Eighth Annual DC Public Health Case Challenge: Addressing Infectious Diseases Using a Population Health Approach: Prevention and Control of Bacterial Sexually Transmitted Infections in Young Adults 18-24
This discussion paper provides an overview of the eighth annual District of Columbia (DC) Public Health Case Challenge (https://nam.edu/initiatives/dc-public-health-case-challenge/), a competition held in 2021 by the National Academy of Medicine (NAM) and the Roundtable on Population Health Improvement in the Health and Medicine Division of the National Academies of Sciences, Engineering, and Medicine (the National Academies). The Case Challenge, which is both inspired by and modeled on the Emory University Global Health Case Competition, is designed to promote interdisciplinary, problem-based learning in public health and to foster engagement with local universities and their surrounding communities. The event brings together graduate and undergraduate students from multiple disciplines and universities to promote awareness of and develop innovative solutions for 21st century public health challenges as experienced by the DC community. (See https://globalhealth.emory.edu/students/case-competitions/index.html).
Each year, the organizers and a student case-writing team develop a case based on a topic that is relevant to the DC area but also has broader national and, in some cases, global resonance. Content experts are recruited as volunteer reviewers of the case. Universities located in the Washington, DC area are invited to form teams of three to six students, all of whom are enrolled in undergraduate or graduate degree programs. In an effort to promote public health dialogue among a variety of disciplines, the competition requires each team to include representation from at least three different schools, programs, or majors.
Two weeks before the Case Challenge event, the case is released and teams are charged to employ critical analysis, thoughtful action, and interdisciplinary collaboration to develop a solution to the problem outlined in the case. On the day of the competition, teams present their proposed solutions to a panel of judges, composed of representatives from DC organizations and other subject matter experts from relevant disciplines. The prize categories vary by year, but generally include a grand prize as well as awards for practicality and interdisciplinary solutions. In 2021, a wildcard prize was also awarded.
2021 Case: Addressing Infectious Diseases Using a Population Health Approach: Prevention and Control of Bacterial Sexually Transmitted Infections in Young Adults 18-24
The 2021 case focused on addressing infectious diseases using a population health approach. The case asked the student teams to develop a program that, with a fictitious grant of $2.5 million over five years, would prevent and/or control the transmission of bacterial sexually transmitted infections (STIs) in 18–to 24-year-old young adults in DC. Each proposed solution was expected to outline a rationale, an intervention, an implementation plan, a budget, and an evaluation plan.
STIs have been, and continue to be, a significant but underresourced public health concern, with reportable STIs rising for the last decade (NASEM, 2021). Adolescents account for 50% of STIs in the United States, although they represent only 25% of the sexually active population (CDC, 2021a). STIs are often asymptomatic, especially in women. When untreated, STIs can lead to poor health outcomes that include infertility, chronic pain, and cancers.
The case framed the issue through three scenarios, illustrating a range of issues faced by adolescents in DC that may affect exposure to STIs and access to testing and treatment. Though the three illustrative scenarios were fictional, they drew from circumstances faced by DC residents, with an emphasis on the conditions most relevant to health outcomes: racism, bias, and the social determinants of health (e.g., access to health care, transportation, financial stability).
The teams were provided with background information on: public health models, including the tiered model of public health prevention and the social ecological framework (Bronfenbrenner, 1977; IOM, 2003); surveillance; DC’s eight wards, including historical disparities among the wards as well as demographics and relevant health disparities in DC; viral and bacterial STIs; priority populations; national STI data; biomedical prevention tools, including testing, condoms and other barrier method contraceptives, and HIV PrEP; drivers of STIs and structural inequities related to education, employment, income, housing, transportation, the health care system, and confidentiality; community, policy, structural, and psychosocial interventions; and the role of technology, data, and media. (For the background information and guide provided to the competing teams, see https://nam.edu/wp-content/uploads/2021/10/2021-DC-Public-Health-Case-Challenge_FINAL.pdf).
Team Case Solutions
The following brief synopses, prepared by students from the seven teams that participated in the 2021 Case Challenge, describe how teams identified a specific need in the topic area, how they formulated a solution to intervene, and how they would implement their solution if they were granted the fictitious $2.5 million allotted to the winning proposal (budgetary information not included). The U.S. Naval Academy team was unable to compete on the day of the competition, but the team prepared a proposal and summary for this paper. Team summaries are provided in alphabetical order according to university name.
The 2021 Grand Prize winner was the team from the Uniformed Services University. Three additional prizes were awarded: the Harrison C. Spencer Memorial Interprofessional Prize, to the team from American University; the Practicality Prize, to the team from Georgetown University; and the Wildcard Prize, to the team from Howard University.
American University: SexifyDC
Team members: Olivia Gonyea, Yongyi Lu, Anita Novillo, Jessie Sadel, Kai Wasson, and Aria Wanek
Summary prepared by: Jessie Sadel, Kai Wasson, Aria Wanek, Yongyi Lu, and Olivia Gonyea
Faculty Advisor: Melissa Hawkins
Statement of Need and Goals
Historically, STIs have been shrouded in shame and blame on the individual level, contributing to the hesitancy of individuals to access STI testing and treatment (Cunningham et al., 2009; Fortenberry et al., 2002; NASEM, 2021). To address this stigma, SexifyDC aims to provide a mechanism for DC young adults —the population with the highest case rates for chlamydia and gonorrhea (CDC, 2021a)—to receive routine STI testing as a part of their overall preventive health care. Via an interactive mobile app, mobile testing with a linkage to treatment, and a peer facilitator system, SexifyDC aims to reinforce STI testing and care as a component of holistic health and to destigmatize STIs among the target population. The long-term goal of the initiative is to decrease the rates of gonorrhea and chlamydia among 18–24-year-olds in DC.
