Implementing Optimal Team-Based Care to Reduce Clinician Burnout
Introduction
Team-based health care has been linked to improved patient outcomes and may also be a means to improve clinician well-being [1]. The increasingly fragmented and complex health care landscape adds urgency to the need to foster effective team-based care to improve both the patient and team’s experience of care delivery. This paper describes key features of successful health care teams, reviews existing evidence that links high-functioning teams to increased clinician well-being, and recommends strategies to overcome key environmental and organizational barriers to optimal team-based care in order to promote clinician and patient well-being.
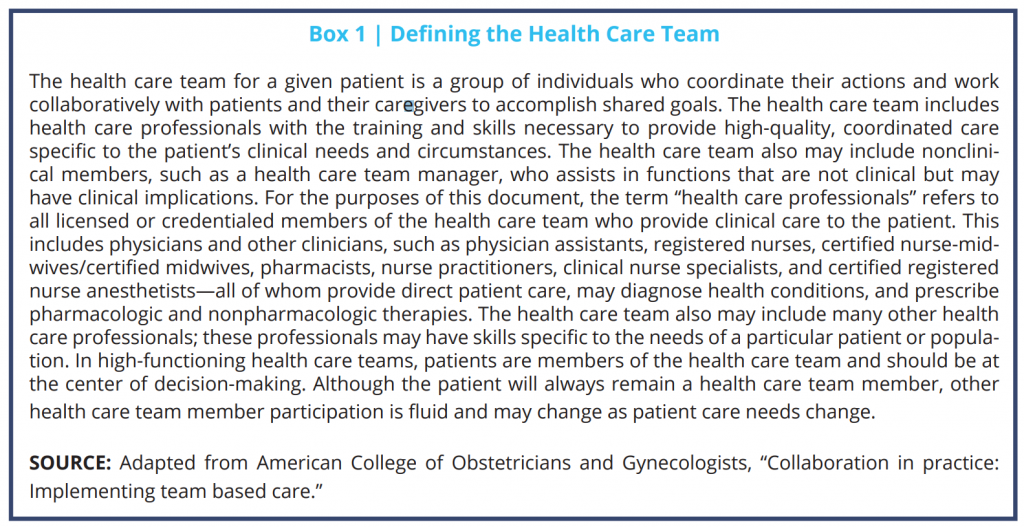
What Is a Health Care Team?
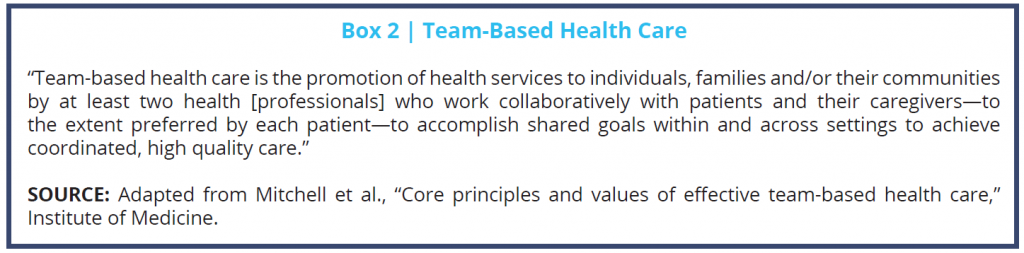
We begin by asking a simple question: what is a health care team? Health care teams have been defined in previous literature as two or more health care professionals who work collaboratively with patients and their caregivers to accomplish shared goals [2,3]. However, a health care team may involve a wide range of team members in various settings. Examples include a small, office-based team consisting of a primary care clinician with one or two medical assistants or a hospital-based trauma team with a dozen members. In addition to patients and their support groups, potential members include physicians, nurses, pharmacists, social workers, trainees, and others identified as persons necessary to help achieve shared goals. The fundamental concept is that a team is a group of individuals who coordinate their actions for a common purpose, which in health care is the prevention or treatment of disease and the promotion of health. A team-based model of care strives to meet patient needs and preferences by actively engaging patients as full participants in their care, while encouraging all health care professionals to function to the full extent of their education, certification, and experience [4].
Successful teamwork has four key characteristics: (1) a clear and compelling purpose or goal, (2) an enabling social structure that facilitates teamwork, (3) a supportive organizational context, and (4) expert teamwork coaching [5]. Effective teamwork depends on (1) the team members’ psychological safety, defined as their ability to trust one another and feel safe enough within the team to admit a mistake, ask a question, offer new data, or try a new skill without fear of embarrassment or punishment, and (2) allows team members to learn, teach, communicate, reason, think together, and achieve shared goals, irrespective of their individual positions or status outside the team [6].
There is growing recognition of the importance of team-based care in today’s changing and increasingly complex health care delivery system. In particular, the shift from fee-for-service (FFS) payment to value-based payment models (which reward providers for the quality of care provided) highlights the importance of a team approach to improve the health of individuals and populations, and to improve the safety, quality, and efficiency of health care delivery [4]. Many emerging value-based payment models facilitate closer integration and alignment of health care team members through coordinated payments and accountable care. Moreover, a team-based approach is especially important when caring for patients with complex care needs. To understand the critical need for team-based care, consider that a typical Medicare beneficiary visits two primary care clinicians and five secondary (i.e., subspecialty) care clinicians per year [3], as well as health care professionals who provide diagnostic, pharmacy, and other services. This number is several times larger for people with multiple chronic conditions. To manage the large amounts of information and multiple handoffs inherent in caring for complex patients, there is a need for seamless communication and transitions among health care professionals (within a team or among teams) [4].
The Effects of Health Care Teams on Patients and Team Members
To be effective, teamwork must enhance “the capability of members to work together interdependently in the future” and must contribute “to the growth and personal well-being of team members” [7]. In this sense, then, a health care team will achieve both clinical goals for patients and personal goals for team members when it functions well.
