Fourth Annual DC Public Health Case Challenge: The Changing American City and Implications for the Health and Well-Being of Vulnerable Populations
In 2016 the National Academy of Medicine (NAM) and the Roundtable on Population Health Improvement, of the National Academies of Sciences, Engineering, and Medicine (the National Academies) held the fourth annual District of Columbia (DC) Public Health Case Challenge (https://nam.edu/initiatives/dc-public-health-case-challenge/), which had its inaugural year in 2013 and was both inspired by and modeled on the Emory University Global Health Case Competition (http://globalhealth.emory.edu/what/student_programs/case_competitions/index.html).
The DC Case Challenge aims to promote interdisciplinary, problem-based learning in public health and to foster engagement with local universities and the local community. The Case Challenge engages graduate and undergraduate students from multiple disciplines and universities to come together to promote awareness of and develop innovative solutions for 21st-century public health issues that are grounded in a challenge faced by the local DC community.
Each year the organizers and a student case-writing team develop a case based on a topic that is relevant to the DC area and has broader domestic and, in some cases, global resonance. Content experts are then recruited as volunteer reviewers of the case. Universities located in the Washington, DC, area are invited to form teams of three to six students, who must be enrolled in undergraduate or graduate degree programs. In an effort to promote public health dialogue among a variety of disciplines, each team is required to include representation from at least three different schools, programs, or majors.
Two weeks before the Case Challenge event, the case is released, and teams are charged to employ critical analysis, thoughtful action, and interdisciplinary collaboration to develop a solution to the problem presented in the case. On the day of the competition, teams present their proposed solutions to a panel of judges composed of representatives from local DC organizations as well as other subject matter experts from disciplines relevant to the case.
2016 Case: The Changing American City and Implications for the Health and Well-Being of Vulnerable Populations
The 2016 case focused on the changing American city and implications for the health and well-being of vulnerable populations. The case asked the student teams to develop a program, with a grant of $2 million over five years, that would mitigate the negative effects of urban change on the city’s most vulnerable populations, including residents of low-income minority communities, those who are displaced or at risk of displacement, and those who are homeless. Each proposed solution was expected to offer a rationale, a proposed intervention, an implementation plan, a budget, and an evaluation plan.
The case framed the issue through three scenarios portraying a range of issues faced by vulnerable groups and the conditions created by recent and ongoing policies that put certain groups at risk in changing urban areas. Though the three illustrative scenarios were fictional, they drew from actual circumstances faced by DC residents. The first scenario described a young, Salvadoran mother without insurance working three part-time jobs to support her parents and young son, struggling to afford medication for her type 2 diabetes, and living in a neighborhood (Adams Morgan) that had until recently been a food desert. In the second scenario, a young boy with asthma lives in a non-smoke-free apartment complex in southwest DC with his family, who is increasingly unable to afford rent and groceries and considering moving to the suburbs, despite the strong social support of their neighborhood. The third scenario described an elderly widow with limited mobility and failing eyesight who lives alone in the Bloomingdale area. Eligible for Medicaid, receiving Social Security benefits, but struggling to afford medication and groceries, she must rely on public transportation and is in need of a home health aide.
The teams were provided with background information on urban renewal, the history of chronic disease in DC, health equity in DC, and issues affecting low-income populations in gentrifying areas (including race, discrimination, and oppression; economic and social mobility; affordable housing and homelessness; accessibility and the built environment; health and education; food and nutrition; and health care and social services in changing neighborhoods).
Team Case Solutions
The following brief synopses prepared by students from the seven teams that participated in the 2016 Case Challenge describe how teams identified a specific need in the topic area, how they formulated a solution to intervene, and how they would implement their solution if they were granted the fictitious $2 million allotted to the winning proposal in the case. Team summaries are provided in alphabetical order.
The 2016 Grand Prize winner was the George Washington University. Three additional prizes were awarded: two Practicality Prizes, to the teams from Howard University and the Uniformed Services University of the Health Sciences, and the Harrison C. Spencer Interprofessional Prize, to American University. The interprofessional prize has been awarded in past years, but in 2016, it was named in memory of Dr. Harrison C. Spencer, who was, until August 2016, the president and chief executive officer of the Association of Schools and Programs of Public Health, and a champion of interprofessional dialogue and collaboration to improve the public’s health.
American University
Team members: Michael DeJesus, Rain Freeman, Kara Suvada, Rebecca Taylor, Liliana Zigo
Statement of Need
A third of all children in Washington, DC, live in poverty, and most are concentrated in neighborhoods east of the Anacostia River [1]. Children are a vulnerable population because they depend on their families and communities to thrive; those who live in poverty often live in areas that lack access to critical resources [1]. Without access to healthy foods, functioning recreation centers, and spaces for exercise, children are at an early disadvantage and at risk for negative health outcomes in the future. To lead healthy lives as adults, children must be given access to the resources necessary to foster healthy lifestyles during childhood.
Goal
The American University team created the Imagine Initiative with a mission to prevent exposure to risk factors that result in the development of chronic disease, specifically childhood obesity. The initiative includes school-based peer mentorship, community partnerships, and behavioral change. Central aims of the mission include increasing self-efficacy and empowering future advocates for the community.
Intended Outcomes
The peer-education and -mentorship component of the intervention is aimed at providing healthy models for young children and improving community connectedness. This element also promotes teaching healthy behaviors that have the potential to reduce chronic disease burden in the future. The mobile farmers market component addresses immediate needs for fresh and affordable food options, and promotes the development of intergenerational buy-in and community connectedness.
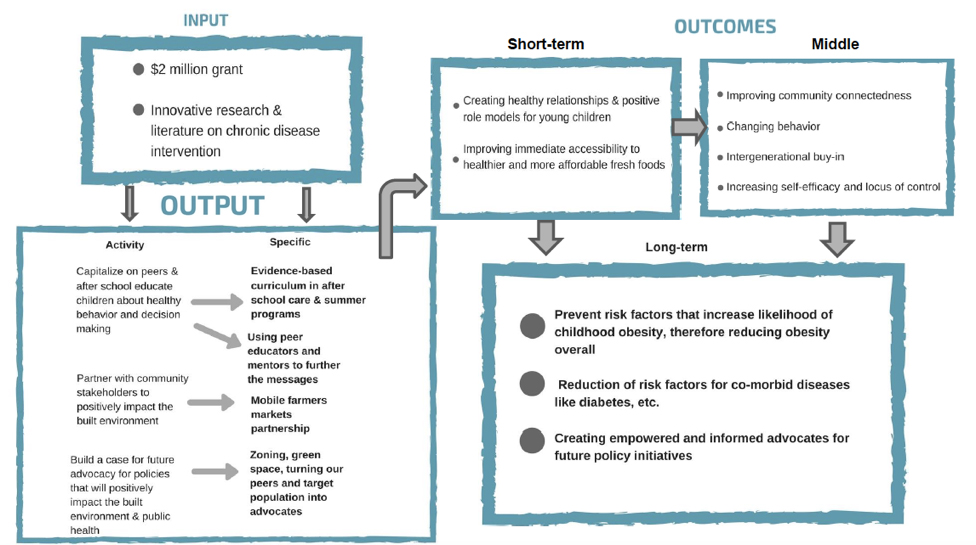
This intervention relies on involvement of the target community to work cohesively as informed and empowered individuals. Students are encouraged to become advocates for their communities and to call for policies that foster a built environment that supports healthy behaviors and prevents risk factors that can lead to chronic disease. Figure 1 shows a logic model describing the intervention’s inputs; outputs; and short-, middle-, and long-term outcomes.