Intended Outcomes
SexifyDC is an interdisciplinary, multi-pronged initiative that aims to connect with the target population through mobile van presence, online communities, and peer relationships. Short-term outcomes include connecting the target population with local peers to ignite conversations around STIs, engaging with existing resources and community partners, cultivating health education and increased knowledge of sexual health, initiating individuals into the health system through initial STI testing, and identifying STI infection early, followed by providing linkages to care. Mid-term outcomes include the development of a support care network with local DC residents, including a digital space to serve as a place to build community capacity to maintain health and collective well-being, and increased awareness of the importance of STI testing and routine care. Long-term outcomes include an increased understanding of the prevalence and significance of bacterial STIs by the target population. The intervention includes a mobile app that allows users to experience increased self-efficacy to maintain their health and well-being, leading to a healthier overall population and lower rates of bacterial STIs among 18-24-year-olds in the District.
Intervention
Target population: As bacterial STIs are prevalent across the eight wards and the age group of 18-24-year-olds, SexifyDC did not choose a subgroup or geographical location as the target population in order to maximize the reach and scope of the intervention. Because the intervention involves a social networking health app, SexifyDC was created to be easily accessible in all areas of the District.
Underlying theory: SexifyDC is driven by interdisciplinary guiding principles: holistic accessibility (including physical, informational, and emotional dimensions) and health equity (including historical contextualization and prioritizing those most impacted). The principles are intended to ensure that the project addresses the needs of the target population, and that it is guided by a comprehensive logic model that encompasses planning, implementation, evaluation, and communication processes. Social Cognitive Theory is the primary theoretical framework (McLeroy, 1988). SexifyDC draws upon components of the Social Ecological Model (IOM, 2003) to integrate socio-structural factors with self-efficacy and behaviors. The intervention also focuses on the social determinants of health to guide its effective implementation, from its modality to its reach. Finally, it uses the sociological theory of Social Network Analysis to explain how a user-focused approach to a public health intervention provides benefits to the broader population.
Mechanism: SexifyDY employs an interconnected three-pronged approach, consisting of a mobile application, SexifyDC peer facilitators, and linkage to testing and treatment. The first prong is the SexifyDC phone application—a DC-based networking app that engages 18–24-year-olds. Users can create a profile to meet and network with other DC individuals. The app also integrates a peer facilitator model (external to the health care system) to provide a resource for sexual health education and STI information. The application serves to destigmatize sexual health and allow for easily accessible information right at the fingertips of the target population. The second prong is a group of peer facilitators who serve as comprehensive sexual health experts that disseminate sexual health information through community outreach. These individuals can provide sexual health counseling either one-on-one or in group settings. Peer facilitators will be deployed, with a focus on recruitment in areas where DC’s STI rates are highest. The third prong is testing and treatment. SexifyDC will establish a collaborative partnership with the DC Department of Health (DC Health) to facilitate access to self-test bacterial STI kits at no cost. Pop-up testing events will allow those connected through the SexifyDC app to administer a self-test and receive results through the app. Should an individual test positive, they will be linked to the DC Health and Wellness Center, where virtual appointments can be scheduled to prescribe antibiotics. Research has shown that digital interventions have a moderate effect on sexual health knowledge and a positive effect on sexual behavior (Bailey et al., 2015). In addition, mobile community-based STI screening and treatment is feasible, could identify high positivity of STIs, and is accepted by the community as an innovative approach to STI control (Kahn, 2003). Peer educators will help to increase knowledge about sexual health, and have been shown to create some behavior change, such as increased condom use and HIV testing (Wong et al., 2019).
Potential partners: A variety of DC-based partners will help foster the initiative and allow for seamless interfacing with the target population. DC Health will provide the self-test bacterial STI kits for the mobile testing events and will also provide the results for patients. This partnership is crucial for the feasibility of the intervention, especially since DC Health is an established and credible organization. Similarly, a partnership with the DC Health and Wellness Center will efficiently connect patients to treatment. The Wellness Center provides virtual appointments and antibiotic prescriptions. Another partner, One Tent Health, currently provides HIV testing throughout DC. SexifyDC will expand upon One Tent Health’s existing infrastructure by modeling their testing process, volunteer training guide, and testing locations. Lastly, a partnership with DC Public Schools will introduce the intervention to high school students to start the conversation about sexual health, help to destigmatize the issue, and familiarize students with available resources.
Potential Barriers and Responses
There are several barriers to the SexifyDC initiative. To ensure that users download and sign up with the SexifyDC app, the app, and its benefits, will need to be promoted and explained on other platforms, at DC health clinics, and at DC public schools. Secondly, since the age group of our target population is between 18 and 24, some of the individuals in the target group might not have access to smartphones. To address this gap, the intervention will connect individuals to partners such as DC Get Checked and the DC Health and Wellness Center to obtain STI testing kits directly. Finally, considering the high cost of SexifyDC’s development, the DC Department of Health will take ownership of the chlamydia and gonorrhea mobile testing intervention after a 5-year period.
George Mason University: DC SHOE (Sexual Health Outreach Education)
Team members/summary prepared by: Sara Alemayehu, Jorge Luis Garcia, Jordan Hunter Jones, Jessica Lammers, Marichamnan Po, and Sara Yousuf
Faculty Advisor: Ibrahim Kargbo
Statement of Need and Goals
Sexually transmitted bacterial infections are on the rise nationally, and especially in Washington, DC. The goal of this upstream-focused intervention is to design a program that will effectively reduce the incidence rate of bacterial STIs in 18–24-year-olds.