According to the Agency for Healthcare Research in Quality (AHRQ), “the primary goal of medical teamwork is to optimize the timely and effective use of information, skills, and resources by teams of health care professionals for the purpose of enhancing the quality and safety of patient care” [8]. Despite some variation in the literature, there is strong evidence in support of team-based care. The evidence that connects optimal teamwork and improved patient outcomes is promising and includes studies in various settings, including ambulatory, emergency department, nursing home, and hospital-based care (intensive care units (ICUs), wards, and operating rooms) [9,10,11]. For example, a 2015 review of 52 studies of team-based care for hypertension found that teams achieved controlled blood pressure in 12 percent more patients than routine care did [12]. Another study found that a novel team-based model that includes new standard work (e.g., proactive patient outreach, pre-visit schedule grooming, depression screening, care planning, and health coaching) improved patients’ self-management of hypertension and diabetes. In particular, patients experienced a decline in diastolic blood pressure and improved glycemic control over the first six months [13]. A multidisciplinary team-based care approach has also been shown to improve survival outcomes in high-risk neuroblastoma patients [14].
There is also evidence that multidisciplinary team-based care is associated with better performance on traditional measures of health care quality, such as emergency department utilization and hospital readmissions. In addition, several studies have concluded that optimizing team-based care is a cost-effective intervention [15,16]. A literature review examined teamwork in operating rooms, ICUs, emergency medicine, and trauma/resuscitation teams, focusing on quality and patient safety. The review revealed that teamwork played an important role in preventing adverse events, and it showed a relationship between staff perception of teamwork and attitudes about the importance of quality and patient safety [17]. One study found that multidisciplinary team-based care for patients with lung cancer was associated with significantly fewer emergency department visits [18]. Additionally, a care model that works in collaboration with primary care clinicians and patient-centered medical homes to provide home-based geriatric care management was associated with 7.1 percent fewer emergency department visits, 14.8 percent fewer 30-day readmissions, 37.9 percent fewer hospital admissions, and 28.5 percent fewer total bed days of care, saving an estimated $200,000 per year after accounting for program costs [19]. Primary care teams that exhibit a higher density of daily interaction and lower centralization were associated with better clinical outcomes and lower medical costs for patients with cardiovascular disease [20].
However, the relationship between high-quality, team-based health care and clinician burnout is less well defined in the literature; few studies have investigated the interplay among teamwork, patient outcomes, and clinician well-being [1,21]. Most of the available evidence is from cross-sectional, single-institutional, or brief observational studies that make causality difficult to ascertain.
Nevertheless, the existing evidence demonstrates a generally positive association between team-based care and clinician well-being. A methodologically sound, longitudinal study of interprofessional teams in the ICU setting found a connection between measures of high-quality teamwork and measures of clinician well-being and resilience. The study concluded that addressing clinician emotional exhaustion is an important prerequisite to effective team-based care and patient safety [1]. Another study explored the relationship among team structure, team culture, and emotional exhaustion in interprofessional teams and found that team culture was more predictive of clinician emotional exhaustion than team structure [22]. Similarly, another study found that perceptions of better team culture, alone and in combination with tight team structure, were associated with lower clinician exhaustion [23]. A small study of 106 Canadian air medical personnel found that both perceived control over one’s job and team efficacy buffered some of the workplace stressors identified by the researchers, including risk perception, worries over medical hassles, and barriers to patient care [24]. A larger survey-based study of over 500 physicians in Taiwan supported the hypothesis that a positive team climate may mitigate physician burnout [25]. Teamwork has been found to partially mitigate the relationship between work demands and burnout and fully mitigate the job engagement–job satisfaction relationship in a large study using a set of valid survey instruments and regression models [26]. The study found that higher work demands or the other physical, psychological, social, or organizational factors that require prolonged physical and/or psychological efforts from workers predicted higher burnout levels. However, teamwork was related to lower levels of burnout. Additionally, higher levels of job engagement were associated with higher levels of teamwork, which, in turn, were associated with increased job satisfaction [26]. An interesting survey-based study comparing experiences of health care teams in Hong Kong and the United Kingdom found that team structure and job design contributed to employee well-being and that culture had a moderating effect on this impact [27]. A cross-sectional study of 12 primary care sites in various stages of transformation to a patient-centered medical home found a strong association between effective leadership, care team behaviors and perceptions (huddles, weekly meetings), and job satisfaction [28].
These studies indicate that optimizing team-based care is one potential lever to help solve the complex problem of decreased clinician well-being. Indeed, achieving effective teamwork is particularly important because teamwork has the potential to function as a demand or a resource: “Job demands deplete the individual’s energy and eventually decrease occupational well-being. Job resources, on the other hand, help employees attain goals, increase occupational well-being or reduce the strain caused by job demands” [1]. In other words, ineffective teamwork may be demanding for its members, leading to a higher workload and decreasing well-being. In contrast, if teamwork quality is high, teamwork may act as a resource, supporting clinicians in providing safe patient care and increasing their overall well-being [1].
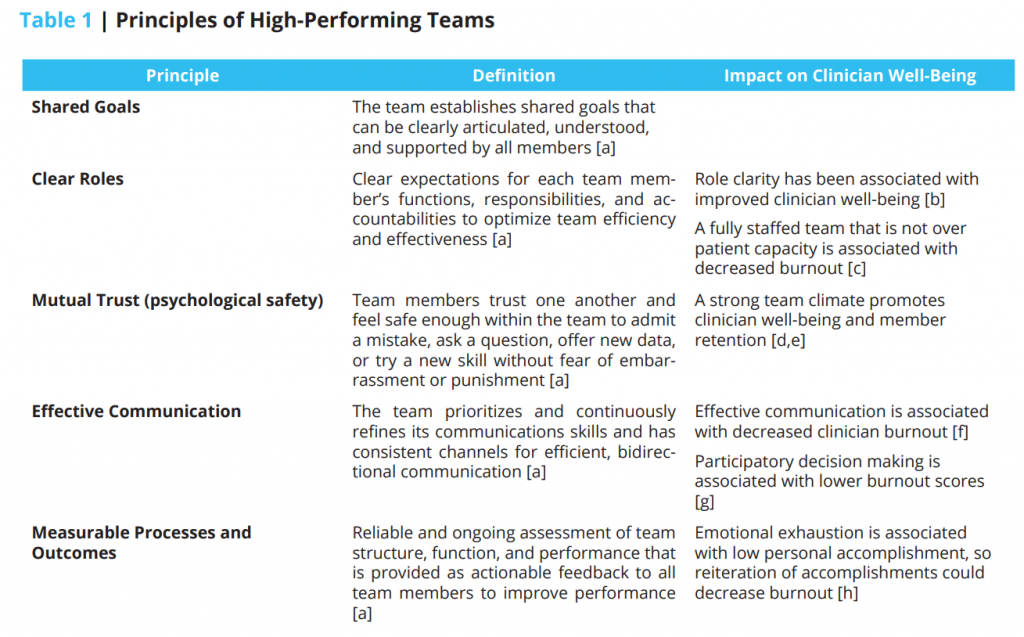
To illustrate how teamwork may act as a resource, it is useful to examine the components and qualities that characterize high-performing teams. Table 1 outlines the principles of high-performing teams [3] and their potential association with aspects of clinician well-being.
