Integration of Oral Health and Primary Care: Communication, Coordination and Referral
ABSTRACT | This discussion paper focuses on some particularly challenging aspects of bridging primary care and oral health care for low health literacy populations. Because of the lack of physical proximity between most dental and medical practices, even in some co-located places, many patients and providers have difficulty navigating this divide. This discussion paper expands on three of the recommendations from a paper commissioned for the Roundtable on Health Literacy of the National Academies of Sciences, Engineering, and Medicine. The discussion paper focuses on the weak links in the integration process of communication, coordination, and referral across professions. Examples and health literacy solutions are presented, such as having personnel assist patients with navigation, electronic tools for appointments and guidance, shared electronic health records, referral guidelines, and educational curricula for health care providers to increase their interprofessional knowledge and practice. Health literacy strategies and systems are needed to establish formal communication, collaboration, and referral networks across professions at all levels. Practice-based research can advance the most effective models. Our vision is a patient-centered health home that includes bidirectional access and communication across oral health and primary care.
Introduction
Former Surgeon General C. Everett Koop is widely quoted for saying, “You’re not healthy without good oral health.” Yet in the United States, the two systems of medical and dental care are largely siloed, making it difficult for these culturally, financially, and educationally different health care professionals to work together to provide whole-person care. At the same time, the need for integration is increasingly apparent. It is estimated that each year 108 million Americans see a physician who do not see a dentist [1]. Although primary care providers routinely ask patients about their overall health, it is rare for them to ask about oral health signs and symptoms such as dry mouth, bleeding gums, and other risk factors such as chewing tobacco or family history of oral disease. Their oral examinations also may be incomplete, constituting missed opportunities for these primary care providers to engage patients in oral health education, screening, preventive strategies, and/or referral to a dental provider for treatment. Many patients who lack access to dental services seek care in hospital emergency departments where they often receive only antibiotics and pain medication without the navigation assistance to help them integrate into the primary dental care system for more definitive treatment.
Conversely, an estimated 27 million people each year have a dental visit but no medical visit [1]. Although a dentist and hygienist take a comprehensive medical history, they rarely ask their patients about preventive health behaviors such as flu shots, HPV vaccines, and mammograms, or screen for diabetes or other chronic diseases. Those without a medical visit may be more likely to have undiagnosed medical conditions that could be identified by point-of-care, chairside testing in a dental office, as increasing numbers of diseases and conditions can be identified by biomarkers present in saliva [2]. Identification of concerns or preventive gaps could then result in a referral to a primary care provider. New York State’s law requiring that dentists offer voluntary HIV screening is a first step in ensuring that preventive screening is available in a broad swath of health professionals’ offices [3].
Improved provider-to-provider and provider-to-patient communication, collaboration, referral, navigation, and feedback methods are needed as health literate interventions to assist patients trying to traverse the medical-dental divide and to provide patient-centered care. These interventions will be especially important for people with lower health literacy levels and language barriers who may have difficulty navigating our complex and fragmented health care system. Key infrastructure elements and policies are needed to alleviate this weak link in health care. Improved referral and consultation between dental and medical offices are first steps toward moving along a continuum from separate systems with little communication to a fully integrated system [4,5].
Background
Integrating the Patient-Centered Medical Home to Include Oral Health
A report issued by the Institute of Medicine in 2011 envisioned a country where everyone has access to high-quality dental care in a variety of settings [6]. Further, it concluded in one of its reports that “interprofessional, team-based care has the potential to improve care coordination, patient outcomes and produce cost savings.” Other governmental and professional bodies strongly support integration of dentistry and medicine as an important strategy to help reduce inequities in access to oral health services. In a commissioned paper for the Roundtable on Health Literacy on integration of oral health and primary health care, the authors of this NAM Perspectives paper reported that integration in the United States is in the early stages and mostly limited to pediatric populations, managed care organizations, and community clinics, leaving large segments of the population without access to comprehensive health services [7].
Oral Health in America: A Report of the Surgeon General envisioned a national partnership to reduce disparities—one that would enable individuals, health professionals, and their communities to work together to bridge the long-standing gap between medical and dental care [6]. An expanded and collaborative medical home can advance much needed bidirectional communication and coordination between all primary and specialty health care providers, hospitals or health centers, and patients [8]. Medical and dental patients share common risk factors that lead to diseases both within the mouth and the rest of the body such as tobacco and alcohol use, HIV and HPV infection, and frequent consumption of sugary foods. Social determinants of health, including economic status, social and welfare policies, and living and working environments, are common risk factors for poor overall and oral health [9,10,11]. People with many different types of expertise are needed to address these individual and societal health problems. A siloed dental profession cannot solve people’s oral health problems alone, nor can the medical profession solve general health problems alone.
To provide whole-person, integrated, patient-centered, comprehensive care, it is important to connect the mouth with the rest of the body. This need is complicated by the fact that the evolution of the dental profession occurred in isolation from other providers and health care settings. Dental care has traditionally been provided in a cottage industry of small private practices. In 2012, 80.7 percent of dental offices employed fewer than 20 people, compared with just a third of physician offices. The health care system is changing, but the changes within the dental care system lag behind medicine. From 1992 to 2012, the percentage of people employed by large dental offices with 500+ employees increased from less than 1 percent to 3.9 percent, whereas the percent of physician office employees in large, 500+ physician offices increased from 15.7 percent to 29.6 percent [12]. Few dental practices are part of large health care organizations such as Kaiser Permanente, HealthPartners, and federally qualified health centers (FQHC) where dentists and physicians practice in proximity and may share patients [13].