Intervention
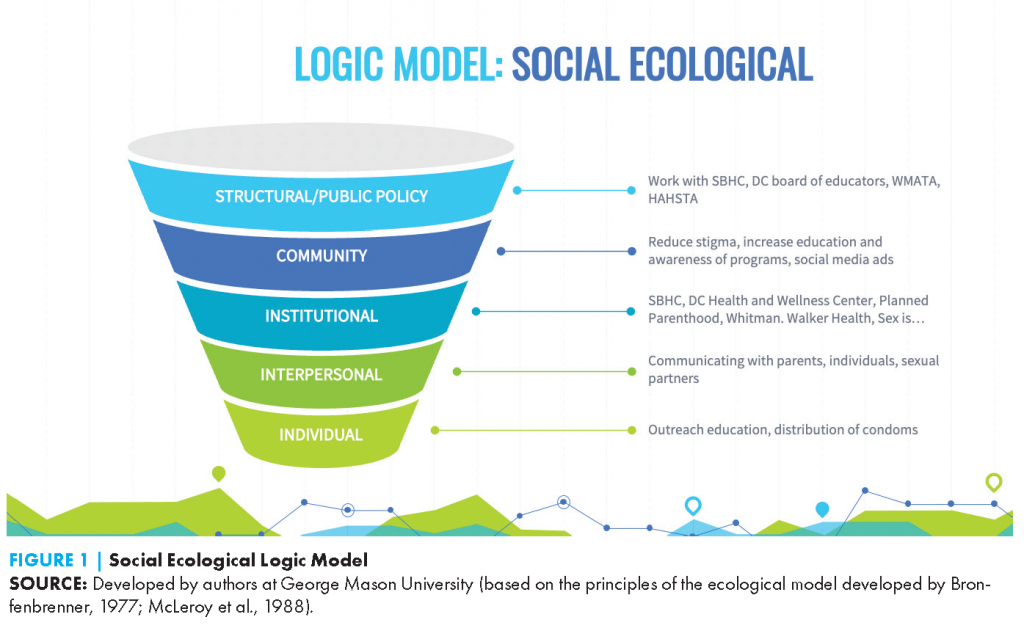
DC Sexual Health Outreach Education (DC SHOE) provides sexual health education for 18-24-year-olds in Washington, DC through a multifaceted approach, including a sexual health hotline to answer questions anonymously and connect people with needed resources, providing staffing at community health fairs, providing outreach in areas of high STI prevalence, and promoting and staffing a mobile STI testing van. The intervention—led by fi ve highly-trained community health workers—is guided by the social ecological model with intervention points at the interpersonal, intrapersonal, community, and public policy level (see Figure 1). DC SHOE will be marketed via social media, dating apps, Washington Metropolitan Area Transit Authority, and paper ads posted in libraries, schools, and community centers.
Outreach specialists will work with established and trusted community partners that serve as gatekeepers in the community. The emphasis will be on partnering with the DC Department of Health and school-based health centers across DC to promote healthy sexual behaviors and provide condoms. Outreach specialists will promote existing programs that have been effective, such as the expedited partner therapy campaign, and will train health providers in cultural competence to better serve the community. Primary care facilities that join the Gay and Lesbian Medical Association and participate in continuing education are eligible for a yearly grant from the outreach team.
Data collected by the outreach team would be used by the DC health department epidemiology team to guide potential locations for the mobile van. Additionally, data collected on resident addresses will allow DC SHOE to provide express bus routes to health clinics for routine STI testing and services.
Intended Outcomes
The main outcome is reducing the incidence of bacterial STIs among 18–24-year-olds in DC. Other desired outcomes are to increase the number of individuals with knowledge of STI resources and to improve trust with the community. This will be measured by monitoring calls to the hotline, trips to the mobile van, and the number of events attended by the outreach team.
Potential Barriers and Responses
The hotline may be inundated with prank calls or messages. Staff would be equipped to handle such messages and trained in de-escalation. This training will also be useful when working with parents or community members who do not support the curriculum. Additionally, the mobile clinic may receive negative attention at first, but through continued exposure in the community it will likely become accepted.
Georgetown University: SHAPE DC
Team members/summary prepared by: Carolina I. Andrada, Elaine Chen, Cat Gardiner, Chloé Jammes, Miller Richmond, and Agrata Sharma
Faculty Advisor: Anne Rosenwald
Statement of Need and Goals
Sexual Health Awareness, Prevention and Education (SHAPE) DC is a young adult sexual wellness project centered on inclusive clinical care and community empowerment to address bacterial STIs in DC’s Wards 7 and 8. The intervention targets 18–24-year-olds in these locations as these wards have disproportionately higher rates of bacterial STIs than other wards in the District. Several social determinants of health contribute to these disparities: limited access to transportation, lower health literacy, financial instability, limited awareness of resources, low trust, and discrimination. SHAPE DC aims to address each of these determinants of health and reduce bacterial STI rates in 18–24-year-olds by 1) empowering community members to advocate for change, 2) training providers on cultural competency and LGBTQ+ health, and 3) providing empathetic care in preventative care and treatment for chlamydia, gonorrhea, and syphilis.
Community Empowerment
SHAPE DC seeks to address some of the long-term, systemic drivers of high STI rates in Wards 7 and 8 by prioritizing community outreach and youth-based advocacy. The approach is to engage the community, build a forum for public discourse on young adult sexual wellness, and empower young adults to become advocates for policy change. SHAPE DC will establish and manage two councils—the Youth Council and the Community Council—that will serve as places to convene members of Wards 7 and 8 for idea sharing and feedback. The Youth Council supports young adults from Wards 7 and 8 with an interest in representing their communities. The Youth Council will convene monthly for discussion and feedback, and will be supported and trained by DC-based advocacy professionals who specialize in grassroots advocacy and policy change. It will also have an LGBTQ+ focus group for queer young adults to share their unique experiences to inform sexual health policy needs. The Community Council will include Youth Council members, trusted community leaders such as religious leaders and former high school faculty and staff, and local health care professionals. The primary goal of the Youth Council is to support and empower young adults to become strong advocates for themselves and their communities, and the primary goal of the Community Council is to convene stakeholders to promote understanding across different perspectives and provide community-based direction for the organization’s programming.