Figure 1 | Logical Model for the Imagine Initiative
Intervention
The target population for the Imagine Initiative includes Aiton Elementary School and H.D. Woodson High School in Ward 7, and King Elementary School and Ballou High School in Ward 8 of Washington, DC. The American University team based its strategy on social cognitive theory, which emphasizes that behavior change requires multiple, interrelated components [2]. This theory relies on the dynamic and reciprocal interaction of person, environment, behavioral capability, observational learning, reinforcements, positive expectations, and self-efficacy [2].
There are three main components of the Imagine Initiative: (1) peer mentorship and the after-school Coordinated Approach to Child Health (CATCH) program (see http://catchinfo.org/ for more information), (2) continued summer programming, and (3) a mobile farmers market through community partnerships. The peer-mentorship program offers high-school students the opportunity to fulfill their required community service hours by facilitating health-focused lesson plans. Student mentees in the program become mentors during high school as a means of ensuring sustainability within the program. The second program component seeks to partner with the DC Department of Parks and Recreation to continue peer mentorship and programming throughout the summer in recreation facilities near the schools. Community partnerships will aid the goals of the third element, the farmers market: to provide fresh produce in food deserts to increase healthier eating habits and, in the long term, to positively enhance the built environment.
Potential Barriers and Responses
The success of the Imagine Initiative depends on the consistent enrollment in after-school care and the involvement of families in the mobile farmers market. The Imagine Initiative school program reaches only those students who are enrolled in and attending partner schools’ after-school programs. Consequently, the intervention may not reach students in the schools who are not enrolled in the program. However, these students will be reached by the mobile farmers market that travels to neighborhoods surrounding the schools. Additionally, in the planning stage school staff informed the intervention team that after-school program participation is extremely common and
that “almost all” of their students attend after-school programs at some point. Perhaps, in the future, the program could be expanded to include a component during the school day so that more students would be reached.
George Mason University
Team members: Nadia Busekrus, Paige Dunleavy, Iris Greenspan, Zoe Quint, Riddhi Shah, Rediet Woldeslassie
Statement of Need
Although gentrification often leads to the establishment of more resources (such as grocery stores or health centers) in historically impoverished or underdeveloped neighborhoods, these resources are often not accessible to all. While there are food banks, public aid programs, and other health-supporting resources available to Washington, DC, residents, poor access to care and unequal distribution of resources pose a problem for many people in DC, specifically those who live east of the Anacostia River in Wards 7 and 8 [3].
Goal
The George Mason University team created a program, Access-8, with a mission to help connect Ward 8 families with health-supporting resources close to their neighborhoods via a peer-led counseling initiative. Through these relationships, Ward 8 residents could be given empowering tools to help maintain control of their health and their lives.
Intended Outcomes
Access-8’s measurable goals include improved overall health literacy, healthier eating habits [4], increased medication adherence, reduced overall emergency room visits, and increased regular appointments with a primary care provider [5]. The team’s research showed that the incredibly fast rate of gentrification in DC includes multiple scheduled and future building projects for areas of Ward 8 [6]. Setting up a program like Access-8 could facilitate greater awareness of the need to make more inclusive investments in existing community members.
Intervention
Target population: Research shows that Ward 8 in Washington, DC, continues to have a high prevalence of poverty, substandard housing and education, and unmanaged chronic disease among its residents [3]. Thus, the decision was made to focus on this community specifically.
Underlying theory: Access-8 was modeled on several other successful programs, particularly the Peer Health Exchange program, which focuses on health education in DC communities by training college students to educate and inform high-school students in underresourced communities [7]. Additionally, we relied on guidelines from The Community Guide (a highly respected public health resource for evidence-based approaches to health improvement) on community outreach and education for chronic disease [8]. Lastly, the work done by the University of Michigan Health System provided a successful example of connecting vulnerable populations to community health care services and resources [9]. The University of Michigan Health System approach encouraged a variety of community partnerships to ensure the longevity of their programs.
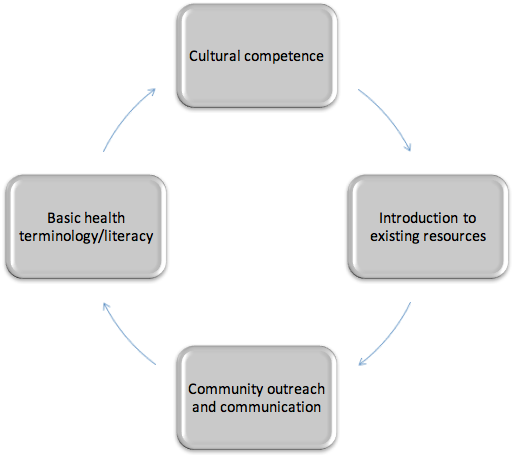
Mechanism and strategy: Access-8 will accomplish its mission by recruiting Ward 8 community members and local university students to undergo training and act as community “navigators.” These navigators will reach out via face-to-face engagement to inform Ward 8 residents about health-building resources as well as the importance of improving their overall health literacy. These navigators will constitute the volunteer parttime staff. Each volunteer will have mandatory training that includes modules on cultural competence and basic health care literacy (see Figure 2). The minimum commitment is one academic year, 10 hours a week, or during the summer for three months at 40 hours a week. The Access-8 team will also hire full-time paid staff members (social worker and office staff). In the third year of the program, an evaluation specialist will be hired for ongoing monitoring and evaluation.
Figure 2 | Training Modules for Access-8 Volunteers
Potential partners: The most significant partner organization for Access-8 is the Town Hall Education Arts Recreation Campus (THEARC), a nonprofit community-based organization operated by Building Bridges Across the River, whose mission is “to improve the quality of life for children and adults who reside east of the Anacostia River” [10]. A community hub located in Anacostia, THEARC has offered in-kind office space in which the Access-8 headquarters would be housed. The partnership with THEARC will also bolster the sustainability of the Access-8 program, as THEARC is a no-cost resource and an established center of activity within the Ward 8 community. Other organizations and services—such as the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC); the Supplemental Nutrition Assistance Program (SNAP); government-subsidized child care; community gardens; and free clinics—will be promoted as resources to program participants.