Integration of medicine and dentistry makes the provision of high-quality care even more challenging. It increases the number of professional types involved in people’s care. These professionals have different training, practices, and cultures, increasing the likelihood of miscommunication and misunderstandings. A lack of shared understanding and communication across professions places an unnecessary burden on patients, who are forced to navigate independent silos of care that may be inaccessible or provide only temporary care. The navigation of the two systems is particularly challenging for patients with low health literacy. As care becomes increasingly complex and dependent on collaboration and shared patient management of chronic disease, communication is of critical importance. Yet communication and referral practices remain largely untested, with few interprofessional guidelines or best practices to guide the process.
Strategies for Improving Communication, Coordination, and Referral
Communication, Referral Networks, and Risk Management
Provider and patient health literacy are critical considerations in improving provider-to-provider and provider-to-patient communication, and ultimately the health of vulnerable populations. However, even across members of the same discipline, communication and referral to other providers can be challenging. Within medical practice, one study found that in caring for 100 Medicare patients, the average primary care provider needed to coordinate care with 99 other physicians working across 53 practices [14]. A national survey of communication between primary care providers and specialists found that only 69.3 percent of primary care providers and 80.6 percent of specialists report “always” or “most of the time” sending basic patient information to each other [15].
No comprehensive national surveys are available that report referral rates between primary health care and dentistry across age groups, nor have best practices to establish multi-provider referral networks been published. State-level surveys suggest that referrals in either direction are highly variable and their effectiveness is unknown [7,16,17]. A scoping review on integrative and collaborative care models for dentistry and primary care by Gauger and colleagues [18] was restricted to those programs in which preventive services were provided and a system was in place for comprehensive dental care, either on- or off-site. Of 24 models in their review, 4 (16.6 percent) included on-site preventive services with referral to off-site dentists for comprehensive care, 13 (54.2 percent) provided on-site preventive services with minor clinical procedures such as dental sealants but off-site referral for comprehensive care, and 7 (29.2 percent) provided on-site comprehensive care. Most of the articles describe programs within FQHCs where medical and dental clinics often are co-located. Even within FQHCs, approximately 70 percent of reviewed programs required off-site comprehensive treatment.
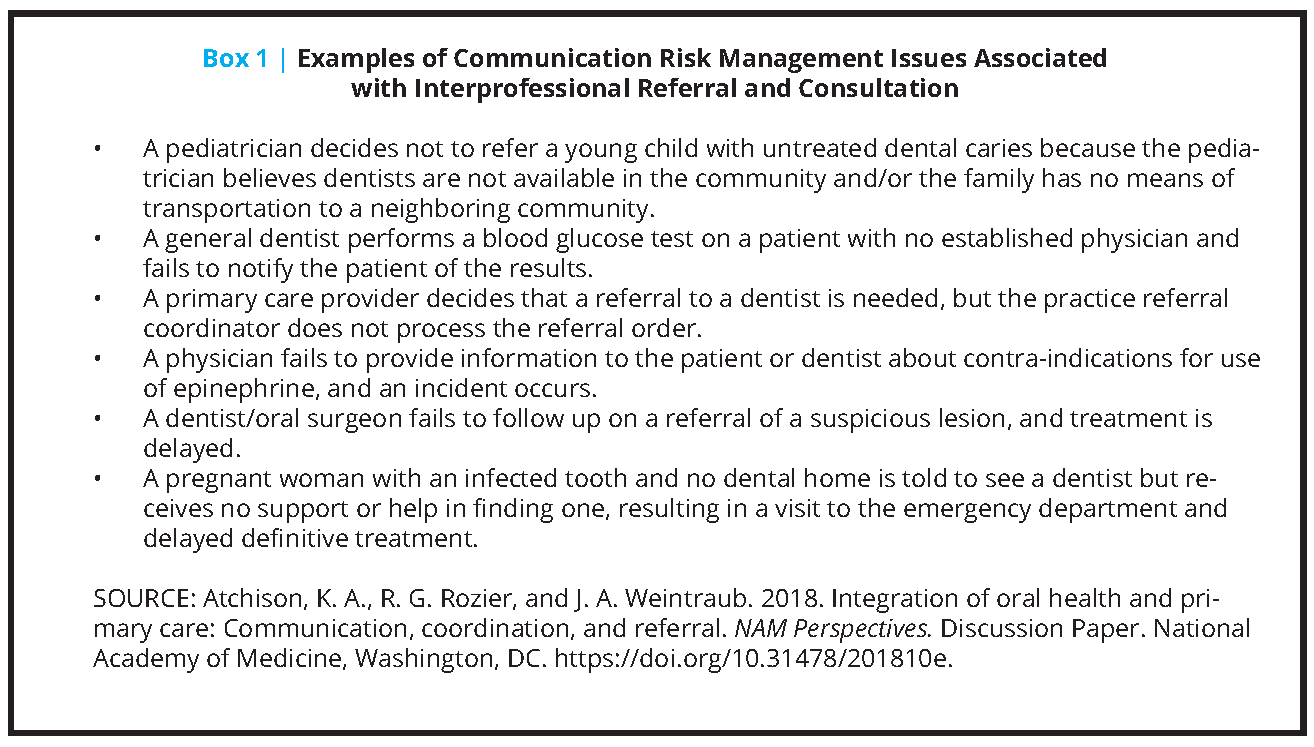
The number of referrals from primary care to dental care and vice versa is likely rising because of the increased emphasis on preventive oral health services, particularly in pediatrics, obstetrics/gynecology (OB/GYN), and chronic disease management. Because referral is an expectation and because of the challenges in communicating across providers, poor communication associated with integration of care has become a risk management concern. Communication problems are the second-most common contributing factor in malpractice claims, according to MedPro Group [19]. In an analysis of more than 23,000 medical malpractice claims and lawsuits between 2009 and 2013, CRICO Strategies identified communication failures as a risk factor in 30 percent of cases [20]. Hypothetical examples of poor quality of care associated with lack of or incomplete referral and consultation across professions are shown in Box 1.