Clinician Partnership and Training
It is possible that DC clinical services will be unable to treat all of the youth in the target community. To expand the reach of SHAPE DC, the initiative will develop a partnership and training program with local clinicians focusing on improving cultural competence and LGBTQ+ care. These areas are often overlooked in medical education, which results in worsening health disparities (NASEM, 2021). The programming will use HHS courses and currently available virtual webinars providing CME credit. SHAPE DC will also form partnerships with DC thought leaders and hold in-person educational workshops specifically focused on treating and preventing STIs in the target population, with the goal of decreasing health disparities. To evaluate the training initiatives, SHAPE DC will survey providers and conduct patient satisfaction questionnaires.
Clinical Services
SHAPE DC will provide various clinical services, including patient navigation services, access to community health workers, a mobile clinic, and transportation services to improve access to health care.
Patient navigation services: Community health workers (CHWs) will process referrals, perform initial outreach, and schedule clinic visits for patients. CHWs will also use telehealth platforms, such as VSee, to set up virtual meetings with patients referred to SHAPE DC for STI education, with the goal of improving health literacy and increasing resource awareness before the patient receives symptomatic testing or screening. Finally, CHWs will perform warm handoffs when connecting patients with community services. CHWs will have critical roles in promoting sexual health and education, coordinating care (such as connecting patients with existing health resources), and addressing social needs. The patient navigation and support component of the intervention will be evaluated through various performance metrics, including rates of patient contact, patient follow-up, and improvements in patient outcomes (e.g., STI recurrence).
The SHAPE clinic: In the first two years of the program, a partnership with GetCheckedDC (Washington, DC’s home-based testing program) will allow for free at-home testing kits for chlamydia and gonorrhea; provide van transportation from the program’s headquarters to the LabCorp location in Ward 8 for syphilis blood draws, chlamydia and gonorrhea swabs, and urine testing; and provide referrals to treatment at a partner health care facility in Ward 8: Family and Medical Counseling Service, Inc. Clinical services will be phased in and will focus on community outreach and provider training. Transportation is an integral part of this plan because public transportation is sparse in DC’s Wards 7 and 8, compared to other wards, and there are not many easily accessible health care facilities. The partnership with Family and Medical Counseling Service, Inc. will provide staff for the mobile clinic (Mission Mobile Medical, 2021). Mobile clinic services will include chlamydia, gonorrhea, and syphilis screening/testing, counseling with in-house culturally competent community health workers on STI prevention, and antibiotic treatment for positive cases.
Barriers and Responses
Some barriers that SHAPE DC might face include: long-term project sustainability, distrust and miscommunication, retention and recruitment of talent, and political interference. The majority of SHAPE DC’s expenses go towards salaries as opposed to other expenses, and SHAPE DC plans to work with other organizations in the future to share administrative costs. Mistrust of health care providers and the health system in general can be addressed with input from CHWs, the Youth and Community Councils, and local organizations. Recruitment and retention of skilled workers will be addressed through incentives or a rotation-based system. Incentives are more costly, but allow for longer-tenured employees, while a rotation-based system costs less but requires more focus on training, as newer employees will cycle in on an ongoing basis.
Political interference can be addressed by the Youth and Community Councils. Long-term planning is difficult in a location like Washington, DC. Even when alert to local ordinances and changes, federal politics can allow or disallow elements of the project with little warning. It is important to keep abreast of what is happening at the federal government level to protect the core elements of the project and keep it functioning.
The George Washington University: Creating Opportunities for Virtual Exposure to Resources in DC (COVERDC)
Team members/summary prepared by: Rita Aidoo, Eun Kyeong (Grace) Jeong, Elizabeth Mason, Samantha Mielke, and Emerald O’Brien
Faculty Advisors: Gene Migliaccio, Jen Skillicorn, Geralyn Johnson, and Victoria Larsen
Statement of Need and Goals
In comparison to other states, DC has the highest prevalence of chlamydia in males and females, highest prevalence of syphilis amongst all adults, highest prevalence of gonorrhea in males, and second highest prevalence of gonorrhea in females (CDC, 2019). Many health care organizations in DC are deeply connected to the community and provide STI screening, testing, and care, but the current mechanisms that link young adults to care are inadequate. Young adults are not adequately utilizing existing resources and the bacterial STI prevalence continues to rise in DC. The goal of COVERDC is to reduce the prevalence of STIs from 2,771 to 2,632 cases per 100,000 by 2027 (a 5% reduction) and from 2,771 to 2,494 cases per 100,000 by 2032 (a 10% reduction) (Healthy People 2030, 2020).
Intended Outcomes
The primary outcome is to reduce the prevalence of chlamydia, gonorrhea, and syphilis by 5% over the five-year grant period (Healthy People, 2020). This includes:
- Reducing the prevalence of chlamydia by 5%, from 4,712 to 4,476 per 100,000.
- Reducing the prevalence of gonorrhea by 5%, from 1,445 to 1,373 per 100,000.
- Reducing the prevalence of syphilis by 5%, from 42.8 to 40.6 per 100,000.
Target Population
The target population is all DC young adults, aged 18–24, as this is the population with the highest prevalence of STIs nationally (CDC, 2019).
Underlying Theory and Rationale
Young adults in DC need customizable, readily accessible, comprehensive care for sexual health. COVERDC aims to answer the following questions among its target population: What do young adults need to know and where do they need to go? The program will use a multi-pronged approach, centering on a smartphone application to increase access to education, social services, and testing. The education component will lead to increased screening and testing, offer education on safe sex practices, and provide information about STIs and treatment options. The testing component will lead to treatment if needed, which will hopefully ultimately lead to a decrease in incidence of STIs. The initiative will also increase access to social support that addresses the upstream determinants of health, which can pose significant barriers to accessing care.