Further research is needed to fully understand the relationship between team-based care and clinician well-being. Additionally, it is important to note that optimizing team-based care is by no means a panacea and may require a baseline level of clinician well-being and a positive team culture to be most effective. A systematic review examining the association among teamwork, clinician well-being, and patient safety in hospital settings, identified several conceptual and methodological limitations of the current research [1]. The authors noted that “the main barrier to advancing our understanding of the causal relationships between teamwork, clinician well-being and patient safety is the lack of an integrative, theory-based, and methodologically thorough approach investigating the three concepts simultaneously and longitudinally. A holistic approach is needed that takes into account the complexity of teams in terms of team structure and different teamwork processes in healthcare organizations, especially in survey studies: for instance, in addition to focusing on the individual professions within the team, the entire multiprofessional team should be included” [1].
Drawing from psychological theory and their findings, Welp and Manser developed an integrative framework that addresses these limitations and proposes mechanisms by which these concepts might be linked (see Figure 1) [1]. Although this framework applies only to hospital settings, it may provide a useful starting point for the development of frameworks in other settings.

Figure 1 | Integrative Framework of Teamwork, Clinician Occupational Well-Being, and Patient Safety in Hospital Settings | Source: Welp and Manser, “Integrating teamwork, clinician occupational well-being and patient safety—development of a conceptual framework based on a systematic review,” BMC Health Services Research. NOTES: Creative Commons license: http://creativecommons.org/licenses/by/4.0/
Successful Models of High-Functioning and Effective Team-Based Care
The absence of robust evidence supporting a causal relationship between optimal team-based care and improved clinician well-being should not stall efforts to advance team-based health care. A wide range of successful models of high-functioning and effective team-based care have been demonstrated, and they may provide important lessons learned and principles to inform the development of future teams [29,30,31]. For example, in Federally Qualified Health Centers, patient-centered medical home implementation has been shown to lead to improvement in patient experience [32].
The development, implementation, and maintenance of health care teams that can improve patient outcomes and clinician well-being are complex endeavors and their manifestation will vary among different health care settings. Despite the heterogeneity of existing health care teams, all require some degree of ongoing investment of time and resources to achieve their potential.
There is a substantial body of literature establishing the science of teamwork and outlining strategies to improve teamwork, such as team-based training practices [33,34]. Furthermore, programs such as the Department of Defense and AHRQ’s Team Strategies and Tools to Enhance Performance and Patient Safety (https://www.ahrq.gov/teamstepps/index.html) have been used to integrate teamwork into practice.
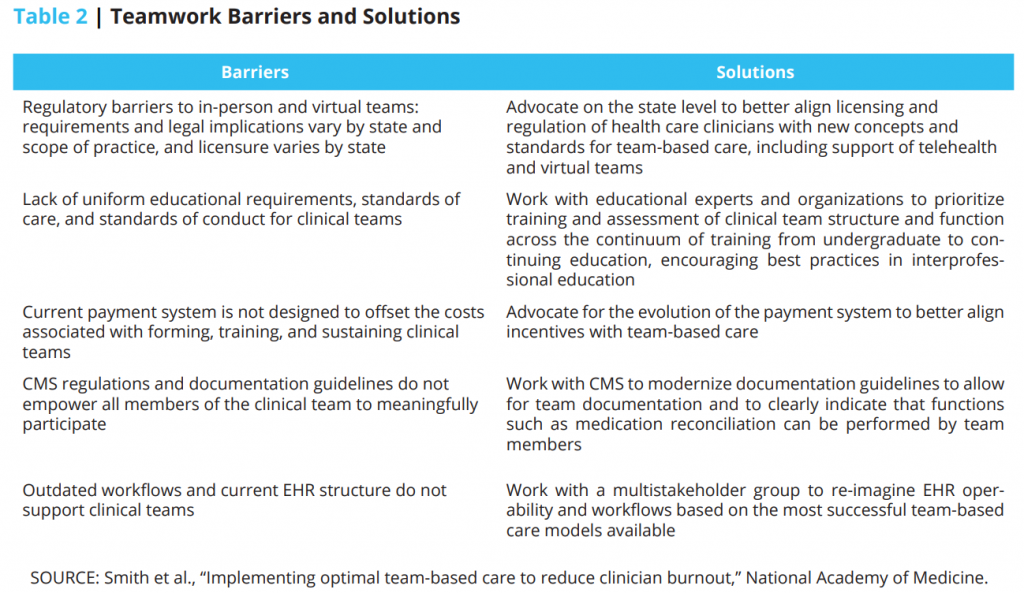
This discussion paper does not seek to provide a comprehensive overview of strategies and resources to inform the development of successful teams. Instead, the authors discuss key environmental and organizational barriers to optimal team-based care within the context of a larger health system. The following sections discuss key components of the system that may impede team-based care and proposed solutions to address such barriers.
Digital Barriers and Solutions
The digital health environment, particularly electronic health records (EHRs), is a barrier to team-based care. Although EHRs have important advantages in terms of improving continuous access to legible clinical information, they are not optimally designed to support clinical care. EHRs have been designed to meet outdated documentation guidelines for Centers for Medicare and Medicaid Services (CMS) billing that were established in the paper medical record era [35]. If used effectively, the EHR can facilitate team-based care and improve patient outcomes [32]. Chronic conditions, such as chronic kidney disease, have been identified as a unique area where EHRs can facilitate high-quality team-based care [36].