A number of health literate interventions of care coordination, referral, or navigation were described in the commissioned paper, “Integrating Oral Health, Primary Care, and Health Literacy: Considerations for Health Professional Practice, Education, and Policy.” For example, at the Grace Health FQHC in Michigan, dental hygienists with a PA 161 permit provide prenatal oral health preventive services under indirect supervision in an OB/GYN facility as part of OB visits. If the woman is enrolled in Medicaid and does not have a dentist, the hygienist can schedule an appointment for her with the FQHC dental department and enter findings through a common electronic patient health record [7].
Other examples provided in the “Integrating Oral Health, Primary Care, and Health Literacy” describe programs of physicians’ offices that provided preventive oral health services to children 0 to 5 years of age followed by referral to a dentist [7]. Some community agencies or other providers referred at-risk children and pregnant women to participating medical and dental providers or to FQHCs. Referral programs were also found to improve patient integration and overall care for chronic disease patients, including patients with diabetes and those with HIV.
The frequency of referrals between primary health care and dental care providers is low but increasing. Communication is difficult, and efficiently functioning referral networks are uncommon. Poor communication and poor quality of care can result, raising risk management concerns. Where systems are not in place to create these networks, it is up to individual providers or professional organizations to develop these personal relationships, which is time-consuming and inefficient for the patient and the providers. To better integrate the broader health care system, including nurse practitioners, physician assistants, and others, common professional policies and practice, and communication and referral networks are required to work across professions.
Clinical Referral Guidelines and Performance Measures
Clinical guidelines and related performance measures provide important instructions on screenings to be done, services to be provided, and adherence to recommended practices. The development, dissemination, adoption, and implementation of practice guidelines are essential to support evolving quality improvement initiatives in clinical care. The high variability in reported dental referrals, low use of dental care by many population groups, and provider and patient frustration with the referral process suggest that improvements are needed in the linkage between primary health care and dental care [21,22].
Many guidelines, some targeted toward referral, have been developed for medicine and dentistry. However, most of them are for referral-related activities within the respective professions of medicine or dentistry, not specifically for physician-to-dentist coordinating, networking, and referring or vice versa. Implementation of dental referral guidelines in primary care faces a number of barriers. Some of the more commonly reported barriers to integration of oral health into primary care are lack of clinical knowledge and skills, lack of time, inadequate reimbursement, and staff buy-in [23,24,25]. More specific to dental referral, pediatric primary health care providers in North Carolina are generally aware of American Academy of Pediatrics dental referral guidelines, know which patients should be referred, and support oral health screening and risk assessment, yet they consistently under-refer, particularly if the child is at low to moderate risk for dental caries [26]. The primary obstacles to referral reported by North Carolina physicians are providers’ beliefs about the low motivation of parents to change child oral health care behaviors, their inability to motivate parents to make changes, and a shortage of dentists in some geographic areas, which leads to frustration on the part of medical providers in referring the child and the parent in obtaining dental care for the child.
A multistep referral process from primary care physicians to medical specialists has been outlined [27,28]. Despite its common practice and importance to health outcomes, only a limited number of rigorous evaluations have been conducted on interventions designed to improve the quantity and quality of referrals in primary health care. A systematic review in the Cochrane Database concluded, based on 17 studies, that the only interventions that affect primary care referral rates are “active local educational interventions involving secondary care specialists and structured referral sheets” [29].
Even less attention has been devoted to developing best practices or evidence of effectiveness for referrals between primary health care and dental care. Performance measures for monitoring the appropriateness and effectiveness of medical-dental referrals are even less well developed. The Oral Health Delivery Framework and Implementation guide supported by the National Interprofessional Initiative on Oral Health (NIIOH) and its partners prominently identified the key features of a dental referral in primary care and provided recommendations [24,30]. The framework, endorsed by 18 professional academies and organizations, defined a dental referral as a “structured” process in which “an order for a referral placed in the electronic health record (EHR) to a specific dentist . . . specifies the reason for the referral and contains relevant clinical information, including lists of the patient’s medical problems, active medications, and medication allergies. There is an expectation that the dentist will return a consultation note to the primary care team.” Field testing in 15 FQHCs and four private practices in five states found making effective dental referrals and incorporating referral information into EHRs to be among the most difficult aspects of the framework to accomplish [23].
A statewide demonstration program of the transformation of the health care system in Oregon to bring together three siloed health care systems—physical, behavioral, and dental health services—is underway [7,31]. A case study of one coordinated care organization (CCO) within the program provides insights into some of the challenges to the simple expectation of mutual referral between primary care medicine and dentistry. The mission of the CCO’s Transformation Plan included:
- developing a patient-centered primary care home;
- creating “communications, outreach, member engagement, and services tailored to cultural, health literacy, and linguistic needs” of the members;
- addressing provider deficiencies in cultural competency by training plus the use of Certified Traditional Health Workers consistent with the members’ diversity; and
- developing a system, including quality improvement plans that focus on eliminating disparities in access, quality of care, experience in care, and outcomes [7].
To summarize this section, making referrals within the same profession can be difficult. It can be even more difficult when the referral is between primary care and dental care providers who have rarely collaborated or been trained to do so. Even within one health care network like an FQHC, demonstration programs reported logistical difficulties because each clinic had different processes and sometimes lacked a shared EHR across the medical, behavioral, and dental practices. Clinical practice referral guidelines and performance measures are under development, and demonstration programs are beginning to provide insights into barriers to the successful linkage of primary health care and dental care. Attention is needed to understand and solve the challenges associated with the primary care–dental gap if integration is to be successful.
Navigation and Coordination
Navigation and coordination are important health literacy interventions, and a variety of different health care team members can provide a navigation function. Commissioned paper authors recommended a multilevel approach to integrate coordination into all levels of an organization [7]. Examples discussed in “Integrating Oral Health, Primary Care, and Health Literacy” showed that care coordination and management were needed as functional health literate messages to ensure that patients understood the need to access a different clinical setting and how to get there, to assist patients in enrolling in public programs to access dental care, and to guide patients from the emergency department to a dental practice or FQHC for appropriate treatment.