COVERDC employs the social ecological model, which examines the interplay between individual, relationship, community, and societal factors to explain health outcomes (CDC, 2021d). The framework helps understand the range of factors that put young adults in DC at risk for contracting bacterial STIs and how the barriers to care can be addressed (see Figure 2).
The initiative will also apply social marketing theory in the development of the smartphone application and in the implementation phase of the campaign, with the goal of advertising and marketing leading to increased app usage.
Strategy
COVERDC is a radically inclusive, personalized, smartphone application that will act as a one-stop shop for sexual health, mental health, and social care. The application is inspired by Aunt Bertha, an online directory of social service organizations designed to consolidate health and social services in DC (DC Health Matters, 2021; Link U, 2021). The application will provide appropriate care through an innovative approach as it improves and enhances how young adults are connected to the resources they need for testing, screening, and care. The goal is for all young adults in DC to understand what they need to know and where they need to go. COVERDC is a discrete, readily accessible innovation that will directly link young adults to the education, health care, and social services they need to live a healthier life. The application aims to address all levels of the social ecological model, engages directly with the target population and partners from day one, and leverages innovative technology to make it accessible for anyone and everyone in DC.
Potential Partners
COVERDC will partner with organizations from a range of sectors beyond the health care system. When users engage with the app, they will earn points that can be redeemed at stores such as Giant Foods and Goodwill, or for transportation services through WMATA. The initiative will leverage community outreach and corporate responsibility activities to incentivize partnering organizations to collaborate with COVERDC, resulting in a sustainable model for continued and expanded partnerships.
Potential Barriers and Responses
There are many structural barriers that prevent young adults in DC from accessing screening, testing, and care for STIs, including the lack of readily accessible, comprehensive, intersectional information on STIs and sexual health, and privacy and confidentiality concerns. These barriers will be addressed by applying the social ecological framework. In addition, while the ownership of mobile devices is high in DC, not everyone in the target population will have a phone. Therefore, a total of 400 iPads will be purchased in the program’s first year and placed in hotspots where the target population is found (i.e., the DC public library, where many unhoused young adults go to use computers). This will allow as many young adults as possible to utilize the innovation to seek care.
One limitation of COVERDC is the inability to follow up with individuals regarding STI testing status via the app. The app is not set up to be an electronic medical record due to concerns of HIPAA compliance. For this intervention, however, it is more effective to get young adults tested by partnering with clinics and sites that are already HIPAA-compliant.
Howard University: UMOJA Health
Team members/summary prepared by: Carizma Forbes, Charnae Henry-Smith, Marcus Mcintyre, Adaeze Okoroajuzie, and Chantay Moye
Faulty Advisor: Monica Ponder
Background/Statement of Need and Goals
Current sexual health campaigns lack an intersectional approach, which can widen health disparities. This initiative consists of the development of a comprehensive health app named UMOJA (unity), which seeks to provide information to college students to support their knowledge of STIs and facilitate access to care. UMOJA utilizes the slogan “Talk to Me,” and focuses on the lack of patient-centered and customer-service-oriented care for STIs. The intervention also includes a comprehensive cultural analysis to address the roots of STI-related stigma (including purity culture, taboos around sex education, and hyper-sexualization of marginalized communities), and partnerships with local providers and other organizations relevant to college students.
The all-inclusive UMOJA app provides community resources, virtual events, intimate partner violence (IVP) education, access to health care professionals, and virtual appointments. The intervention uses resources from the community to establish and sustain an effective and inclusive system. Although there are numerous resources already offered to the intended target population in DC, they are not always utilized, due to reasons of accessibility, comfort, and confidentiality. Intervention efforts will focus on whether the app is suitable for the target audiences (i.e., DC residents ages 18–24, and especially residents of marginalized communities). In focusing on this specific demographic, the intervention team felt it was important to create a campaign that stood out from other current sexual health campaigns.
Intended Outcomes
The intended outcome is to address the following issues for the target audience:
- accessibility,
- confidentiality,
- response time for results, and
- customer service.
Ethnographic qualitative analysis will be used to obtain feedback and input from this demographic on STI prevention and treatment.
Timeline
In year one, the program will establish partnerships and hold pop-up shops (see the interventions section for more information). During year two the aim is for the UMOJA app to be used by 50–100 young adults and for pop-up shops to be conducted bi-monthly. Year three will focus on collecting data from previous years and utilizing these insights to improve the intervention. In year four the UMOJA app will be used on at least two college campuses and activities will be held to increase attendance at the pop-up shops. By year five the goal will be to sustain community cohorts throughout ongoing partnerships, and expand the intervention to all DC residents ages 18–24.
Interventions
To test the effectiveness of the intervention, it will first be implemented where the intended demographic is prevalent—a college campus. Gender imbalance, combined with high-risk sexual behaviors exhibited by college students in general, provided the rationale of testing this system on a college campus. STIs present serious health concerns among the campus community, and they also negatively impact students’ overall health and therefore ability to focus on their studies. In order to understand the drivers of increased STI incidence among historically marginalized and racialized communities, an intersectional approach to public health intervention design is needed. By asking questions such as “What is intimacy?” and “What are the taboos of sex education?”, UMOJA’s implementation plan gets to the root of the problem.
A “pop-up shop” is a short-term fair or event that lasts for one day. This intervention will occur on a monthly basis to allow the intended audience to discuss sex positivity and access sexual health resources. These pop-up events and other activities will use well-known pop culture figures to target the intended audience. The intervention team will also partner with DC organizations including One Tent Health, Community of Hope, Planned Parenthood, DC HealthLink, and Slutty Vegan (restaurant pop-ups).