EHR platforms focus more on a single contributor to the notes than on multiple contributors [37]. The entire care team lacks adequate access to perform simple tasks, such as medication reconciliation, that would inform all the clinicians using the platform. Many important fields essential for care management, care gap analysis for prevention, and clinical care maintenance are simply not readily available.
Current EHRs do not facilitate exchange of data about a patient among clinicians in different health systems. For example, EHRs do not hold nationally standardized data and metadata, thus limiting data exchanges in a format that would allow for different EHR systems to machine-read and use the information such that clinicians could safely track patients under their care. These messaging functions are important aspects of digital health information functionality and are essential for optimal care.
In addition, patients have a limited view of their digital health information and cannot easily communicate with their care team. Patient portals are not easily navigated and shared, except to accomplish the most basic aspects of medication refills or to request an appointment [38]. The potential for a unified and seamless EHR system goes unrecognized, and this loss causes frustration for patients and the entire care team.
Regulatory changes are needed to leverage the full potential of digital health information. Those regulatory changes exist in several layers.
- Regulatory burdens within the EHR—such as excessive signature requirements or mandates that certain documentation tasks be performed only by physicians—should be examined and clarified.
- Promotion of the exchange of information between EHRs needs to be accelerated through regulatory requirements.
- Interoperability should include more than EHRs. Data liquidity in a digital health information environment must flow to the patient’s consolidated medical record in a patient cloud, into registries, and into performance measurement tools and software.
- To facilitate a learning health system, interoperability should promote deep learning, advances in predictive analytics, and the use of artificial intelligence to support patient care.
Changes in federal regulations should support the evolution of the digital health information environment, as illustrated by the following examples:
- CMS could modernize the documentation guidelines requirement and remove unnecessary redundancies to make clinical teams more efficient and effective. This will require an early phase to reduce the documentation burden and subsequent phases to build documentation into the clinical workflow for that patient. With these changes, all participants in the care delivery system, including the patient, could contribute documentation to the History of Present Illness, History, and Physical fields for which the key clinician is accountable.
- CMS, the Office of the National Coordinator (ONC), AHRQ, and the National Institutes of Health (NIH)/National Cancer Institute (NCI) could work with Health Level Seven International, Systematized Nomenclature of Medicine Clinical Teams, Logical Observation Identifiers Names and Codes, RxNorm, and others to create interoperability standards and Fast Healthcare Interoperability Resources profiles, and to expedite data liquidity and real-time information sharing for geographically remote teams.
- AHRQ, NIH/NCI, and National Library of Medicine could establish the digital foundational elements of a learning health system and evidence-based medicine to promote readily available clinical workflows to optimize team function in EHRs at the point of care in real time.
- ONC and CMS could make prescribed medication selection, alternatives, and pricing transparently available to clinical teams at the point of care as a regulatory EHR requirement.
Workforce Barriers and Solutions
In addition to the digital health barriers mentioned above, there are many issues related to the workforce itself that can impede and/or facilitate team-based care. These issues range from the training and mindset of health care team members to team organization and leadership. They also include larger contextual issues related to resources and staffing patterns. Despite the evidence that team-based care can improve outcomes and mitigate burnout—and despite the availability of material resources such as implementation guides for team-based care—barriers continue to exist. The lack of human resources is one fundamental barrier. A health care system or practice may seek to move to team-based care but cannot find the resources to augment the existing clinical staff with medical assistants, documentation assistants, or registered nurses (RNs). Another barrier is mindset. What constitutes “our team” and who is on it? Some health care professionals may carry a somewhat narrow and inflexible mindset (e.g., “only the people who work for me and/or directly around me are on my team”). Others may have a more wide-ranging, flexible, and adaptable perspective (e.g., “anyone who supports efforts to care for this patient is part of ‘our team’; decisions will be made based on the information and concerns provided by everyone on the team, including the patient”). These perspectives can manifest in issues such as whether a radiologist or pharmacist is part of the team, or how to coordinate both care and accountability for medically and/or socially complex patients. It should be noted that leading teams is a complex undertaking, especially when conflicts arise or unexpected challenges require changes to care plans.
Despite these barriers, promising solutions can promote team-based care. Process improvement methods such as Lean Six Sigma and others can be used to analyze the current state of operations and identify waste—in every system, there are such opportunities to identify and redeploy resources to promote team-based care. Team members can be trained in new skills—e.g., training medical assistants in basic health coaching and information management—that can add capacity to the existing team. Adding team members such as RNs can enhance the effectiveness of care and improve distribution of work. Addressing the “hidden curriculum,” practices that are not explicitly taught but tacitly followed, that may influence physicians and nurses to work in specialty/hospital–based practice versus ambulatory/primary care–based practice can promote high-quality and professionally satisfying practice in ambulatory care. Mindset and leadership issues can be addressed by adopting curricula and best practices from industries outside of health care. The field of aviation, the military, and the corporate sector all have promising practices that can be implemented in health care. For all health professionals, exposure to the theory and practice of team-based care should be part of both preclinical and clinical education, leveraging the growing body of knowledge and practical experience with Interprofessional Education/Interprofessional Practice [39,40]. For example, the 2016 update of the Accreditation Council for Pharmacy Education standards lists demonstrated competence in interprofessional team dynamics, including articulating the values and ethics that underpin interprofessional practice, engaging in effective interprofessional communication—e.g., conflict resolution and documentation skills—and honoring interprofessional roles and responsibilities [41]. Ongoing professional development and team coaching should be provided for all team members to sustain long-term high performance.
Payment Barriers and Solutions
The clinical care model, business operations, and fiscal models are important considerations for the implementation of team-based care.
There is widespread agreement that the current health care payment system has serious weaknesses, which may serve as barriers to team-based care [42]. For example, FFS continues to be the predominant payment method. In most FFS systems, there is no explicit payment to reimburse clinicians and other health care team members for their time and effort to coordinate services. For example, clinicians are often not paid for time spent discussing how to coordinate services for individual patients, and clinicians who play the role of a team leader are not compensated for their time involved in performing team leader duties [42]. Although the addition of team-based care codes, such as Medicare’s chronic care management code, are promising exceptions to the current FFS system, their impact has been limited by bureaucratic requirements and lack of utilization among primary care practices [43].