The roles, responsibilities, and classifications of patient navigators vary and include clinical assistants, case managers, community health workers or promotores de salud, and social workers. In dentistry, a new allied health professional is being trained for this role and is called a community dental health coordinator [32]. Depending on their skills, patient navigators can help increase access to care by providing assistance with scheduling appointments, following up to see if appointments are kept, explaining processes and procedures to improve care coordination, and connecting patients with social service agencies that could assist with a number of problems, such as lack of transportation or child care and understanding how to enroll in Medicaid to help access dental care. If appropriately trained and as state dental practice acts allow, navigators can provide some oral health counseling, and potentially provide oral health risk assessment, screening, and preventive services. For services in the same facility, navigators can facilitate warm handoffs among providers and introduce patients to new providers, alleviate concerns, and help build relationships.
The patient-centered medical home initiative requires that each patient have a primary care provider. This individual leads the team of all clinical care professionals to provide comprehensive, coordinated health care to the patient [33]. Patient-centered medical home standards include the use of linguistically and culturally appropriate services, care planning, referral to community resources, referral tracking, and coordination of care for all provider transitions. The patient-centered medical home initiative and the Joint Commission, the accrediting organization for US health care organizations, both endorse system-level application of low health literate patient information and processes for patients to navigate the health care organization [34]. Patient-centered medical homes have been proposed by both medical and dental professionals [33,35,36].
Electronic Tools and Integrated Patient Health Records
Electronic tools can be helpful health literate interventions that enable providers to share information and for patients to be referred from one provider to another. “Integrating Oral Health, Primary Care, and Health Literacy” provided examples where technology was incorporated into clinical care to convey health literate messages to patients and providers to improve the quality of care [7]. For example, prompts within the EHR are used to guide a provider on how and when to use anticipatory guidance and to produce preventive reports to enable dental providers to look for care gaps [7,37]. Patient portals are also to provide oral health education materials and after-visit summaries. A case study included in “Integrating Oral Health, Primary Care, and Health Literacy” discussed how a CCO in Oregon worked with the dental practices in their network to connect the dentists to the prescription drug monitoring program so the dentists could more knowledgably manage their patients’ prescription drug use [7].
Integrated EHRs have become commonplace in medicine but less so in dentistry. Bringing more dental software companies to meaningful use and the ability to share with medical electronic systems is needed. In integrated systems such as Kaiser Permanente, medical and dental electronic records can be shared among the patient’s clinicians and updated with current medical histories, medications, and treatment to avoid errors caused by multiple tests or medications [13]. When appointment scheduling is built into the system, referrals and requests for consultation between medicine and dentistry are much easier. Feedback to the referring clinician also becomes easier. In the absence of a shared record, communicating between providers, or between a provider and a patient, is challenging, requiring tracking mechanisms, and carries the risk of lost documentation and lack of both patient and provider follow-up.
Integrated—or at least compatible and interoperable—health record systems can help to improve communication between provider types. Their use is growing in managed care organizations but lags in private practice. Some states are calling for health information exchanges (HIE) that can provide secure transmission of health care-related data, in response to a federal requirement for Centers for Medicare & Medicaid Services-eligible providers to use a secure electronic method when patients are being referred from one provider to another [38,39,40]. Expanded use of HIE could begin to bring better electronic communication between private practices and managed care, FQHCs, and other practice types.
Interprofessional Education and Collaborative Practice
In “Integrating Oral Health, Primary Care, and Health Literacy,” the authors of this paper [7] described how pre-licensure and post-licensure health professionals are learning about each other’s disciplines and preparing to work together [7]. Interprofessional education (IPE) is now part of academic program accreditation standards. IPE is a prelude to interprofessional collaborative practice (IPCP), although because this is relatively new, there is little information about the extent to which IPE translates into IPCP, or the outcomes of such integration on patient care [41,42,43]. Both the NIIOH and the American Dental Education Association (ADEA) have been national leaders in promoting integration and the inclusion of oral health in IPE activities.
Academic institutions are responsible for preparing the clinicians of the future. Dental school students and faculty are dental safety net providers, providing care for people with diverse backgrounds who lack access to dental services, whether because of economics, lack of dental insurance, or residing in a dental health professional shortage area [44]. Many of these patients may have low health literacy levels and other health care and social service needs. Schools should ensure that students gain experience during their education in effective communication practices for patients with low health literacy and in learning to make and respond to referrals to and from other types of health and social service professionals. A collaboration between the Harvard School of Dental Medicine and Northeastern University resulted in a manual to promote collaborative practice between dentists and nurse practitioners [45].
The Commission on Dental Accreditation standards are designed to ensure that dental students participate in IPE and understand the social determinants of health and factors associated with disparities in vulnerable populations. Data from the ADEA 2017 annual Senior Survey show that 90 percent of graduating seniors think they were prepared or well prepared in IPE and for working with other professions. Eighty-four percent indicated they thought they were prepared/well prepared for integrating oral health with medical care [46]. Regardless of the high perceived competence, some of the interactions occur in shared classes, case discussions, simulated patients, or extracurricular activities that do not involve direct interprofessional collaborative patient care. However, in many schools, students spend part of their time outside the dental school on rotations providing dental care in other health care settings, such as FQHCs. Although small proportions of practicing dentists are currently in these settings, incorporating partnerships between academic dental institutions and FQHCs is pivotal in building the pipeline of new dentists practicing in team-based care settings through externships and dental residency rotations [47].