Potential Barriers
The main potential barrier for this intervention is traffic and accessibility of the app by the intended demographic. Initiating this plan on a college campus grants the ability for improvement, feedback, and changes to better serve the DC community.
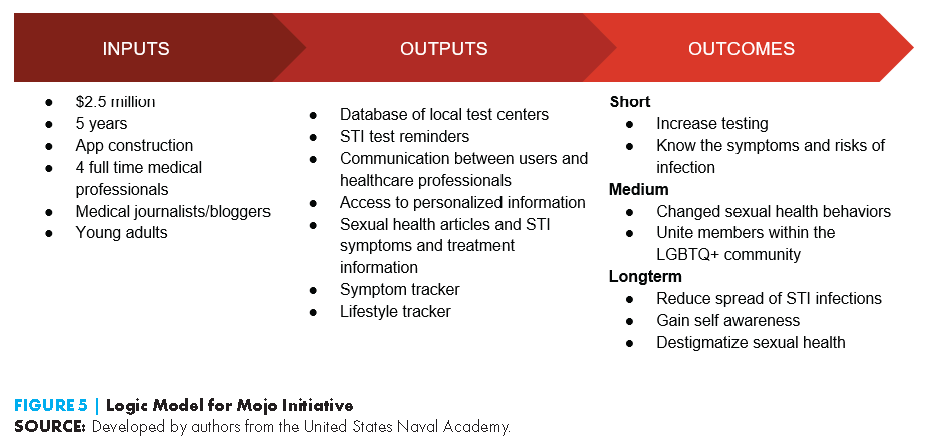
United States Naval Academy: Mojo Initiative—Don’t Let STIs Slow Your Mojo
Team members/summary prepared by: Ainslee Gabriel, Kelly Hughes, Yusuf Mousa, Faith Southwick, and Sarah Yo
Faculty Advisors: Christopher Kinter and Chelsea Snyder
Statement of Need
Structural inequities have led to large gaps in education on the treatment and prevention of bacterial STIs, leaving many of Washington DC’s young adults vulnerable and susceptible to infection. The proposed initiative aims to reshape the method of STI education, allowing for a broader audience regardless of social determinants of health.
Goal/Intended Outcomes
This digital initiative provides an educational baseline and a dynamic platform for young adult users to interact with and receive streamlined information about sexual health topics and bacterial STI prevention.
The initiative aims to increase accessibility to sexual health information and ensure that the information provide is oriented to the user’s individual needs. This includes sexual health information for members of the LGBTQ+ community. Mojo will equip users with beneficial knowledge and empower them to holistically take charge of their sexual health.
The Mojo initiative seeks to destigmatize sexual health by giving individuals access to free, easy to understand information. This will allow users to feel knowledgeable when talking to health professionals and enable them to start well-educated discussions between peers.
Intervention
Target population/underlying theory/rationale: The target population for Mojo is young adults across all of DC’s eight wards. The digital format of this intervention makes it possible to reach a large audience at an effective cost. The intervention was developed using the cognitive theory of self-efficacy, as it seeks to foster healthy habits among young adult users.
Strategy/mechanism/details: The Mojo app will be promoted on social media platforms (e.g., Instagram, Facebook, Twitter, Snapchat, TikTok) to attract users of the target population to download the app. New users will be prompted to create a profile where they will be able to provide personal information such as their sexual orientation and sexual health topics they are interested in learning more about.
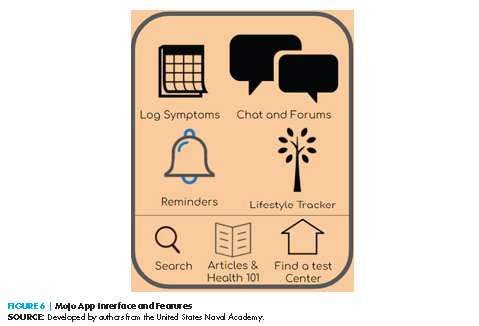
The app’s home screen will then provide multiple icons, each serving a separate function to contribute to the promotion of the user’s sexual health and awareness (as seen in Figure 6):
- Log symptoms: On a daily basis, users can log various symptoms that are commonly associated with bacterial STIs. This can help identify possible infections (Flo Health, n.d.).
- Lifestyle Tracker: Somewhat similar to the daily symptoms log, the lifestyle tracker will allow users to track other facets of their life such as mood, vaginal discharge, and recent sexual activity (Flo Period Tracker, 2019).
- Set testing reminders: This function provides users the opportunity to set reminders for the annually recommended routine STI testing by the CDC (CDC, 2021c).
- Find Test Centers: Based on the user-entered location, this function will provide information on nearby test centers, including appointment requirements and payment options.
- Articles & Health 101: Users can learn about sexual health information by choosing from a vast collection of articles under various topics, including STI Health 101, FAQs, Reproductive Health, Sex, LGBTQ+, and Disorders and Conditions.
- Chat and Forums: At the user’s discretion, users can anonymously chat one-on-one with a health ambassador (a licensed healthcare professional) or can engage within a forum on a topic of their choosing.
- Search: Provides ease of navigation
Potential partners: Key stakeholders are local colleges and universities. Additional stakeholders include the DC Department of Public Health.
Potential barriers and responses: This initiative does not replace a doctor’s diagnosis in identifying STIs, nor does it directly treat STIs. The initiative must make clear to the user that the intent is to simply increase self-awareness of sexual
health and STI prevention.