In recent years, the broader health care environment has increasingly emphasized a shift toward value. Notably, the passage of the Medicare Access and CHIP Reauthorization Act of 2015 created the Quality Payment Program, which shifts Medicare payment toward rewarding value over volume [44,45]. As a result, accountable care organizations (ACOs) and other alternative payment models will likely become prevalent modes of care delivery [46]. In light of these trends, it is in the interest of health care systems to embrace the shift to value now and not wait until it is the predominant mode of reimbursement.
Fortunately, the implementation of team-based care closely aligns with this shift. Team-based care has the ability to more effectively work toward the Quadruple Aim of (1) improving individuals’ and families’ experience of care, (2) improving population health, (3) lowering per capita costs, and (4) improving the work-life of health care providers [4,47].
Several studies have demonstrated the ability of team-based care to produce cost savings. Even under a typical FFS structure, implementation of team-based care in the management of uncontrolled hypertension has been suggested to have the potential over 10 years to produce more than $5 billion in savings to Medicare [48]. Moreover, a cost-benefit analysis of team-based care demonstrated that it is cost effective in improving blood pressure control [15]. Furthermore, a retrospective longitudinal cohort study found that per patient payments to the delivery system were lower in the team-based care group ($3,400 compared with $3,515 for traditional practices) and were lower than investment costs of the team-based care program [49].
The implementation of team-based care has been demonstrated to enhance individual clinician productivity. Implementation of team-based care resulted in an increased number of patient visits per day, which generated increased revenue and decreased cost per patient encounter [50].
ACOs can move health care delivery in a positive direction if they establish teamwork as “their unshakeable cultural priority,” while recognizing the challenges inherent in changing established patterns of behavior among clinicians [51]. “Support for team based care should focus on reimbursement for improved outcomes, while patients, payers, hospitals, and practices are held accountable for costs. Payers should create incentives for high value care that improves outcomes while decreasing costs” [4]. However, payers should also recognize that there will be instances when high-value care will not decrease costs or when cost savings will not be realized in the short term [4].
Barriers and facilitators to team-based care have been identified in the patient-centered medical home setting [52]. Barriers included a lack of intentional focus on team building and the loss of autonomy resulting from standardized workflows. Factors that were deemed critical to establishing team-based care included strong leadership—particularly regarding employing change management, co-locating team members in a shared workspace, standardizing roles and job expectations among team members, and adopting of team huddles.
Conclusion
Team-based care—or the provision of care by two or more health clinicians who work collaboratively with patients and their caregivers to accomplish shared goals—presents a unique opportunity to achieve key aims of a high-quality health system. Successful teams have the capacity to improve patient outcomes, the efficiency of care, and the satisfaction and well-being of health care clinicians.
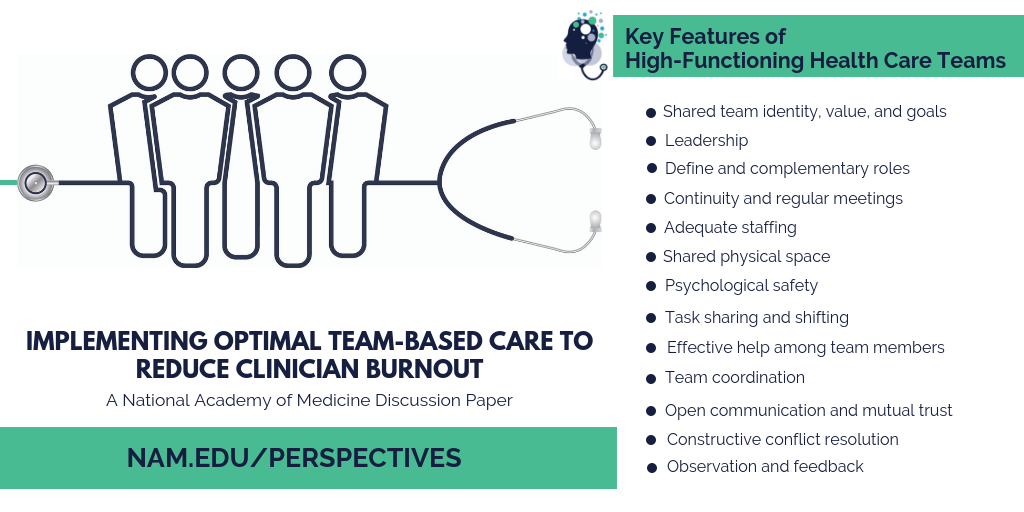
High-functioning health care teams come in a variety of compositions, yet all possess key features that make them successful. These include shared team identity, values, and goals; leadership; defined and complementary roles; continuity and regular meetings; adequate staffing; shared physical space; psychological safety; open communication and mutual respect; effective help among team members; constructive conflict resolution; task sharing and shifting; team coordination; and observation and feedback.
In increasingly complex health care systems, high-functioning teams are more essential than they have ever been and more challenging to develop and sustain. This paper describes critical, evidence-based elements of high-functioning clinical teams, including clearly articulated goals and roles, an enabling social structure with expert leadership and psychological safety, a supportive organization that assures needed resources, and coaching that promotes the function and well-being of the team and its members. It also describes studies of a variety of clinical teams that have had improved patient and clinician outcomes. Finally, the paper explores opportunities to overcome barriers to the implementation of teamwork in health care by harnessing the power of digital health information technology to support more efficient documentation, standardized communication and workflows, and non-geographically located teams. Team training is also a means for investing in the continuous professional development of clinicians, keeping them engaged and practicing at the top of their licenses. Training can also break down the silo-ed approach to the undergraduate and graduate education of clinicians.
The current payment models are complex and superficially seem to dissuade investment in clinical teams; however, the evidence for the return on investment for training and sustaining clinical teams is considerable in both the FFS and value-based payment constructs. Although the opportunity costs for organizations to invest in clinical teams seem considerable with the increasing complexity and constant change of the health care system, the evidence is clear: Health care organizations that do not invest in training and sustaining their clinical teams will be at a significant financial disadvantage in the long term.