Potential Barriers and Responses
The Access-8 program was designed for the Ward 8 community as a whole, and staff will maintain an expansive approach to accomplish the level of community engagement necessary for the program’s success. By partnering with local organizations that facilitate community gatherings, including places of worship and local businesses, the legitimacy of Access-8 can be supported by community opinion leaders. These organizations can also afford Access-8 an ongoing presence at events so that staff and volunteers can further engage with residents.
Georgetown University
Team members: Sahil Chaudhary, Noah Martin, Robin Megill, Allyn Rosenberger, Neha Shah, Matthew Simmons, Breanna Walsh, Alex Webb
Overview
Washington, DC’s changing geographic and socioeconomic landscape has diminished the ability of many residents to access health resources. Of note, the rapidly changing urban landscape has fractured communities; this lack of social infrastructure is detrimental to both physical and mental health conditions and augments the dearth of resources for community members. To address these issues, we developed My Health Compass.
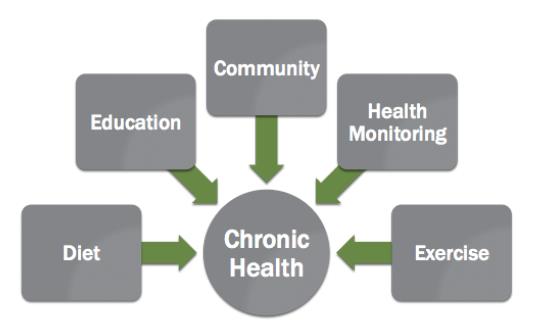
As shown in Figure 3, there are several components that play a critical role in the reduction of chronic disease burden. My Health Compass synthesizes these components and serves as a guide to the complicated landscape of personal health. My Health Compass is a digital application (app) designed to reduce the burden of chronic disease in Washington, DC’s vulnerable populations. The app provides health education, health monitoring, and diet and exercise tips. Importantly, this app connects users to other users in their community and fosters a sense of community through a digital modality. Through this app, individuals can maintain ties with communities of which they were once a part and build community with others in their new geographic location.
Figure 3 | Overview of My Health Compass’s Model to Improve Chronic Health
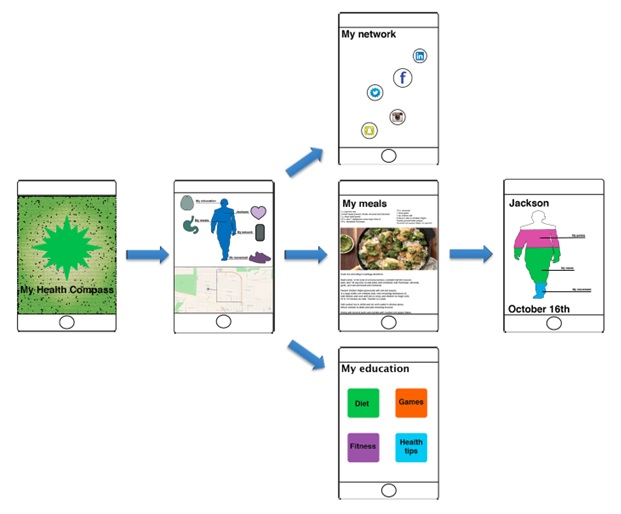
My Health Compass connects members to a network of personal health improvement opportunities [11]. Following the input of user information, the app identifies individualized health needs and establishes personal health plans that fit the context of the user’s everyday life (see Figure 4 for an example of the app’s user interface). It tracks user habits and identifies convenient and affordable health resources for users. For example, the app can be used to locate convenient sources of healthy food located along an individual’s normal daily commute, thereby minimizing the burden of grocery shopping in distant areas [12]. Our partners (described below) provide incentives and discounts at their locations, allowing these convenient options also to be more affordable. In addition, My Health Compass provides a digital interface wherein users can compete with one another to meet health and fitness goals, while also providing advice and support for those wishing to improve their personal health metrics.
Figure 4 | Example of My Health Compass’s User Interface
Therefore, partnerships play a critical role in the program. We seek to develop relationships with local clinics, grocery stores, sustainable food initiatives, and local government agencies to ensure ample availability of resources. Because My Health Compass serves as a community-building tool, partner organizations will likely experience increased traffic. This influx of customers, combined with the benefit of good publicity, will incentivize their participation, creating an atmosphere where numerous private interests align with our civic mission.
Theory
A number of risk factors and unhealthy behaviors can increase susceptibility to chronic health issues. Increasing access to resources that can help individuals properly minimize risk factors can aid in the reduction of chronic illness. My Health Compass puts healthy food options, medical resources, education, and community in the path of those with limited access to personal health care. We expect that diet changes, additional exercise, and appropriate education will improve in the community with increased access to resources [13].
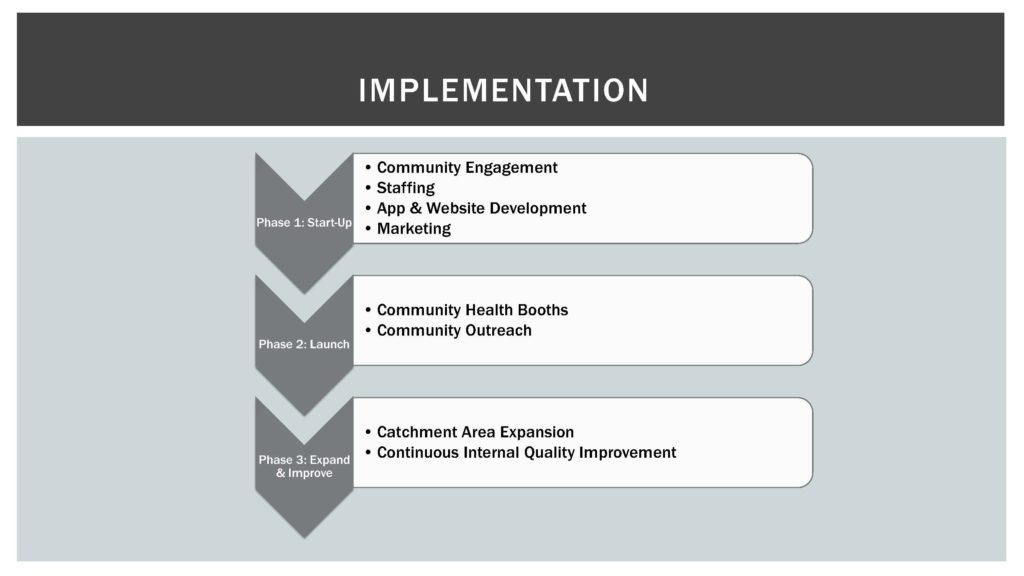
Implementation
My Health Compass will be implemented in three phases (see Figure 5). Phase 1 is the initiation phase, a three-month period centered on community engagement and evaluation, staffing, app/website development, and marketing. Phase 2 is a three- to six-month launch phase, focused on developing community health booths to complement the online program and beginning community outreach programs. The goal of the community outreach programs is to bolster the online resources with physical infrastructure as a means to further increase accessibility and amplify marketing. Phase 3 is a six-month phase of expansion and improvement, focusing on expansion of the program’s catchment area and quality improvement, and development of the software. Phase 3 will be continued to a lesser extent as the program grows and adapts, to maintain appropriate levels of monitoring and evaluation. We estimate the roll-out plan will cost $2 million over a five-year timeline, with approximately $100,000 allocated for discretionary spending.