Uniformed Services University: DSTIGMA
Team members/summary prepared by: Amanda Dao, Tonay Flattum-Riemers, Elizabeth Graydon, Jaime Mencke, Remle Scott, and Patricia Theard
Faculty Advisors: Weyinshet Gossa, Carolyn Reimann, and Christopher Snitcher
Statement of Need and Goal
The incidence of bacterial STIs among 18–24-year-olds in DC continues to steadily increase in low-resource communities, including Wards 7 and 8. To effectively mitigate the incidence of STIs, we must address the stigma surrounding STIs, underutilization of the resources that are available to address the issue, and provide education, with an emphasis on marginalized populations.
The Decreasing Sexually Transmitted Infections through Guidance, Mentoring, and Accessibility (DSTIGMA) intervention was designed to address the underlying causes behind the increased incidence of STIs in DC using a socioecological approach.
Intended Outcomes
DSTIGMA aims to reduce STIs among 18–24-year-olds in Wards 7 and 8 by 10% annually over five years, for a total reduction of 50%.
Intervention
Target population: In the DC area, the highest prevalence of STIs is among 18–24-year-olds living in Wards 7 and 8, consisting of approximately 13,000 individuals. The intervention will focus on the priority populations of African Americans, the LGBTQ+ community, people who engage in sex work, and persons who are incarcerated, pregnant, or experiencing homelessness.
Underlying theory/rationale: Socioeconomic barriers to STI care and health care generally include low income, lack of transportation, food insecurity, gaps in knowledge of health risk behaviors associated with STIs, and inability to obtain health insurance. These socioeconomic barriers can significantly limit STI prevention, screening, and care. DSTIGMA will work with existing organizations in Wards 7 and 8 to increase utilization of available resources, engage the community, and improve the program’s long-term sustainability.
Strategy/Mechanism/Details
Interpersonal and health care bias: Research by the intervention team identified stigmatizing culture and language associated with STIs and developed interventions focused on destigmatizing sexual health risk behaviors and encouraging education and screening of STIs. A study about false beliefs in sexual risk identified that up to 51% of females reported hesitation addressing sex or STIs with their provider (Quest Diagnostics, n.d.). Additionally, 24% of physicians felt uncomfortable discussing STIs with their female patients (Quest Diagnostics, n.d.). As a result, one component of this intervention is a continuing medical education (CME) course to improve provider communication and educate and empower patients on STIs.
Community food distributions: The DSTIGMA intervention engages key community stakeholders at the organizational level. The first step identifies community health care volunteers: culturally trained 18–24-year-olds selected from community social support groups. These volunteers will canvas at existing food distribution networks such as Martha’s Table, Little Lights, So What Else?, and DC Central Kitchen to provide prevention services such as on-site testing and to encourage peer-to-peer conversations about STIs. By leveraging community members and locally embedded organizations, the intervention will create a community initiative to provide hands-on STI testing and education and increase utilization of resources among individuals who have social capital in the target populations.
Recruitment and training of community health care workers: Community volunteers and interns will receive training through the CDC-funded National Network of STD Clinical Prevention Training Centers (PTCs). Johns Hopkins PTC, the regional site, offers low-cost and no-cost training options for different degrees of STI preventative care and education (John Hopkins, n.d.). The training is accessible via virtual and in-person options administered at any location in DC. All staff, including community volunteers, paid interns recruited from Mayor Marion S. Barry’s Summer Youth Employment Program, and full-time community health care workers, will take the Johns Hopkins PTC training at variable levels based on their position. By investing in interns recruited from the community, the initiative will create a network of future community health care workers that will provide longevity to the initiative. DSTIGMA full-time employees will provide mentorship to interns and volunteers, while a full-time infectious disease nurse practitioner will be a clinical intermediary between the community and health care resources.
Policy: DSTIGMA proposes the following policies to improve screening, access to sexual health resources, and patient care. The first policy is to add bacterial STIs to the intake screening of DC Department of Corrections facilities in an effort to identify and reduce transmission in the general population of the corrections facility. Individuals under 35 in detention facilities have higher rates of STIs than nonincarcerated individuals (CDC, 2021b).
A second policy is to provide information and readily accessible resources regarding STIs through dating apps. Among 18–24-year-olds, 27% use dating apps (Smith, 2016), and providing information and readily accessible resources through these applications can encourage awareness and utilization of the free STI resources in the District. However, this policy would require dating applications to provide readily visible information about free local STI resources.
A third policy would integrate screening for bacterial STIs into prevention and care for HIV through the DC Ends HIV initiative. This initiative already has robust plans to end the HIV epidemic by increasing access, testing, education, and care (Bowser, 2020). The proposed policy would require post-test counseling and follow-up care for persons who test positive for an STI, which is essential to prevent further spread and reduce possible complications. This is especially true for pregnant people, because STIs can have serious medical consequences for both the parent and the child.
A final proposed policy would require health care providers in DC to take updated CMEC courses on effective STI communication. As discussed previously, further education on the topic is important for decreasing stigma around sexual health.
Potential barriers and responses: A significant barrier to the program’s implementation is ensuring community buy-in and program longevity. To address this, the intervention will provide peer-to-peer education from culturally trained individuals within the community and leverage community-embedded organizations.
Conclusion
Reflections
Solutions developed by the competing teams were innovative and generally included cross-sector partnerships and community participation or feedback. Most of the proposed strategies paired evidence-based interventions with promising new approaches or new takes on existing approaches. A few solutions leveraged existing resources in exciting ways, which will also help with sustainability of the solutions. However, the judges’ questions and comments underscored that not all teams were clear or realistic in their proposals. For example, mobile app-based interventions can be tricky, as they face significant barriers in achieving discoverability and user engagement. Some of the solutions (or aspects of them) were overly general, and were not tailored to the DC community.
The teams with the most realistic solutions had spoken with DC stakeholders and community members and used what they learned to tailor their interventions, making them more likely to be adopted.
The teams’ presentations and judges’ questions underscore that providing STI resources of any type in isolation will not be enough. As several teams pointed out, DC has many STI interventions and resources in place, yet still has one of the highest STI rates in the country.