High-functioning teams have tremendous potential to promote clinician well-being, which is foundational to effective and efficient health care. We need additional research to help health care organizations routinely measure teamwork using reliable and valid instruments. There is also a need for longitudinal studies that better elucidate the relationship between high-functioning teams and clinician well-being, so health care organizations and practices have a clear road map for evidence-based implementation of team-based care.
Join the conversation!
![]() Tweet this! Teamwork matters for #ClinicianWellBeing. But how do we foster effective team-based care? Authors explore in new paper from @theNAMedicine: https://doi.org/10.31478/201809c
Tweet this! Teamwork matters for #ClinicianWellBeing. But how do we foster effective team-based care? Authors explore in new paper from @theNAMedicine: https://doi.org/10.31478/201809c
![]() Tweet this! Teamwork has been found to partially mitigate the relationship between work demands and burnout. Why certain strategies may help us better implement team-based care in an effort to achieve #ClinicianWellBeing: https://doi.org/10.31478/201809c
Tweet this! Teamwork has been found to partially mitigate the relationship between work demands and burnout. Why certain strategies may help us better implement team-based care in an effort to achieve #ClinicianWellBeing: https://doi.org/10.31478/201809c
![]() Tweet this! New discussion paper from @theNAMedicine identifies key features of high-functioning health care teams and why these teams are so essential for #ClinicianWellBeing & better patient care: https://doi.org/10.31478/201809c
Tweet this! New discussion paper from @theNAMedicine identifies key features of high-functioning health care teams and why these teams are so essential for #ClinicianWellBeing & better patient care: https://doi.org/10.31478/201809c
![]() Tweet this! High-functioning health care teams have tremendous potential to promote #ClinicianWellBeing. New paper explores why: https://doi.org/10.31478/201809c
Tweet this! High-functioning health care teams have tremendous potential to promote #ClinicianWellBeing. New paper explores why: https://doi.org/10.31478/201809c
Download the graphics below and share them on social media!
References
- Welp, A., and T. Manser. 2016. Integrating teamwork, clinician occupational well-being and patient safety—development of a conceptual framework based on a systematic review. BMC Health Services Research 16(1):281. https://doi.org/10.1186/s12913-016-1535-y
- Naylor, M. D., K. D. Coburn, E. T. Kurtzman, J. P. Bettger, H. G. Buck, J. V. Cleave, and C. A. Cott. 2010. Inter-professional team-based primary care for chronically ill adults: State of the science. Unpublished white paper presented at the ABIM Foundation Meeting to Advance Team-Based Care for the Chronically Ill in Ambulatory Settings, Philadelphia, PA.
- Mitchell, P., M. Wynia, R. Golden, B. McNellis, S. Okun, C.E. Webb, V. Rohrbach, and I. Von Kohorn. 2012. Core principles & values of effective team-based health care. NAM Perspectives. Discussion Paper, National Academy of Medicine, Washington, DC. https://doi.org/10.31478/201210c
- American College of Obstetricians and Gynecologists. 2016. Collaboration in practice: Implementing team based care. Washington, DC. Available at: https://www.acog.org/clinical/clinical-guidance/task-force-report/articles/2016/collaboration-in-practice-implementing-team-based-care (accessed September 2, 2020).
- Hackman, R. 2014. What makes for a great team? Washington, DC: American Psychological Association. Available at: https://www.apa.org/science/about/psa/2004/06/hackman (accessed September 2, 2020).
- Gordon, S., D. L. Feldman, and M. Leonard. 2014. Collaborative caring: Stories and reflections on teamwork in health care. Ithaca, NY: Cornell University Press. https://doi.org/10.3163/1536-5050.104.1.017
- Bodenheimer, T., and R. Willard-Grace. 2016. Teamlets in primary care: Enhancing the patient and clinician experience. Journal of the American Board of Family Medicine 29(1):135-138. https://doi.org/10.3122/jabfm.2016.01.150176
- Agency for Healthcare Research and Quality. 2014. TeamSTEPPS long-term care implementation guide. Available at: https://www.ahrq.gov/teamstepps/longtermcare/implement/implguide.html (accessed November 22, 2017).
- Pape, G. A., J. S. Hunt, K. L. Butler, J. Siemienczuk, B. H. LeBlanc, W. Gillanders, Y. Rozenfeld, and K. Bonin. 2011. Team-based care approach to cholesterol management in diabetes mellitus: Two-year cluster randomized controlled trial. Archives of Internal Medicine 171(16):1480-1486. https://doi.org/10.1001/archinternmed.2011.417
- Groenestege-Kreb, D. T., O. Van Maarseveen, and L. Leenen. 2014. Trauma team. British Journal of Anaesthesia 113(2):258-265. https://doi.org/10.1093/bja/aeu236
- Roberts, M. S., J. A. Stokes, M. A. King, T. A. Lynne, D. M. Purdie, P. P. Glasziou, D. A. J. Wilson, S. T. McCarthy, G. E. Brooks, F. J. de Looze, and C. B. Del Mar. 2001. Outcomes of a randomized controlled trial of a clinical pharmacy intervention in 52 nursing homes. British Journal of Clinical Pharmacology 51(3):257-265. https://doi.org/10.1046/j.1365-2125.2001.00347.x
- Njie, G. J., K. K. Proia, A. B. Thota, R. K. C. Thota, D. P. Hopkins, S. M. Banks, D. B. Callahan, N. P. Pronk, K. J. Rask, D. T. Lackland, T. E. Kottke, and Community Preventive Services Task Force. 2015. Clinical decision support systems and prevention: A community guide cardiovascular disease systematic review. American Journal of Preventive Medicine 49(5):784-795. Available at: https://www.thecommunityguide.org/content/clinical-decision-support-systems-and-prevention-community-guide-cardiovascular-disease (accessed September 2, 2020).