Figure 5 | Implementation Plan for My Health Compass
The George Washington University
Team members: Mary Bonnell, Ans Irfan, Jennifer Reiner, Puja Sheth, Taylor Tresatti, Amelia Whitman
Statement of Need
Displacement of people and families creates short- and long-term problems for communities. These problems include economic instability, social isolation, and lack of access to services, all of which lead to poor health outcomes, including chronic conditions such as heart disease, autoimmune disorders, and asthma.
Goal
Communities for Collective Action (C4CA) seeks to create a diverse, tight-knit, and inclusive community within each neighborhood that is at risk of urban renewal and displacement, and in neighborhoods with displaced populations by providing the services and support that one needs to lead a healthy and productive life.
Intended Outcomes
C4CA will connect individuals and organizations to resources that will enhance community engagement, encourage activism and advocacy, and promote crosssector collaboration. Through collective action, this intervention aims to increase community connectivity and capacity and, in turn, enact policies that support economic stability, access to services, and diversity.
Intervention
Target population: C4CA seeks to reach three key groups in the DC metropolitan area: low-income minorities, individuals at risk for or affected by displacement, and homeless individuals.
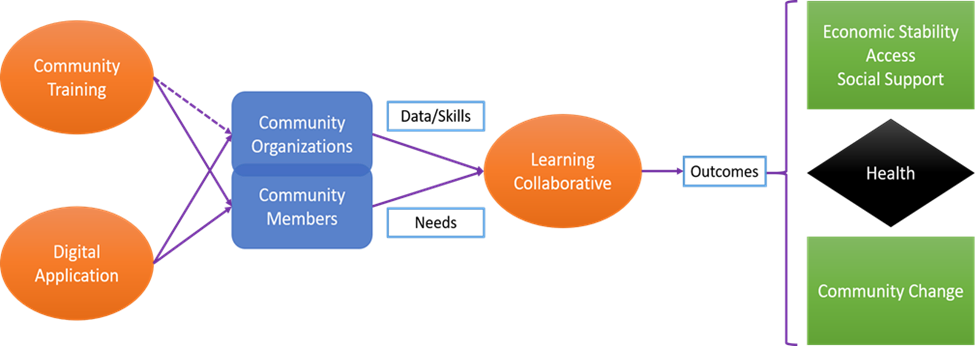
Underlying rationale: C4CA uses community training, a digital application, and a learning collaborative to support our target population. Our rationale for this three-pronged approach (see Figure 6) lies in the belief that community members know their needs and are the best advocates for themselves. However, we recognize that power dynamics (including the interplay of social class, race, and education) may prevent local community voices from being heard. To address this, C4CA focuses on training community members in effective advocacy strategies, fostering cross-sector partnerships across organizations to enhance collaboration, and providing accessible information to facilitate inclusion for displaced populations.
Figure 6 | Overview of Communities for Collaborative Action’s Three-Pronged Approach
Strategy: Digital access: As our communities change, the need to connect becomes more important and more difficult. Digital access is one means of fostering communication and connectedness and reducing social isolation. By connecting community members to resources, information, and perspectives through the online platforms, we hope to increase community connectedness both internally and externally. Features of the application and website include a community forum; a filterable, location-based resource map; an appointment tracker with reminders; and a virtual meeting space where the learning collaborative and other organizations can engage with community members.
Community training: Community training will build community members’ capabilities by providing tools, strategies, and skills to empower them to advocate for their neighborhoods. The training will consist of three sessions that focus on identifying community issues, assets, and resources; developing effective communication strategies; and training and mobilizing other community members. Through these three sessions, participants will learn to strategically frame their own stories to gain support and advocate for changes they need while strengthening connections among community members.
Learning collaborative: C4CA will facilitate a learning collaborative of nonprofit organizations and community members to share and generate knowledge while working together to ameliorate the impacts of displacement. Participation in the learning collaborative will enable nonprofits to further their own missions while strategically aligning their efforts to support communitywide changes. Through these efforts, nonprofits can leverage their collective resources to advocate for local policies that support economic stability, access, and diversity. This will, in turn, improve the health of community members and provide more resources to deal with existing chronic health problems.
Potential partners: Potential partners include the DC government, N Street Village, ONE DC, the Washington Low Income Housing Alliance, the Greater Washington Community Foundation (formerly the Community Foundation for the National Capital Region), the Metropolitan Washington Public Health Association, Empower DC, DC Central Kitchen, Operation HOPE, So Others Might Eat, Community of Hope, Bright Beginnings, Thrive DC, Pathways to Housing DC, and community members themselves.
Potential Barriers and Responses
We recognize that a significant portion of our target population may not have access to a smartphone, a computer, or the internet. To address this, we will partner with organizations in the DC metropolitan area to provide these resources. To address barriers around funding sustainability, we have incorporated into the budget the employment of a development officer, who will procure funding to support the project beyond the first three years. In addition to securing monetary capital for sustainability, C4CA will focus on developing social capital to ensure sustainability. The community training course incorporates a “train-the-trainer” model, which will allow trained community members to lead workshops for others in their community.