Continuing education (CE), particularly integrated CE targeted at medical and dental audiences together, is rare, and little is found about training on referral and consultation across the medical-dental divide [7]. Integrated CE is needed because most practitioners are removed from their initial professional education and were not likely to have been exposed to IPE during training. The long-term goal is to move along the pathway from provider education to changing provider behavior to improving patient care delivery and ultimately improving patient health. The Interprofessional Education Collaborative presents one model of education for health professions faculty engaged with their clinical partners that provides guided learning, team-based planning activities, and consultation with experts and peers [48].
The NIIOH provides backbone support to a consortium of funders, health professionals, and national organizations focused on the integration of oral health in primary care. The NIIOH works to build a shared culture across the professions to ensure that all patients have access to oral health services and referrals within the context of their primary care. NIIOH activities are organized around core strategies to cultivate leaders, facilitate interprofessional training, and develop resources to increase professionals’ understanding, knowledge, and skills. One of these resources is Smiles for Life, a national oral health curriculum created in 2005 by the Society of Teachers of Family Medicine Group on Oral Health [49]. Now in its third edition, Smiles for Life is free and online. Continuing education credit for this program is available for many health professionals. More than 250,000 courses had been completed for CE credit by registered users as of June 12, 2018.
The Health Resources and Services Administration (HRSA)’s Integration of Oral Health and Primary Care Practice initiative developed a “core set of oral health care clinical competencies for primary care providers who practice in safety net settings” [50]. These competencies consist of five domains: risk assessment, oral health evaluation, preventive interventions, communication and education, and interprofessional collaborative practice (IPCP). HRSA made education and continuing education recommendations for implementation [51]. Needed infrastructure identified for the IPCP domains included interoperable electronic health records and other communication and collaboration pathways to exchange patient information, appropriate referral systems, and facilitation of patient navigation.
Research and Demonstration Programs
Demonstration programs on integration of oral health and primary care are increasingly found in the gray and peer-reviewed literature. Little outcomes research has been published to guide the profession in assembling an efficient and effective integrated medical-dental health system, including referral networks, referral behaviors and outcomes, performance standards, and consultation between provider types. Limited research studying the primary care–dental referral process exists in the literature, particularly the interface between primary health care and private dental offices. Two initiatives developed guidance about the process and challenges related to oral health integration.
The National Network for Oral Health Access pilot tested the clinical competencies for interprofessional collaboration developed by HRSA in three community health centers [51]. A resulting implementation guide provides general recommendations on strategies to improve interaction between medical and dental systems. Primary barriers to successful referrals in these health centers even with co-located dental clinics were the lack of interoperability among the medical and dental EHRs, which made it difficult to track referrals; low motivation of patients who lacked understanding of the need for the referral to the dental clinic, coupled with a lack of educational materials in the primary care clinics to educate patients on the reason for the referral; and lack of the dental clinics’ capacity to accommodate the referrals made to the clinic.
The Oral Health Delivery Framework [30] describes five activities that a primary care team can take to protect and promote oral health: Ask, Look, Decide, Act, and Document & Follow-Up. This key demonstration program was pilot-tested in 19 primary care locations, resulting in guidance on how to implement the framework in a variety of workplace settings. They further developed the process and the components for a structured referral, how to develop a referral network, and appropriate quality improvement measures for such integration (such as the number of referral agreements in place and percentage of referred patients with a completed dental referral). The initiative laid the groundwork for future outcomes research.
Medical and Dental Practice Based Research Networks (PBRN) developed across the 50 states offer an opportunity to elucidate the challenges of integrated primary care and to develop and test an efficient mechanism for referral of patients between medicine and dentistry. The Dental PBRN has a unique role in recruiting, training, and implementing practice-based research among dentists in private practice, both fee-for-service and managed care. The Dental PBRN investigated medical screening for blood glucose testing in the dental practice followed by a one-way letter of patient results to the physician [52]. Numerous primary care medical PBRNs conduct community-based quality improvement and evidence-based research. Although the medical and dental PBRNs have not yet worked together on a study, capitalizing on these research networks could be one way to develop and test efficient referral mechanisms.
The Center for Medicare & Medicaid Innovation launched a comprehensive review of primary care in 2012 with a goal of improving the primary care delivery system, health care quality, the patient experience, and ways to lower cost [53]. Five delivery functions were measured in the study of more than 2,000 clinicians serving 3 million patients. The five key functions of integrated primary care practice were access and continuity, planned care for chronic conditions and preventive care, risk-stratified care management, patient and caregiver engagement, and coordination of care across the medical neighborhood. Oral health was not included in this important Comprehensive Primary Care Initiative, representing a missed opportunity to explore the communication, coordination, and referral aspects described in this discussion paper.
Practice-based outcomes research assessing the effect of the integration of oral health and primary care is much needed to determine the most effective and efficient process for improving access to preventive services across the lifespan, to improve medical and dental outcomes, and to assess whether an integrated health care system can achieve the goals of improved care, improved patient experience, and reduced cost for the US health care system. Ultimately communication, coordination, and referral between the medical and dental systems will be required to achieve these goals.
Recommendations and Conclusion
There is an enormous need for the health care professions to develop and implement a system integrating medicine and dentistry, recognizing that physical proximity of practices is unlikely to be the norm for many years to come. The lack of, or a poorly conducted, consultation and referral process leads to risk management issues and is potentially contributing to poor health outcomes that simultaneously drive up health care costs.
The use of strategies for low health literate populations such as those reported in the commissioned paper and described in this discussion paper that promote interprofessional communication, coordination, and referral should be encouraged by the professional organizations and academic medical centers. Implementation of these strategies should be closely monitored and research conducted on these efforts to identify and advance the most effective integration models. Ultimately, improved communication among providers and between providers and patients will benefit all participants in the health care process.
