burnout and well-being, and applies them across all health care professions and career stages, including that of the student, and clearly identifies the link between clinician well-being and outcomes for clinicians, patients, and the health system. Group members will update and refine the model as future research is undertaken in this area. The goal is for this model to be a useful tool to increase knowledge and understanding about clinician well-being, to further research in this area, and to design effective and appropriate methods to decrease clinician burnout and to increase well-being and joy in learning and practice. Working group members envision that the work of the action collaborative will spur action on the part of hospitals and health care professionals in the same ways as To Err Is Human.
Join the conversation!
![]() Tweet this! Despite a number of existing models describing clinician well-being and burnout, few probe the reasons why so many clinicians are experiencing alarming rates of burnout. A new model from @theNAMedicine’s Action Collaborative on Clinician Resilience and Well-Being: http://ow.ly/dz8k30i1je4 #ClinicianWellBeing
Tweet this! Despite a number of existing models describing clinician well-being and burnout, few probe the reasons why so many clinicians are experiencing alarming rates of burnout. A new model from @theNAMedicine’s Action Collaborative on Clinician Resilience and Well-Being: http://ow.ly/dz8k30i1je4 #ClinicianWellBeing
![]() Tweet this! @theNAMedicine’s newest discussion paper provides a holistic view of clinician burnout and well-being, accompanied by a comprehensive conceptual model: http://ow.ly/dz8k30i1je4 #ClinicianWellBeing
Tweet this! @theNAMedicine’s newest discussion paper provides a holistic view of clinician burnout and well-being, accompanied by a comprehensive conceptual model: http://ow.ly/dz8k30i1je4 #ClinicianWellBeing
![]() Tweet this! Why are so many clinicians experiencing burnout? A new conceptual model from @theNAMedicine shines light on a multitude of factors and how they all intersect: http://ow.ly/dz8k30i1je4 #ClinicianWellBeing
Tweet this! Why are so many clinicians experiencing burnout? A new conceptual model from @theNAMedicine shines light on a multitude of factors and how they all intersect: http://ow.ly/dz8k30i1je4 #ClinicianWellBeing
Download the graphic below and share it on social media!
References
- Institute of Medicine. 2000. To Err Is Human: Building a Safer Health System. Washington, DC: The National Academies Press. https://doi.org/10.17226/9728
- Bodenheimer, T., and C. Sinsky. 2014. From triple to quadruple aim: Care of the patient requires care of the provider. Annals of Family Medicine 12(6):573-576. https://doi.org/10.1370/afm.1713
- Dyrbye, L. N., T. D. Shanafelt, C. A. Sinsky, P. F. Cipriano, J. Bhatt, A. Ommaya, C. P. West, and D. Meyers. 2017. Burnout among health care professionals: A call to explore and address this underrecognized threat to safe, high-quality care. NAM Perspectives. Discussion Paper, National Academy of Medicine, Washington, DC. https://doi.org/10.31478/201707b
- Shanafelt, T., O. Hasan, L. N. Dyrbye, C. Sinsky, D. Satele, J. Sloan, and C. P. West. 2015. Changes in burnout and satisfaction with work-life balance in physicians and the general US working population between 2011 and 2014. Mayo Clinic Proceedings 90:1600-1613. https://doi.org/10.1016/j.mayocp.2015.08.023
- Shanafelt, T. D., S. Boone, L. Tan, L. N. Dyrbye, W. Sotile, D. Satele, C. P. West, J. Sloan, and M. R. Oreskovich. 2012. Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Archives of Internal Medicine 172:1377-1385. https://doi.org/10.1001/archinternmed.2012.3199
- Parks, T. 2017. Report reveals severity of burnout by specialty. AMA Wire.