Howard University
Team members: Keemi Ereme, Amoge Ezike, Deawodi Ladzekpo, Mark Lorthe, Lavern Smith, Tamea Williams
Goal
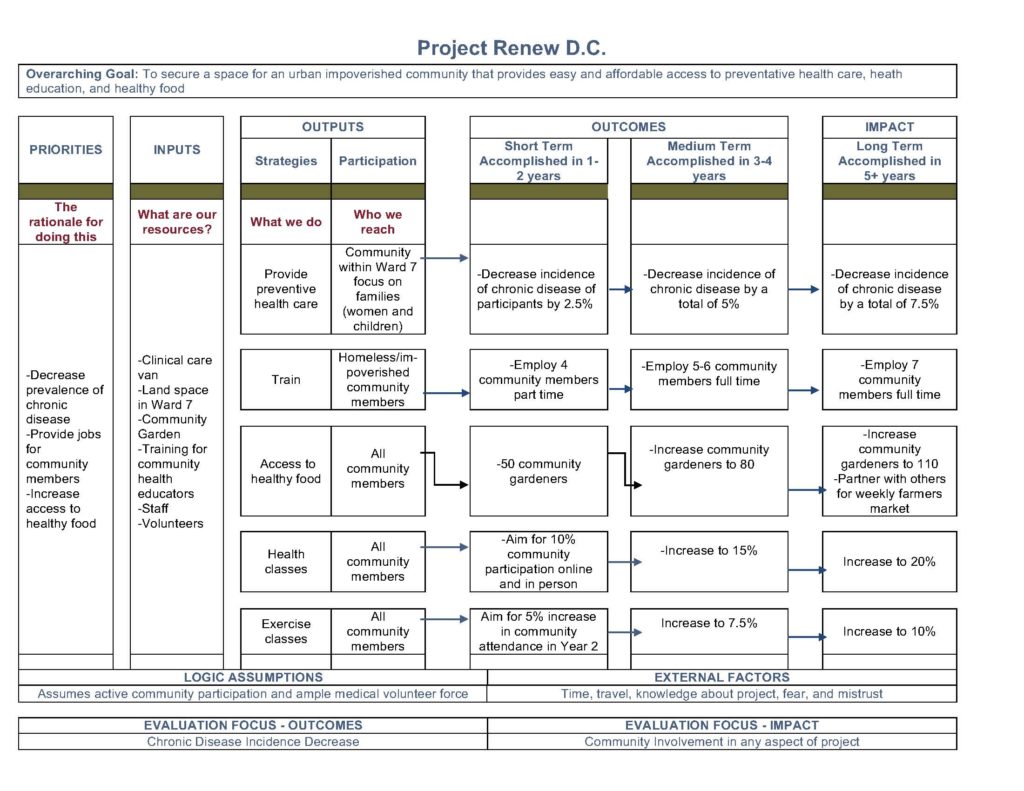
Project Renew D.C. (see Figure 7) is a nonprofit organization that aims to curb the rise of chronic illnesses among the vulnerable population of the Washington, DC, metropolitan area, especially in Wards 7 and 8, through the provision of access to basic health care services and education on health and nutrition. Drawing on the collaborative efforts of student doctors, public health practitioners, staff, and community partners, the organization aims to help people in these communities achieve better physical and mental health.
Figure 7 | Project Renew D.C. Logo
Target Population
With the changes in development and demographics that have swept through Washington, DC, a large portion of its population now faces food scarcity and dwindling access to health care due to relocation. These DC communities (specifically Wards 7 and 8) are composed of elderly, low-income, homeless, and displaced individuals, a disproportionate number of whom are people of color. These individuals also have a higher likelihood for developing chronic diseases. We believe everyone has the right to access the highest standard of health care available. It is therefore imperative that these individuals are provided with health care services.
Intended Outcomes
Project Renew D.C. aims to solve the above-stated problems with a mobile health care clinic and a community garden. The mobile health care clinic is modeled after a similar program in Prince George’s County, Maryland, called Wellness on Wheels, while the community garden program is modeled after the Greater Newark Conservancy. We at Project Renew D.C. think that a health van will be most effective in tackling the problem of access to health care. With a van, we will be able to reach elderly and homebound individuals, residents who work irregular hours, and those who have little or no health insurance. In addition, our community garden will encourage community members to think actively about what they eat and how their diet influences their illnesses and general health.
Intervention
Our project site is located on a 4,000-square-foot plot of land in Ward 7 of Washington, DC. Our intervention encompasses a “PATH” to better health. The PATH mnemonic stands for preventive health care, access to healthy food, training, and health classes. Our project details the pillars of an overall intervention that will work to improve the social determinants of health in this population. Figure 8 shows a logic model detailing the components and target outcomes of the intervention.
Figure 8 | Logic Model for Project Renew D.C.
The implementation of a mobile health van acts as our first pillar of PATH: to provide preventive health care. During the spring, summer, and fall months, the van will be located at our project base and provide OB-GYN, pediatric, and mental health services. The van will be staffed with a paid full-time nurse practitioner as well as volunteer pre-health students, professional health students, and social work students from local universities in Washington, DC. During the winter months, the same services will be available as the van relocates to various preapproved areas in Ward 7 to make care more accessible.
The community garden—the mainstay of our intervention, located on a 3,000-square-foot plot of land within our project site—is another central pillar of PATH and aims to provide access to healthy food. The garden will be open during set hours, Monday through Sunday, and overseen by a manager while open. Groups of families are assigned plots to work in for a minimum of two hours per week and are allowed to take home one bag of produce each week. The program provides all materials necessary to tend to the garden. The garden will grow a selection of vegetables that grow well in the mid-Atlantic climate.
To further facilitate community involvement, the program also has a training pillar of PATH. This pillar aims to train and employ homeless and impoverished youth in the community as health counselors on chronic diseases like diabetes and asthma, as well as on healthy eating. The trained health counselors will work as additional staff at our project site, providing education to community members during set times.
The final pillar of the PATH plan is health classes. The organization will offer exercise, cooking, and health maintenance classes on-site and online to further involve the community in our intervention and to help implement and maintain healthy behaviors.
Outreach: To reach our target community, we plan to advertise Project Renew D.C. through different modalities. We will advertise the program via flyers and tabling events at hospitals, places of worship, grocery stores, homeless shelters, schools, and thrift stores. A second method of advertisement will include bus bench ads. A third method of outreach will include our website, www.projectrenewdc.com. The website will include the mission, hours of operation, and other important details about the program.
Partnerships: The pillars of Project Renew D.C. cannot be fulfilled unilaterally. We intend to partner with free clinics at local medical schools (for example, Howard University’s New Freedmen’s Clinic and Georgetown University’s Hoya Clinic) as well as other student groups at these universities. Project Renew D.C. also intends to partner with local hospitals that serve our target populations. Finally, forming partnerships with other community organizations, such as So Others May Eat, will allow for a larger reach.
Potential Barriers and Responses
Although similar projects have shown successful results, there are limitations. The barriers that we identified center primarily on participation. Specific threats to success include low community member participation in classes and gardening, and unavailability of science student volunteers. To offset these risks, we have implemented several incentives. For our community members, participation in our classes will provide entry into a cash prize raffle drawn every two months, and contributing to the community garden will give them access to a limited supply of free produce. Incentives for health science students are hands-on experience as well as community service hours. Considering the needs of the community and the desire of students to be involved, both parties have much to gain from participation.
Uniformed Services University of the Health Sciences
Team members: Evan M. Gregg, Horace A. Hayes, Alexander J. Leeds, Emad S. Madha, William G. Valiant
Background and Statement of Need
The march of urban renewal in metropolitan domains is not without its drawbacks: While flourishing economic value may engender improvements in public health and commercial opportunity, it may also bring new financial burdens to local populations. The shift of neighborhoods from low to high economic value carries an associated increase in property price and rent, as the influx of more affluent consumers drives up the local price of goods. Original residents may not see a parallel increase in income to compensate for these growing financial demands. As such, the most financially vulnerable are at greater risk of the social and physical hardships associated with
homelessness and displacement.