- Panattoni, L., L. Hurlimann, C. Wilson, M. Durbin, and M. Tai-Seale. 2017. Workflow standardization of a novel team care model to improve chronic care: A quasi-experimental study. BMC Health Services Research 17(1):286. https://doi.org/10.1186/s12913-017-2240-1
- Chang, H., Y. Liu, M. Lu, S. Jou, Y. Yang, D. Lin, K. H. Lin, K. Tzen, R. Yen, C. C. Lu, C. J. Liu, S. S. Peng, Y. Jeng, S. Huang, H. Lee, H. F. Juan, M. Huang, Y. Liao, Y. Lee, and W. Hsu. 2016. A multidisciplinary team care approach improves outcomes in high-risk pediatric neuroblastoma patients. Oncotarget 8(3):4360-4372. https://doi.org/10.18632/oncotarget.13874
- Jacob, V., S. K. Chattopadhyay, A. B. Thota, K. K. Proja, G. Njie, D. P. Hopkins, R. K. C. Finnie, N. P. Pronk, T. E. Kottke, and Community Preventive Services Task Force. 2015. Economics of team-based care in controlling blood pressure: A community guide systematic review. American Journal of Preventive Medicine 49(5):772-783. https://doi.org/10.1016/j.amepre.2015.04.003
- Reiss-Brennan, B., K. D. Brunisholz, C. Dredge, P. Briot, K. Grazier, A. Wilcox, L. Savitz, and B. James. 2016. Association of integrated team-based care with health care quality, utilization, and cost. JAMA 316(8):826-834. https://doi.org/10.1001/jama.2016.11232
- Manser, T. 2009. Teamwork and patient safety in dynamic domains of healthcare: A review of the literature. Acta Anaesthesiologica Scandinavica 53(2):143-151. https://doi.org/10.1111/j.1399-6576.2008.01717.x
- Wang, S. M., P. T. Kung, W. H. Wang, K. H. Huang, and W. C. Tsai. 2014. Effects of multidisciplinary team care on utilization of emergency care for patients with lung cancer. American Journal of Managed Care 20(8):e353-364. https://doi.org/https://pubmed.ncbi.nlm.nih.gov/25295798
- Schubert, C. C., L. J. Myers, K. Allen, and S. R. Counsell. 2016. Implementing geriatric resources for assessment and care of elders team care in a Veterans Affairs medical center: Lessons learned and effects observed. Journal of the American Geriatrics Society 64(7):1503-1509. https://doi.org/10.1111/jgs.14179
- Mundt, M. T., V. J. Gilchrist, M. F. Fleming, L. I. Zakletskia, W. Tuan, and J. W. Beasley. 2015. Effects of primary care team social networks on quality of care and costs for patients with cardiovascular disease. Annals of Family Medicine 13(2):139-148. https://doi.org/10.1370/afm.1754
- Dyrbye, L. N., T. D. Shanafelt, C. A. Sinsky, P. F. Cipriano, J. Bhatt, A. Ommaya, C. P. West, and D. Meyers. 2017. Burnout among health care professionals: A call to explore and address this underrecognized threat to safe, high-quality care. NAM Perspectives. Discussion Paper, National Academy of Medicine, Washington, DC. https://doi.org/10.31478/201707b
- Dehn, R. W., D. M. Brock, A. O. Keller, R. S. Hooker, D. Mittman. 2015. Commentaries on health services research. Journal of the American Academy of Physician Assistants 28(6):1-3. https://doi.org/10.1097/01.JAA.0000465232.59384.6f
- Willard-Grace, R., D. Hessler, E. Rogers, K. Dubé, E. Bodenheimer, and K. Grumbach. 2014. Team structure and culture are associated with lower burnout in primary care. Journal of the American Board of Family Medicine 27:229-238. https://doi.org/10.3122/jabfm.2014.02.130215
- Day, A. L., A. Sibley, N. Scott, J. M. Tallon, and S. Ackroyd-Stolarz. 2009. Workplace risks and stressors as predictors of burnout: The moderating impact of job control and team efficacy. Canadian Journal of Administrative Sciences 26:7-22. https://doi.org/10.1002/cjas.91
- Lin, Y., and Y. Huang. 2014. Team climate, emotional labor and burnout of physicians: A multilevel model. Journal of Taiwan Public Health 33(3):271-289. https://doi.org/10.6288/TJPH201433103012
- Mijakoski, D., J. Bislimovska, M. Milosevic, and J. Minov. 2015. Differences in burnout, work demands and team work between Croatian and Macedonian hospital nurses. Cognition, Brain, Behavior 19(3):179-200. Available at: https://www.researchgate.net/publication/282085378_Differences_in_burnout_work_demands_and_team_work_between_Croatian_and_Macedonian_hospital_nurses (accessed September 2, 2020).
- So, T. T. C., M. A. West, and J. F. Dawson. 2011. Team-based working and employee well-being: A crosscultural comparison of United Kingdom and Hong Kong health services. European Journal of Work and Organizational Psychology 20(3):305-325. https://doi.org/10.1080/13594320903384821
- Stout, S., L. Zallman, L. Arsenault, A. Sayah, and K. Hacker. 2017. Developing high-functioning teams: Factors associated with operating as a “real team” and implications for patient-centered medical home development. Inquiry (54). https://doi.org/10.1177/0046958017707296
- Hooker, R. S., J. Cawley, C. Everett, and D. M. Brock. 2017. Commentaries on health services research. Journal of the American Academy of Physician Assistants 30(8):1-3. https://doi.org/10.1097/01.JAA.0000558380.39352.af
- Hastings, S. E., E. Suter, J. Bloom, and K. Sharma. 2016. Introduction of a team-based care model in a general medical unit. BMC Health Services Research 16(1):245. https://doi.org/10.1186/s12913-016-1507-2
- Hunt, J. S., J. Siemienczuk, G. Pape, Y. Rozenfeld, J. MacKay, B. H. LeBlanc, and D. Touchette. 2008. A randomized controlled trial of team-based care: Impact of physician-pharmacist collaboration on uncontrolled hypertension. Journal of General Internal Medicine 23(12):1966-1972. https://doi.org/10.1007/s11606-008-0791-x
- Kawamoto, K., K. J. Anstrom, J. B. Anderson, H. B. Bosworth, D. F. Lobach, C. M. Marx, J. M. Ferranti, H. Shang, and K. S. H. Yarnall. 2016. Long-term impact of an electronic health record-enabled, team-based, and scalable population health strategy based on the chronic care model. AMIA Annual Symposium Proceedings:686-695. Available at: https://pubmed.ncbi.nlm.nih.gov/28269865/ (accessed September 2, 2020).