- Aiken, L. H., S. P. Clarke, D. M. Sloane, J. Sochalski, and J. H. Silber. 2002. Hospital nurse staffing and patient mortality, nurse burnout, and job dissatisfaction. JAMA 288:1987-1993. https://doi.org/10.1001/jama.288.16.1987
- McHugh, M. D., A. Kutney-Lee, J. P. Cimiotti, D. M. Sloane, and L. H. Aiken. 2011. Nurses’ widespread job dissatisfaction, burnout, and frustration with health benefits signal problems for patient care. Health Affairs 30:202-210. https://doi.org/10.1377/hlthaff.2010.0100
- Letvak, S. A. , C. J. Ruhm, and S. N. Gupta. Nurses’ presenteeism and its effects on self-reported quality of care and costs. American Journal of Nursing 112:30-388; quiz 48, 39. https://doi.org/10.1097/01.NAJ.0000411176.15696.f9
- DeWitt, B. C. (2015 November 17-18). The whole is more than the sum of its parts: Toward a conceptual map for resident wellbeing. PowerPoint presented at the 2015 ACGME Symposium on Physician Well-Being, Chicago, IL.
- Maslach, C., W. Schaufeli, and M. Lieter. Job burnout. Annual Review of Psychology 52(1):397-422. https://doi.org/10.1146/annurev.psych.52.1.397
- Perlo, J., B. Balik, S. Swensen, A. Kabcenell, J. Landsman, and D. Feeley. 2017. IHI Framework for Improving Joy in Work. IHI White Paper. Cambridge, MA: Institute for Healthcare Improvement. Available at: http://www.ihi.org/resources/Pages/IHIWhitePapers/Framework-Improving-Joy-in-Work.aspx (accessed September 1, 2020).
- Manzano-García, G., and J. C. Ayala-Calvo 2013. New perspectives: Towards an integration of the concept “burnout” and its explanatory models. Annals of Psychology 29(3):800-809. https://doi.org/10.6018/analesps.29.3.145241
- Bakker, A. B., and E. Demerouti.2017. Job demands-resources theory: Taking stock and looking forward. Journal of Occupational Health Psychology 22(3):273-285. https://doi.org/10.1037/ocp0000056
- Schaufeli, W. B., C. Maslach, and T. Marek. 2017. Professional burnout: Recent developments in theory and research. Washington, DC: Taylor and Francis.
- Hobfoll, S. E. 1989. Conservation of resources: A new attempt at conceptualizing stress. American Psychologist 44(3):513. https://doi.org/10.1037/0003-066X.44.3.513
- Siegrist, J. 1996. Adverse health effects of high-effort/low-reward conditions. Journal of Occupational Health Psychology 1(1):27. https://doi.org/10.1037/1076-8998.1.1.27
- Caplan, R. D., S. Cobb, and J. R. French. 1975. Job demands and worker health: Main effects and occupational differences. Hew Publication (NIOSH) 75: DHEW.
- Karasek, R. A. 1979. Job demands, job decision latitude, and mental strain: Implications for job redesign. Administrative Science Quarterly 24(2):285-308. Available at: https://www.jstor.org/stable/2392498 (accessed September 1, 2020).
- Demerouti, E., A. B. Bakker, F. Nachreiner, and W. B. 2001. The job demands-resources model of burnout. Journal of Applied Psychology 86(3):499-512. https://doi.org/10.1037/0021-9010.86.3.499
- Gagné, M., and E. L. Deci. 2005. Self‐determination theory and work motivation. Journal of Organizational Behavior 26(4):331-362. Available at: https://selfdeterminationtheory.org/SDT/documents/2005_GagneDeci_JOB_SDTtheory.pdf (accessed September 1, 2020).
- Kanter, R. M. 1979. Power failure in management circuits. Classics of Organization Theory, 342-351. Available at: https://hbr.org/1979/07/power-failure-in-management-circuits (accessed September 1, 2020).