The consequences of homelessness may be particularly striking for local families, as the loss of domestic stability has a profound effect on the well-being and livelihood of children. Indeed, this loss of stability is correlated with an increase in mental illness and behavioral issues among urban youth. Studies have shown that mental illnesses are more prevalent among youth facing homelessness, with nearly one-third of homeless youth having at least one major mental disorder that interferes with their daily lives. Furthermore, the prevalence of anxiety and depression among homeless youth may be as high as 47 percent, compared with 18 percent in the general population [14]. The amount of homeless youth with issues of delinquency and aggressive behavior reaches 36 percent, in contrast with 17 percent of their counterparts in the general population [14].
Our nation’s capital is not immune to these issues. According to the Washington Legal Clinic for the Homeless, student homelessness increased by approximately 60 percent between 2009 and 2014 [15]. This is not surprising, however, considering that homelessness rates in the District of Columbia (DC) have risen significantly in the last decade: The total number of homeless persons rose by 14 percent in 2015 alone. In 2016 nearly 1,500 families were
homeless in the DC area, an increase of 46 percent since 2012 [16]. The magnitude of both the short- and long-term consequences burdening homeless youth is deplorable and warrants immediate attention. Therefore, we offer
the framework for the Innovative School Program for Individual Resilience and Engagement (InSPIRE) (see Figure 9) as a means to effect positive change and to ameliorate the mental health burdens placed upon homeless youth in
Washington, DC.
Figure 9 | InSPIRE: Innovation School Program for Individual Resiliency and Engagement Logo
Goals and Intended Outcomes
InSPIRE was developed to address the impact of homelessness on the mental health of young students in Washington, DC. The program has been designed with evidence-based therapies aimed at treating mental illnesses prevalent in this population and set for after school to help offset the burden on parents and guardians. Through InSPIRE, we seek to teach students resiliency skills that can help them deal with new issues as well as seek care from mental health specialists to address ongoing needs. The overarching goals of this program include reducing the incidence of mental illness among these children and providing resources, mentorship, and professional assistance in a safe and stable environment.
Methodology and Rationale
Our interventional model for InSPIRE entails a comprehensive and collaborative after-school program. Participants eligible for the curriculum include youth with current or prior status of homelessness. As a pilot program, InSPIRE would first be established at two schools in the DC area chosen based on high rates of homelessness within their student bodies. Two schools in particular exhibited homeless student rates of 18 and 24 percent in 2013 [17]. Focusing on these schools allows us to maximize the cost-to-benefit impact of InSPIRE while targeting student populations in DC with the greatest current need.
The day-to-day influence of InSPIRE will involve a targeted program immediately following the school day and beginning with structured play and activity time. This will occur two and a half days per week throughout the school
year, and promote physical activity while allowing for trust-building between program staff and participating youth. The students would then be involved in a group-based coping skills session lead by trained clinicians. Finally, a nutritious meal would be provided while students engage with local mentoring groups partnered with InSPIRE, further allowing local youth to build stable, one-on-one connections in addition to receiving dietary support. At the conclusion of each session, participating students would then be escorted back to their parents or guardians by a program sponsored bus to ensure safe transportation from school.
To support our program’s efficacy, we use evidence-based practices that also promote the development of meaningful and lasting skill development among participating youth. Regular physical activity has been repeatedly shown to positively influence mental health among children and to reduce existing symptoms of anxiety and depression [18,19,20]. Allowing time for children to play also supports their emotional and social development while letting adult mentors establish trust and familiarity with the students [21]. Our coping skill sessions will draw from established behavioral health practices, including cognitive behavioral therapy. The therapy may be performed in a group setting, and its usefulness in limiting anxiety and depressive symptoms among adolescents is well documented [22,23]. Using techniques from existing coping skills programs with documented effectiveness in improving childhood resiliency will provide additional valid and efficacious techniques [24,25]. Finally, time allocated for mentoring and meals will not only provide students with a healthy meal, but also permit further building of stable relationships with adult mentors, thereby supporting students’ social and emotional development [26]. Ultimately, InSPIRE is intended to impart lifelong skills and self-efficacy to homeless children so that they are adequately protected against the development of chronic mental illness.
Potential Barriers and Responses
Implementing a program like InSPIRE is not without its challenges. Chief among them is the pervasive stigmatization of both homelessness and mental illness. The tragic irony is that the prevalence of these issues in some communities is so high that a child could be eating lunch next to someone struggling with homelessness or mental illness and not even realize it. We aim to dispel misconceptions through public awareness events, school assemblies, and counseling for parents or guardians of prospective candidates for InSPIRE.
Another formidable obstacle to InSPIRE’s success is adequate personnel and resources. Community outreach is key for sustaining the program. With seven area academic institutions offering graduate degrees in medicine, social work, and behavioral health, we foresee an ample supply of qualified volunteers. Partnerships with local organizations already working to achieve similar goals will promise not only resources, but also a wealth of real-world experience and local knowledge. The flexible nature of InSPIRE’s scheduling permits invaluable partnerships involving groups such as Eyes Wide Open Mentoring; United Way of the National Capital Area; the District of Columbia YMCA; Reading Partners of Washington, DC; the AfterSchool Alliance; and DC Hunger Solutions.
Conclusion
The state of homelessness in Washington, DC, is both pressing and concerning, and its effects are particularly notable among urban youth. The consequences of mental illness faced by these individuals are far-reaching and have long-term implications. It is therefore our hope that establishing a program like InSPIRE will limit the hardships young people face. By using evidence-based practices and invaluable local partnerships, this program can equip homeless youth in the Washington, DC, area with skills and resiliency that will benefit them throughout their lives.
University of Maryland, Baltimore
Team members: Anna Alikhani, Breanne Bears, Kimberly Blay, Priya Davey, Douglass Elliott, Jennifer Qian
Statement of Need
Urban changes in DC have led to an increase in chronic disease rates, especially for the most vulnerable and at-risk populations [27,28]. In 2010, 8 of the 15 leading causes of death in DC were due to chronic diseases such as diabetes, asthma, cardiovascular disease, and obesity [29]. Lack of or inadequate health insurance, problems with transportation, reduced access to healthy foods, poor living conditions, and exposure to environmental hazards are some of the factors that may have contributed to increases in chronic disease rates [30].
Goal
Our goal is to use the resources already available in the DC metropolitan area and the passion of young individuals to connect the most vulnerable populations to services needed to live a healthy lifestyle. Our team concept is Community Opportunities for Valuable Residents (COVR)—DC Farmers Market and Wellness Connection. Through COVR, our goal is to advocate for vulnerable families and address the issue of food deserts in urban areas by providing wellness passes that provide access to produce. We hope to implement a plan that inspires policy change. Much like an umbrella provides a shield from the rain, COVR provides a shield to vulnerable populations against the elements that may impede their access to care (see Figure 10).