The commissioned paper includes a number of recommendations regarding the recurring needs for communication, collaboration, and referral as examples of the health literacy needs for successful medical-dental integration. Specifically, these recommendations for action and research include recognizing:
- the importance of incorporating oral health literacy principles into all levels of a health care organization;
- the need to explore the best ways to establish formal collaboration and referral networks among health care systems, medical practices, and dental practices within local regions; and
- the importance of conducting research and demonstration programs on the integration of oral health into primary care and the development of effective linkages between primary care teams and dentists in private practices.
Until sometime in the future when a greater proportion of dental practices is incorporated into large health care settings, it is imperative to build on the ways the profession has developed to connect these two siloed systems of care so that patient care can be improved, particularly for vulnerable, low literacy populations. Ultimately, practice-based research that includes medical and dental professions will confirm the best models for communication, coordination, and referral within the expanded patient-centered health home.
Join the conversation!
![]() Tweet this! Patient-centered care must connect the mouth with the rest of the body. A new #NAMPerspectives discussion paper explores how to best bridge primary care with dental care: https://doi.org/10.31478/201810e
Tweet this! Patient-centered care must connect the mouth with the rest of the body. A new #NAMPerspectives discussion paper explores how to best bridge primary care with dental care: https://doi.org/10.31478/201810e
![]() Tweet this! Dental care is often left out of a preventative care strategy, especially for patients with low health literacy. Authors illuminate how clinicians can help ensure whole-person health for their patients: https://doi.org/10.31478/201810e #NAMPerspectives
Tweet this! Dental care is often left out of a preventative care strategy, especially for patients with low health literacy. Authors illuminate how clinicians can help ensure whole-person health for their patients: https://doi.org/10.31478/201810e #NAMPerspectives
![]() Tweet this! Electronic health records that incorporate all aspects of a patient’s care, including dental visits, are critical to assisting those with low health literacy navigate an increasingly complex health care system: https://doi.org/10.31478/201810e #NAMPerspectives
Tweet this! Electronic health records that incorporate all aspects of a patient’s care, including dental visits, are critical to assisting those with low health literacy navigate an increasingly complex health care system: https://doi.org/10.31478/201810e #NAMPerspectives
Download the graphics below and share them on social media!
References
- Vujicic, M., H. Israelson, J. Antoon, R. Kiesling, T. Paumier, and M. Zust. 2014. A profession in transition. Guest editorial. Journal of the American Dental Association 145(2):118-121. https://doi.org/10.14219/jada.2013.40
- Khan, R. S., Z. Khurshid, and F. Yahya Ibrahim Asiri. 2017. Advancing point-of-care (PoC) testing using human saliva as liquid biopsy. Diagnostics 7(3):E39. https://doi.org/10.3390/diagnostics7030039
- New York State Department of Health. 2012. Chapter 308 of the laws of 2010, HIV testing law, mandated report, August 2012. Available at: https://www.health.ny.gov/diseases/aids/providers/testing/law/docs/chapter_308.pdf (accessed June 13, 2018).
- Doherty, W. 1995. The whys and levels of collaborative family health care. Family Systems Medicine 13(3-4):275-281. http://dx.doi.org/doi:10.1037/h0089174
- Collins, C., D. L. Heuson, R. Munger, and T. Wade. 2010. Evolving models of behavioral health integration in primary care. New York: Milbank Memorial Fund. Available at: https://www.milbank.org/wp-content/uploads/2016/04/EvolvingCare.pdf (accessed June 12, 2018).
- Institute of Medicine. 2011. Improving access to oral health care for vulnerable and underserved populations. Washington, DC: The National Academies Press. https://doi.org/10.17226/13116
- Atchison, K. A., R. G. Rozier, and J. A. Weintraub. 2017. Integrating oral health, primary care, and health literacy: Considerations for health professional practice, education and policy. Commissioned by the Roundtable on Health Literacy, Health and Medicine Division, the National Academies of Sciences, Engineering, and Medicine,. Available at: http://nationalacademies.org/hmd/~/media/Files/Activity%20Files/PublicHealth/HealthLiteracy/Commissioned%20Papers%20-Updated%202017/Atchison%20K%20et%20al%202017%20Integrating%20oral%20health%20primary%20care%20and%20health%20literacy.pdf (accessed February 23, 2018).
- Taylor, E. F., T. Lake, J. Nysenbaum, G. Peterson, and D. Meyers. 2011. Coordinating care in the medical neighborhood: Critical components and available mechanisms. White paper (prepared by Mathematica Policy Research under Contract No. HHSA290200900019I TO2). AHRQ Publication No. 11-0064. Rockville, MD: Agency for Healthcare Research and Quality. Available at: https://pcmh.ahrq.gov/page/coordinating-care-medical-neighborhood-critical-components-and-available-mechanisms (accessed September 2, 2020).
- Sheiham, A., and R. G. Watt. 2000. The common risk factor approach: A rational basis for promoting oral health. Community Dentistry and Oral Epidemiololgy 28:399-406. https://doi.org/10.1034/j.1600-0528.2000.028006399.x
- Tiwari, T. 2018. Social determinants of health: An essential element in dental education. Journal of Dental Education 82(3)235-236. https://doi.org/10.21815/JDE.018.021
- Watt, R. G., and A. Sheiham. 2012. Integrating the common risk factor approach into a social determinants framework. Community Dentistry and Oral Epidemiology 40(4):289-296. https://doi.org/10.1111/j.1600-0528.2012.00680.x
- Guay, A., and T. Wall. 2016. Considering large group practices as a vehicle for consolidation in dentistry. Health Policy Institute research brief. American Dental Association. Available at: http://www.ada.org/~/media/ADA/Science%20and%20Research/HPI/Files/HPIBrief_0416_1.pdf (accessed June 13, 2018).