- Hackman, J. R. 1990. Teams that work (and those that don’t): Creating conditions for effective teamwork. Somerset, NJ: Jossey-Bass.
- Salas, E., S. Zajac, and S. L. Marlow. 2018. Transforming health care one team at a time: Ten observations and the trail ahead. Group & Organization Management 43(3): 357-381. https://doi.org/10.1177/1059601118756554
- Ommaya, A. K., P. F. Cipriano, D. B. Hoyt, K. A. Horvath, P. Tang, H. L. Paz, M. S. DeFrancesco, S. T. Hingle, S. Butler and C. A. Sinsky. 2018. Care-Centered Clinical Documentation in the Digital Environment: Solutions to Alleviate Burnout. NAM Perspectives. Discussion Paper, National Academy of Medicine, Washington, DC. https://doi.org/10.31478/201801c
- Drawz, P. E., P. Archdeacon, C. J. McDonald, N. R. Powe, K. A. Smith, J. Norton, D. E. Williams, U. D. Patel, and A. Narva. 2015. CKD as a model for improving chronic disease care through electronic health records. Clinical Journal of the American Society of Nephrology 10(8):1488-1499. https://doi.org/10.2215/CJN.00940115
- Clark, C. 2016. 10 ways EHRs lead to burnout. Family Practice News Digital Network, March 28. Available at: https://www.mdedge.com/chestphysician/article/107632/practice-management/10-ways-ehrs-lead-burnout (accessed September 2, 2020).
- Baldwin J. L., H. Singh, D. F. Sittig, and T. D. Giardina. 2017. Patient portals and health apps: Pitfalls, promises, and what one might learn from the other symptoms. Healthcare 5:81-85. https://doi.org/10.1016/j.hjdsi.2016.08.004
- O’Leary, K. J., D. B. Wayne, C. Haviley, M. E. Slade, J. Lee, and M. V. Williams. 2010. Improving teamwork: Impact of structured interdisciplinary rounds on a medical teaching unit. Journal of General Internal Medicine 25(8):826-832. https://doi.org/10.1007/s11606-010-1345-6
- Weller, J., M. Boyd, and D. Cumin. 2014. Teams, tribes and patient safety: Overcoming barriers to effective teamwork in healthcare. Postgraduate Medical Journal 90(1061):149-154. https://doi.org/10.1136/postgradmedj-2012-131168
- Accreditation Council for Pharmacy Education. 2016. Accreditation standards and key elements for the professional program in pharmacy leading to the doctor of pharmacy degree. Chicago. Available at: https://www.acpe-accredit.org/pdf/Standards2016FINAL.pdf (accessed September 2, 2020).
- Network for Regional Healthcare Improvement. 2016. Accelerating the implementation of value-based care and payment: Recommendations from the 2016 National Payment Reform Summit. Portland, ME: Available at: http://www.nrhi.org/uploads/2016_nationalpaymentreformsummit.pdf (accessed September 2, 2020).
- Wohler, D. M., and W. Liaw. 2016. Team-based primary care: Opportunities and challenges. Available at: https://www.graham-center.org/content/dam/rgc/documents/publications-reports/reports/StarfieldSummit_Report_TeamBasedPrimaryCare.pdf (accessed September 2, 2020).
- Centers for Medicare and Medicaid Services (CMS). 2017. MACRA. Available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Value-Based-Programs/MACRA-MIPS-and-APMs/MACRA-MIPS-and-APMs.html (accessed November 30, 2017).
- Alternative payment model (APM) design toolkit. Washington, DC. Available at: https://www.cms.gov/Medicare/Quality-Payment-Program/Resource-Library/Alternative-Payment-Model-APM-Design-Toolkit.pdf (accessed November 30, 2017).
- Milken Institute. A closer look at alternative payment models. Santa Monica, CA. Available at: http://www.fastercures.org/assets/Uploads/PDF/VC-Brief-AlternativePaymentModels.pdf (accessed November 30, 2017).
- Bodenheimer, T., and C. Sinsky. 2014. From triple to Quadruple Aim: Care of the patient requires care of the provider. Annals of Family Medicine 12(6):573-576. https://doi.org/10.1370/afm.1713
- Dehmer, S. P., M. M. Baker-Goering, M. V. Maciosek, Y. Hong, T. E. Kottke, K. L. Margolis, J. C. Will, T. J. Flottemesch, A. B. LaFrance, B. C. Martinson, A. J. Thomas, and K. Roy. 2016. Modeled health and economic impact of team-based care for hypertension. American Journal of Preventive Medicine 50(5):S34-S44. https://doi.org/10.1016/j.amepre.2016.01.027
- Brunetto, Y., R. F. Wharton, and K. Shacklock. 2011. Supervisor-nurse relationships, teamwork, role ambiguity and well-being: Public versus private sector nurses. Asia Pacific Journal of Human Resources 49(2):143-164. Available at: https://core.ac.uk/download/pdf/143869139.pdf (accessed September 2, 2020).
- Hopkins, K. D., and C. A. Sinsky. 2014. Team-Based Care: Saving Time and Improving Efficiency. Family Practice Management 21(6):23-29. Available at: https://www.aafp.org/fpm/2014/1100/p23.html (accessed September 2, 2020).
- Berry, L. L., and D. Beckham. 2014. Team-based care at Mayo Clinic: A model for ACOs. Journal of Healthcare Management 59(1):9-13. https://doi.org/10.1097/00115514-201401000-00003
- Cromp, D., C. Hsu, K. Coleman, P. A. Fishman, D. T. Liss, K. Ehrlich, E. Johnson, T. R. Ross, C. Trescott, B. Trehearne, and R. J. Reid. 2015. Barriers and facilitators to team-based care in the context of primary care transformation. Journal of Ambulatory Care Management 38(2):125-133. https://doi.org/10.1097/JAC.0000000000000056