Figure 10 | COVR: Community Opportunities for Valuable Residents Logo
Intended Outcomes
Our objectives for southeast DC over the next five years are to use the framework of COVR to increase the following: 1) number of people receiving coordinated care services by 10 percent, 2) community access to healthy food in areas with food deserts by 15 percent, and 3) insurance coverage for residents who qualify for Medicaid or Medicare by 5 percent. We project a decrease in chronic disease incidence by 5 percent.
Intervention
Target population: We will connect the vulnerable population to existing medical outpatient clinics, which will help individuals avoid physician’s office wait times. For example, the Elaine Ellis Center of Health and the Anacostia Health Clinic are located in Wards 7 and 8, which represent lower income and have higher chronic disease rates compared with Wards 3 and 4. Despite this, there is significant disparity among income levels in La Clinica del Pueblo, our third location in Ward 3. There is a higher prevalence of Hispanic and Latino and African American individuals moving to this area for lower-income housing [29]. An advantage is that all clinics are positioned for lower-income residents to easily access via Metro lines and bus stations.
Underlying theory and rationale: The Wellness Connection at our three locations aims to connect with residents in accessible locations and provide a direct, in-person resource for information on maintaining a healthier lifestyle. These services cover an interprofessional spectrum, including (1) health insurance signups and housing information, (2) pharmacy counseling and delivery, (3) dentistry resources and appointments, (4) home health education, and (5) legal advice. COVR operates every Monday, Wednesday, and Friday during the day, as this conveniently aligns with existing referral service working hours. The main driving force of COVR is our DC undergraduate student liaisons, as they are passionate and motivated to create change. Professional health fellows oversee undergraduate student liaisons at each center.
For every appointment scheduled by COVR and followed up on by the resident, the resident will receive a wellness pass to be used at COVR’s Saturday farmers market. To address the food desert dilemma and attempt to combat the effects of gentrification, COVR creates an opportunity for all residents to meet and foster community engagement through “Farmers Market and Wellness Connection” Saturdays at LeDroit Park. Residents will have the opportunity to sign up at interactive information booths at the market and engage in special events for children and adults that take place during the first Saturday of each month.
Strategy and mechanism: The advisory board is composed of dentists, physicians, health attorneys, pharmacists, nurses, clinical social workers, and community advocates. This team oversees professional health fellows and undergraduate student liaisons. COVR is nonhierarchical; like a web, community advocates are just as essential as the board members, because the former are most aware of the underserved community’s needs.
The mechanism of COVR follows the logic model [31]. Initial inputs involve obtaining funding for development of materials, staff, and training curricula. Activities include student wellness liaisons referring clients, residents participating in Farmers Market and Wellness Connection events, and liaisons following up with residents. Outputs involve residents gaining access to new resources and healthier foods, and medical professionals developing
an improved understanding of available resources for residents. Our outcomes consist of increasing the proportion of the DC population with access to services that meet basic needs and to healthy food options. Our projected impact is to decrease the rate of people with chronic diseases within Washington, DC, and to increase interaction between residents to foster community support.
Potential partners: To ensure sustainability, we will seek sponsorship and apply for grants. For example, the Social Innovation Fund perfectly fits with COVR’s mission; the fund supports innovative, evidence-based, and effective solutions to challenges in the targeted areas of economic opportunities, healthy futures, and youth development [32]. We would partner with local grocery chains and fitness sponsors, and integrate cooking workshops to build our reputation and attract more volunteers. If our model is successful, we could implement it in other areas in DC, Maryland, and Virginia or even other countries as a longer-term strategy.
Potential Barriers and Responses
Finding an appropriate means to measuring program success is not clear-cut. During years 2 and 3, assessments will be administered to COVR participants to troubleshoot issues and improve the program. Surveys are obtained both in-person after services are rendered and through follow-up by wellness liaisons. Reward incentives used in the farmers market will be calculated and used by the advisory board as a metric to assess wellness booths’ effect and to ensure residents’ needs are being met. This approach to feedback analysis is critical for COVR’s sustainability and success.
Conclusion
Reflections
Solutions developed by the competing teams were innovative and generally included cross-sector partnerships and community participation. Most proposed strategies paired evidence-based interventions with promising new approaches. However, the judges’ questions and comments underscored that the focus for most teams was almost exclusively at the individual level (i.e., individual-level interventions, such as mobile farmers markets or resiliency training) and to a far lesser extent on more upstream interventions (e.g., addressing poverty and lack of affordable housing) needed to support better nutrition and address the challenges faced by community members rendered homeless or displaced by urban change.
Future Plans
The Case Challenge has served to bring the work of the Health and Medicine Division (HMD) to both university students and to the DC community. The NAM and the HMD are therefore committed to continuing this activity with the 2017 (and fifth) DC Public Health Case Challenge, on the topic of “Protecting Young Brains in DC: Tackling Neurologic Risks.” It will be sponsored and implemented by the HMD Roundtable on Population Health Improvement, with the support of the NAM’s Kellogg Health of the Public Fund and the engagement of related activities of the National Academies, including the Global Forum on Innovation in Health Professional Education; the Roundtable on Environmental Health Sciences, Research, and Medicine; the Forum on Promoting Children’s Cognitive, Affective, and Behavioral Health; and the Forum on Neuroscience and Nervous System Disorders. HMD and NAM staff continue to look for new ways to further involve and create partnerships with the next generation of leaders in health care and public health, and with the local DC community through the Case Challenge.
As noted in the reflections above, the solutions brought forward in the Case Challenge do not always consider the complex, but critically important, upstream and multilevel factors that impact health. To address this, the Case Challenge organizers have two approaches planned for the 2017 event. First, they will ensure the ecological model [33] and upstream factors are represented in the case document sent to the competing teams in advance of the event. Second, a webinar will be held before the case is released to the competing teams, to provide the teams with a primer on evidence-based policy solutions for public health issues and to provide an overview of the Case Challenge, best practices, and a question-and-answer period (questions may be asked during the webinar and submitted ahead of time). The webinar will be recorded so that students have future access to it.
References
- Chung, H. 2016. A third of DC children live in a neighborhood of concentrated poverty. DC Action for Children. Available at: http://www.dcactionforchildren.org/blog/third-dc-children-live-neighborhood-concentratedpoverty (accessed May 12, 2017).
- LaMorte, W. W. 2016. The social cognitive theory. Boston University School of Public Health. Available at: http://sphweb.bumc.bu.edu/otlt/MPH-Modules/SB/BehavioralChangeTheories/BehavioralChangeTheories5.html (accessed May 12, 2017).
- Merrill, C., L. Cottrell, and K. Searcy. 2016. District of Columbia community health needs assessment. Washington, DC: District of Columbia Healthy Communities Collaborative. Available at: https://www.dchealthmatters.org/content/sites/washingtondc/2016_DC_CHNA_062416_FINAL.pdf (accessed August 31, 2020).