- Jones, J. A., J. J. Snyder, D. S. Gesko, and M. J. Helgeson. 2017. Integrated medical-dental delivery systems: Models in a changing environment and their implications for dental education. Journal of Dental Education 81(9):eS21-eS29. https://doi.org/10.21815/JDE.017.029
- Pham, H. H., A. A. O’Malley, P. B. Bach, C. Salontz-Martinez, and D. Schrag. 2009. Primary care physicians’ links to other physicians through Medicare patients: The scope of care coordination. Annals of Internal Medicine 150(4):236-242. https://doi.org/10.7326/0003-4819-150-4-200902170-00004
- O’Malley, A. S., and J. D. Reschovsky. 2011. Referral and consultation communication between primary care and specialist physicians: Finding common ground. Archives of Internal Medicine 171(1):56-65. https://doi.org/10.1001/archinternmed.2010.480
- Moyer, V. A., and US Preventive Services Task Force. 2014. Prevention of dental caries in children from birth through age 5 years: US Preventive Services Task Force recommendation statement. Pediatrics 133(6):1102-1111. https://doi.org/10.1542/peds.2014-0483
- American Academy of Family Physicians. 2017. Summary of recommendations for clinical preventive services. Available at: https://www.aafp.org/dam/AAFP/documents/patient_care/clinical_recommendations/cps-recommendations.pdf (accessed June 11, 2018).
- Gauger, T. L., L. A. Prosser, M. Fontana, and P. J. Polverini. 2018. Integrative and collaborative care models between pediatric oral health and primary care providers: A scoping review of the literature. Journal of Public Health Dentistry. https:/doi.org/10.1111/jphd.12267
- Cascella, L. M. Close encounters of the diagnostic kind: Improving provider–patient communication during the diagnostic process. MedPro Group. https://www.medpro.com/provider-patient-encounter-dxerrors (accessed October 1, 2018).
- CRICO Strategies. 2015. Malpractice risks in communication failures. Annual Benchmarking Report. Available at: https://www.rmf.harvard.edu/Malpractice-Data/Annual-Benchmark-Reports/Risks-in-Communication-Failures (accessed June 29, 2018).
- Meyer, B. D., J. Y. Lee, L. N. Lampiris, P. Mihas, S. Vossers, and K. Divaris. 2017. “They told me to take him somewhere else”: Caregivers’ experiences seeking emergency dental care for their children. Pediatric Dentistry 39(3):209-214. Available at: https://pubmed.ncbi.nlm.nih.gov/28583245/ (accessed September 2, 2020).
- Miloro, M. B., and M. Vujicic. 2016. Physicians dissatisfied with current referral process to dentists. Health Policy Institute, American Dental Association. Available at: https://www.ada.org/~/media/ADA/Science%20and%20Research/HPI/Files/HPIBrief_0316_5.pdf?la=en (accessed June 13, 2018).
- Safety Net Medical Home Initiative. 2016. Implementation guide supplement. Organized, evidence-based care: Oral health integration. Available at: http://www.safetynetmedicalhome.org/sites/default/files/Guide-Oral-Health-Integration.pdf (accessed April 30, 2018).
- Phillips, K. E., and J. Hummel. 2016. Oral health in primary care: A framework for action. JDR Clinical & Translational Research 1(1):6-9. Available at: http://journals.sagepub.com/doi/full/10.1177/2380084415625634 (accessed June 13, 2018).
- Harnagea, H., Y. Couturier, R. Shrivastava, F. Girard, L. Lamothe, C. P. Bedos, and E. Emami. 2017. Barriers and facilitators in the integration of oral health into primary care: A scoping review. BMJ Open 7(9):e016078. https://doi.org/10.1136/bmjopen-2017-016078
- Zhu, Y., K. Close, L. Zeldin, R. B. Quinonez, B. A. White, and R. G. Rozier. 2018. A clinical vignette-based study of physicians’ adherence to guidelines for dental referrals of young children. Academic Pediatrics. https://doi.org/10.1177/2380084418810332
- Mehrotra, A., C. B. Forrest, and C. Y. Lin. 2011. Dropping the baton: Specialty referrals in the United States. Milbank Quarterly 89(1):39-68. https://doi.org/10.1111/j.1468-0009.2011.00619.x
- Forrest, C. B. 2009. A typology of specialists’ clinical roles. Archives of Internal Medicine 8;169(11):1062-1068. https://doi.org/10.1001/archinternmed.2009.114
- Akbari, A., A. Mayhew, M. A. Al-Alawi, J. Grimshaw, R. Winkens, E. Glidewell, C. Pritchard, R. Thomas, and C. Fraser. 2008. Interventions to improve outpatient referrals from primary care to secondary care. Cochrane Database of Systematic Reviews (4):CD005471. https://doi.org/10.1002/14651858.CD005471.pub2
- Hummel, J., K. E. Phillips, B. Holt, and C. Hayes. 2015. Oral health: An essential component of primary care. Seattle, WA: Qualis Health. White paper commissioned by the National Interprofessional Initiative on Health. Available at: http://www.safetynetmedicalhome.org/sites/default/files/White-Paper-Oral-Health-Primary-Care.pdf (accessed March 15, 2018).
- Health Management Associates. 2016. Oral health integration in Oregon: Environmental scan & recommendations. Available at: https://www.oregon.gov/oha/HPA/CSI-TC/Resources/Oral%20Health%20Integration%20in%20Oregon%20-%20Environmental%20Scan%20and%20Recommendations.pdf (accessed June 28, 2017).
- Grover, J. 2017. Community dental health coordinators: Cultural “connectors” for oral health. North Carolina Medical Journal 78(6):383-385. Available at: https://www.ncmedicaljournal.com/content/ncm/78/6/383.full.pdf (accessed September 2, 2020).
- American Academy of Family Physicians. 2007. Joint principles of the patient-centered medical home. Available at: http://aafp.org/dam/AAFP/documents/practice_management/pcmh/initiatives/PCMHJoint.pdf (accessed June 8, 2018).