- Freudenberger, H. J. 1974. Staff burn‐out. Journal of Social Issues 30(1):159-165. https://doi.org/10.1111/j.1540-4560.1974.tb00706.x
- Aiken, L. H., W. Sermeus, K. Van den Heede, D. M. Sloane, R. Busse, M. McKee, L. Bruneel, et al. 2012. Patient safety, satisfaction, and quality of hospital care: Cross sectional surveys of nurses and patients in 12 countries in Europe and the United States. British Medical Journal 344, e1717. https://doi.org/10.1136/bmj.e1717
- Rassolian, M., L. E. Peterson, B. Fang, H. C. Knight, M. R. Peabody, E. G. Baxley, and A. G. Mainous III. 2017. Workplace factors associated with burnout of family physicians. JAMA Internal Medicine 177(17):1036-1037. https://doi.org/10.1001/jamainternmed.2017.1391
- Aiken, L. H., S. P. Clarke, D. M. Sloane, E. T. Lake, and T. Cheney. 2008. Effects of hospital care environment on patient mortality and nurse outcomes. The Journal of Nursing Administration 38(5):223-229. https://doi.org/10.1097/01.NNA.0000312773.42352.d7
- Stimpfel, A. W., D. M. Sloane, and L. H. Aiken. 2012. The longer the shifts for hospital nurses, the higher the levels of burnout and patient dissatisfaction. Health Affairs 31(11): 2501-2509. https://doi.org/https://doi.org/10.1377/hlthaff.2011.1377
- Freeney, Y. M., and J. Tiernan. 2009. Exploration of the facilitators of and barriers to work engagement in nursing. International Journal of Nursing Studies 46(12):1557-1565. https://doi.org/10.1016/j.ijnurstu.2009.05.003
- Kutney-Lee, A., H. Germack, L. Hatfield, S. Kelly, P. Maguire, A. Dierkes, M. Del Guidice, and L. H. Aiken. 2016. Nurse Engagement in shared governance and patient and nurse outcomes. Journal of Nursing Administration 46(11):605-612. https://doi.org/10.1097/NNA.0000000000000412
- Leape, L., D. Berwick, C. Clancy, J. Conway, P. Gluck, J. Guest, D. Lawrence, J. Morath, D. O’Leary, P. O’Neill, D. Pinakiewicz, T. Isaac, and Lucian Leape Institute at the National Patient Safety Foundation. 2009. Transforming healthcare: A safety imperative. Quality and Safety in Health Care 18(6):424-428. https://doi.org/10.1136/qshc.2009.036954
- Halbesleben, J. R., and C. Rathert. 2008. Linking physician burnout and patient outcomes: Exploring the dyadic relationship between physicians and patients. Health Care Management Review 33(1):29-39. https://doi.org/10.1097/01.HMR.0000304493.87898.72
- Vahey, D. C., L. H. Aiken, D. M. Sloane, S. P. Clarke, and D. Vargas. 2004. Nurse burnout and patient satisfaction. Medical Care 42 (2 Supplement), 1157. https://doi.org/10.1097/01.mlr.0000109126.50398.5a
- Cimiotti, J. P., L. H. Aiken, D. M. Sloane, and E. S. Wu. 2012. Nurse staffing, burnout, and health care-associated infection. American Journal of Infection Control 40(6):486-490. https://doi.org/10.1016/j.ajic.2012.02.029
- Shanafelt, T. D., C. M. Balch, G. Bechamps, T. Russell, L. Dyrbye, D. Satele, P. Collicott, P. J. Novotny, J. Sloan, and J. Freischlag. 2010. Burnout and medical errors among American surgeons. Annals of Surgery 251(6):995-1000. https://doi.org/10.1097/SLA.0b013e3181bfdab3
- Dewa, C. S., D. Loong, S. Bonato, N. X. Thanh, and P. Jacobs. 2014. How does burnout affect physician productivity? A systematic literature review. BMC Health Services Research 14(1):325. https://doi.org/10.1186/1472-6963-14-325
- Leiter, M. P., C. Maslach. 2009. Nurse turnover: The mediating role of burnout. Journal of Nursing Management 17(3):331-339. https://doi.org/10.1111/j.1365-2834.2009.01004.x
- Noworol, C., Z. Zarczynski, M. Fafrowicz, and T. Marek. 1993. Impact of professional burnout on creativity and innovation. In Professional Burnout: Recent Developments in Theory and Research, 1st ed., edited by W. B. Schaufeli, C. Maslach, and T. Marek. Boca Raton, FL: CRC Press. Pp. 163-175.
- Coffey, D. S., K. Eliot, E. Goldblatt, C. Grus, S. P. Kishore, M. E. Mancini, R. Valachovic, and P. Hinton Walker. 2017. A Multifaceted Systems Approach to Addressing Stress Within Health Professions Education and Beyond. NAM Perspectives. Discussion Paper, National Academy of Medicine, Washington, DC. https://doi.org/10.31478/201701e