- Office of Disease Prevention and Health Promotion. 2014. Healthy People 2020. Available at: https://www.healthypeople.gov (accessed August 31, 2020).
- Lurie, N., C. R. Gresenz, J. C. Blanchard, A. Chandra, B. O. Wynn, K. G. Morganti, T. Ruder, A. Price, D. Sickler, B. Norton, K. Jones, M. Regenstein, and B. Siegel. 2008. Assessing health and health care in the District
of Columbia: Phase 2 report. Santa Monica, CA: RAND Corporation. Available at: https://www.rand.org/pubs/working_papers/WR579.html (accessed August 31, 2020). - DC Office of Planning. 2011. Demographic and housing profiles 2010 by ward. Available at: http://planning.dc.gov/node/596612 (accessed May 8, 2017).
- Peer Health Exchange. n.d. About us. Available at: http://www.peerhealthexchange.org/about-us (accessed May 12, 2017).
- The Community Guide. n.d. About the Community Guide. Available at: https://www.thecommunityguide.org/about/about-community-guide (accessed May 15, 2017).
- University of Michigan Health System. 2016. Community health needs assessment report: June 2016. Ann Arbor, MI: University of Michigan Health System and Saint Joseph Mercy Health System. Available at: http://www.med. umich.edu/pdf/2016-Joint-CHNA-Report.pdf (accessed May 18, 2017).
- Town Hall Education Arts Recreation Campus. n.d. Overview. Available at: http://www.thearcdc.org/partners-programs/building-bridges-across-river-bbar (accessed July 25, 2017).
- Grosberg, D., H. Grinvald, H. Reuveni, and R. Magnezi. 2016. Frequent surfing on social health networks is associated with increased knowledge and patient health activation. Journal of Medical Internet Research 18(8):e212. https://doi.org/10.2196/jmir.5832
- Greenwald, R. 2015. Food as medicine: The case for insurance coverage for medically-tailored food under the Affordable Care Act. Presented at Hunger Action Summit, Santa Clara, CA. Available at: http://www.chlpi.org/wpcontent/uploads/2013/12/CA-Greenwald-HungerSummit-1-26-15.pdf (accessed May 12, 2017).
- Centers for Disease Control and Prevention. 2015. The four domains of chronic disease prevention: Working toward healthy people in healthy communities. Atlanta, GA. Available at: https://www.cdc.gov/chronicdisease/pdf/
four-domains-factsheet-2015.pdf (accessed May 4, 2017). - Hart-Shegos, E. 1999. Homelessness and its effects on children. Minneapolis, MN: Family Housing Fund. Available at: https://shnny.org/uploads/Homelessness_and_Its_Effects_on_Children.pdf (accessed August 31, 2020).
- Eyes Wide Open Mentoring. n.d. Our mission & program. Available at: http://www.ewomentoring.org/our-program.html (accessed October 13, 2016).
- Kurzius, R. 2016. Report: D.C. homelessness increased by 14 percent since 2015. DCist. Available at: http://dcist.com/2016/05/homelessness_increases_in_dc.php (accessed October 21, 2016).
- DC Alliance of Youth Advocates. n.d. DCPS releases chart on DC homeless student enrollment. Available at: http://www.dc-aya.org/news/dcps-releases-chart-dc-homelessstudent-enrollment (accessed October 21, 2016).
- Ahn, S., and A. L. Fedewa. 2011. A meta-analysis of the relationship between children’s physical activity and mental health. Journal of Pediatric Psychology 36(4):385-397. https://doi.org/10.1093/jpepsy/jsq107
- US Department of Health and Human Services. 2008. 2008 physical activity guidelines for Americans. Washington, DC. Available at: https://health.gov/our-work/physical-activity/previous-guidelines/2008-physical-activity-guidelines (accessed August 31, 2020).
- Nieman, P. 2002. Psychosocial aspects of physical activity. Paediatrics & Child Health 7(5):309-312. https://doi.org/10.1093/pch/7.5.309
- Ginsburg, K. R. 2007. The importance of play in promoting healthy child development and maintaining strong parent-child bonds. Pediatrics 119(1):182-191. https://doi.org/10.1542/peds.2006-2697
- Anxiety and Depression Association of America. n.d. Treatment. Available at: https://www.adaa.org/living-withanxiety/children/treatment (accessed October 13, 2016).
- Seligman, L. D., and T. H. Ollendick. 2011. Cognitive-behavioral therapy for anxiety disorders in youth. Child and Adolescent Psychiatric Clinics of North America 20(2):217-238. https://doi.org/10.1016/j.chc.2011.01.003
- Mishara, B. L., and M. Ystgaard. 2006. Effectiveness of a mental health promotion program to improve coping skills in young children: Zippy’s Friends. Early Childhood Research Quarterly 21(1):110-123. Available at: https://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.519.5826&rep=rep1&type=pdf (accessed August 31, 2020).
- University of Pennsylvania Positive Psychology Center. n.d. Resilience in children: The Penn Resilience Program for middle school students. Available at: https://ppc.sas.upenn.edu/research/resilience-children (accessed October 13, 2016).
- California Department of Education. n.d. Social emotional development domain: California infant/toddler learning & development foundations. Available at: http://www.cde.ca.gov/sp/cd/re/itf09socemodev.asp (accessed October 13, 2016).
- Partnership to Fight Chronic Disease. n.d. Partnership to Fight Chronic Disease. Available at: http://www.fightchronicdisease.org/ (accessed September 22, 2017).
- DC Cancer Registry. 2014. Burden of cancer in the District of Columbia. Washington, DC: DC Department of Health. Available at: https://dchealth.dc.gov/sites/default/files/dc/sites/doh/DOH_BurdenOfCancer_V5.pdf (accessed August 31, 2020).
- DC Department of Health. 2014. District of Columbia community health needs assessment: Volume 2. Washington, DC. Available at: https://dchealth.dc.gov/page/dc-community-health-needs-assessment (accessed August 31, 2020).
- National Academy of Medicine. 2016. Urban Change and Impact on Chronic Disease of Vulnerable Populations in DC. Available at: https://nam.edu/wp-content/uploads/2016/10/2016-DC-Public-Health-Case-Challenge.pdf (accessed August 31, 2020).
- Community Tool Box. n.d. Section 1: Developing a logic model or theory of change. Available at: http://ctb.ku.edu/en/table-of-contents/overview/models-for-communityhealth-and-development/logic-model-development/main (accessed May 8, 2017).
- Corporation for National and Community Service. n.d. About the Social Innovation Fund. Available at: https://www.nationalservice.gov/programs/social-innovation-fund (accessed May 8, 2017).
- Institute of Medicine. 2003. Who Will Keep the Public Healthy?: Educating Public Health Professionals for the 21st Century. Washington, DC: The National Academies Press. https://doi.org/10.17226/10542