- Agency for Healthcare Research and Quality. 2015. Using health literacy tools to meet PCMH standards. Available at: https://www.ahrq.gov/sites/default/files/wysiwyg/professionals/quality-patient-safety/quality-resources/tools/literacy-toolkit/pcmh-crosswalk.pdf (accessed June 7, 2018).
- Damiano, P. C., J. C. Reynolds, S. C. McKernan, S. Mani, and R. A. Kuthy. 2015. The need for defining a patient-centered dental home model in the era of the Affordable Care Act. Iowa City, IA: University of Iowa Public Policy Center. Available at: http://ppc.uiowa.edu/sites/default/files/pchdjul2015.pdf (accessed June 13, 2018).
- Girish Babu, K. L., and G. M. Doddamani. 2012. Dental home: Patient centered dentistry. Journal of International Society of Preventive & Community Dentistry 2(1):8-12. https://doi.org/10.4103/2231-0762.103448
- Mosen D., D. Pihlstrom, J. Snyder, N. Smith, E. Shuster, and K. Rust. Association of dental care with adherence to HEDIS measures. Permanente Journal 2016;20(1):33-40. https://doi.org/10.7812/TPP/15-075
- Centers for Medicare & Medicaid Services. 2016. EHR incentive programs in 2015 through 2017 health information exchange. Available at: https://www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms/Downloads/2016_HealthInformationExchange.pdf (accessed May 11, 2018).
- NC Health Information Exchange Authority. 2018. About the NC HIEA. Available at: https://hiea.nc.gov/about-us/about-nc-hiea (accessed May 12, 2018).
- Burris, C. 2017. Connecting oral and physical health via the Health Information Exchange. North Carolina Medical Journal 78(6):410-412. https://doi.org/10.18043/ncm.78.6.410
- Reeves, S., L. Perrier, J. Goldman, D. Freeth, and M. Zwarenstein. 2013. Interprofessional education: Effects on professional practice and healthcare outcomes (update). Cochrane Database of Systematic Reviews (3):CD002213. https://doi.org/10.1002/14651858.CD002213.pub3
- Brandt, B., M. N. Lutfiyya, J. A. King, and C. Chioreso. 2014. A scoping review of interprofessional collaborative practice and education using the lens of the Triple Aim. Journal of Interprofessional Care 28(5):393-399. https://doi.org/10.3109/13561820.2014.906391
- Lutfiyya, M. N., B. F. Brandt, and F. Cerra. 2016. Reflections from the intersection of health professions education and clinical practice: The state of the science of interprofessional education and collaborative practice. Academic Medicine 91(6):766-771. https://doi.org/10.1097/ACM.0000000000001139
- Contreras, O. A., D. Stewart, and R. W. Valachovic. 2018. Examining America’s dental safety net. American Dental Education Association. Available at: http://www.adea.org/policy/white-papers/Dental-Safety-Net.aspx (accessed July 19, 2018).
- Dolce, M. C., J. L. Parker, and J. D. Da Silva. 2018. Nurse practitioner & dentist model for primary care: A guide for implementing collaborative care in U.S. dental schools. Boston, MA: Harvard School of Dental Medicine and Northeastern University. Available at: http://www.northeastern.edu/npd/assets/uploads/2018/02/npd-model-implementation-guide.pdf (accessed June 12, 2018).
- Wanchek, T., B. J. Cook, and R. W. Valachovic. 2018. Annual ADEA survey of dental school seniors: 2017 graduating class. Journal of Dental Education 82(5):613-630. https://doi.org/10.21815/JDE.018.059
- Langelier, M., J. Moore, B. K. Baker, and E. Mertz. 2015. Case studies of 8 federally qualified health centers: Strategies to integrate oral health with primary care. Rensselaer, NY: Center for Health Workforce Studies, School of Public Health, SUNY Albany. Available at: http://www.oralhealthworkforce.org/wp-content/uploads/2015/11/FQHC-Case-Studies-2015.pdf (accessed June 27, 2017).
- Interprofessional Education Collaborative. 2018. 2018 Fall Institute About Page. Available at: https://www.ipecollaborative.org/2018-fall-institute.html (accessed June 29, 2018).
- Clark, M. B., A. B. Douglass, R. Maier, M. Deutchman, J. M. Douglass, W. Gonsalves, H. Silk, J. W. Tysinger, A. S. Wrightson, R. Quinonez, M. Dolce, and J. Bowser. 2010. Smiles for Life: A National Oral Health Curriculum. 3rd ed. Society of Teachers of Family Medicine. Available at: http://smilesforlifeoralhealth.com (accessed July 30, 2018).
- Health Resources and Services Administration. 2014. Integration of oral health and primary care practice. U.S. Department of Health and Human Services. Available at: https://www.hrsa.gov/sites/default/files/hrsa/oralhealth/integrationoforalhealth.pdf (accessed February 23, 2018).
- National Network for Oral Health Access. 2015. A user’s guide for implementation of interprofessional oral health care clinical competencies: Results of a pilot program. Denver, CO: NNOHA. Available at: http://www.nnoha.org/nnoha-contents/uploads/2015/01/IPOHCCC-Users-Guide-Final_01-23-2015.pdf (accessed June 12, 2017).
- Barasch, A. M. M. Safford, V. Qvist, R. Pallmore, D. Gesko, and G. H. Gilbert. 2012. Random blood glucose testing in dental practice. Journal of the American Dental Association 143(3):262-269. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3296288/ (accessed September 2, 2020).
- Mathematica Policy Research. 2018. Evaluation of the comprehensive primary care initiative. Fourth annual report. Available at: https://www.mathematica-mpr.com/our-publications-and-findings/projects/evaluation-of-the-comprehensive-primary-care-initiative (accessed June 12, 2018).