Future Plans
The Case Challenge brings the work of the National Academies’ Health and Medicine Division (HMD) and NAM to both university students and the DC community. The NAM and HMD are committed to continuing this activity with the 2022 DC Public Health Case Challenge, which will be hosted by the HMD Roundtable on Population Health Improvement, with the support of the NAM’s Kellogg Health of the Public Fund and involvement from other National Academies groups, including the Global Forum on Innovation in Health Professional Education. HMD and NAM staff continue to look for new ways to further involve and create partnerships with the next generation of leaders in health care and public health and the local DC community through the Case Challenge.
Case Challenge organizers will continue to provide information about the ecological model (IOM, 2003) and upstream factors that affect health in the case document sent to the competing teams. This will help teams prepare for the event and encourage them to utilize these key dimensions in their solutions. Organizers will hold a webinar before the case is released to the competing teams to provide a primer on evidence-based policy solutions for public health issues (in 2021, an overview was provided to the students by Sheri Johnson, PhD, Director, Population Health Institute; Co-Director, County Health Rankings & Roadmaps; Professor, Population Health Sciences, University of Wisconsin–Madison). The webinar orients students to the Case Challenge, reviews best practices developed over the years, and then holds a question and answer period. The webinar is recorded so that students have future access to it.
The organizers are also exploring ways to further engage the student case writing team, which is critical to writing the document that sets the stage for the Case Challenge. Activities could include a writing retreat, webinar, and meetings with District of Columbia leaders working on the topic they are exploring.
The organizers also hope to engage the competing teams and relevant DC stakeholders after the event to further explore solutions to the complex issues presented in the Case Challenge.
Join the conversation!
![]() Tweet this! A new #NAMPerspectives discussion paper provides an overview of the 2021 DC Public Health Case Challenge’s student-submitted solutions to preventing and controlling bacterial sexually transmitted infections in young adults. Read more: https://doi.org/10.31478/202208a #PopHealthRT
Tweet this! A new #NAMPerspectives discussion paper provides an overview of the 2021 DC Public Health Case Challenge’s student-submitted solutions to preventing and controlling bacterial sexually transmitted infections in young adults. Read more: https://doi.org/10.31478/202208a #PopHealthRT
![]() Tweet this! The 2021 DC Public Health Case Challenge, which engages student teams from the DC metro area, is summarized in a new #NAMPerspectives discussion paper. Read more about this program and the winning solution: https://doi.org/10.31478/202208a #PopHealthRT
Tweet this! The 2021 DC Public Health Case Challenge, which engages student teams from the DC metro area, is summarized in a new #NAMPerspectives discussion paper. Read more about this program and the winning solution: https://doi.org/10.31478/202208a #PopHealthRT
Download the graphic below and share it on social media!
References
- Bailey, J., S. Mann, S. Wayal, R. Hunter, C. Free, C. Abraham, and E. Murray. 2015. Sexual health promotion for young people delivered via digital media: A scoping review. Public Health Research 3(13):1-120. https://dx.doi.org/10.3310/phr03130.
- Bowser, M. 2020. DC ends HIV: Ending the HIV epidemic in the District of Columbia for all communities by 2030. Available: https://assets.website-files.com/5f aac3b49b484021bd3f9502/602ef507ad7091a06fa49299_DCH-101%20DC%20Ends%20HIV%20Report_508.pdf (accessed March 24, 2022).
- Bronfenbrenner, U. 1977. Toward an experimental ecology of human development. American Psychologist 32(7):513-531. https://doi.org/10.1037/0003-066X.32.7.513.
- Centers for Disease Control and Prevention (CDC). 2021a. Adolescents and young adults. Available at: https://www.cdc.gov/std/life-stages-populations/adolescents-youngadults.htm (accessed March 24, 2022).
- CDC. 2021b. Persons in correctional facilities. Available at: https://www.cdc.gov/std/treatment-guidelines/correctional.htm (accessed March 24, 2022).
- CDC. 2021c. Screening recommendations and considerations referenced in treatment guidelines and original sources. Available at: https://www.cdc.gov/std/treatment-guidelines/screening-recommendations.htm (accessed March 24, 2022).
- CDC. 2021d. The social-ecological model: A framework for prevention. Available at: https://www.cdc.gov/violenceprevention/about/social-ecologicalmodel.html (accessed March 24, 2022).
- CDC. 2019. Sexually transmitted infections prevalence, incidence, and cost estimates in the United States. Available at: https://www.cdc.gov/std/statistics/prevalence-incidence-cost-2020.htm (accessed March 24, 2022).
- Cunningham, S. D., D. L. Kerrigan, J. M. Jennings, and J. M. Ellen. 2009. Relationships between perceived STD-related stigma, STD-related shame and STD screening among a household sample of adolescents. Perspectives on Sexual and Reproductive Health 41(4):225-230. https://dx.doi.org/10.1363/4122509.
- DC Health Matters. 2021. DC health matters connect. Available at: https://dchealthmattersconnect.auntbertha.com/search_results/20037 (accessed March 24, 2022).
- Flo Health. n.d. Track your health beyond periods. Available at: https://fl o.health/ (accessed March 24, 2022).
- Flo Period Tracker. 2019. Flo. We are together! Available at: https://www.youtube.com/watch?v=rUyIGpwAjhc (accessed March 24, 2022).
- Fortenberry, J. D., M. McFarlane, A. Bleakley, S. Bull, M. Fishbein, D. M. Grimley, C. K. Malotte, and B. P. Stoner. 2002. Relationships of stigma and shame to gonorrhea and HIV screening. American Journal of Public Health 92(3):378-381. https://dx.doi.org/10.2105/ajph.92.3.378.
- Healthy People 2030. 2020. Sexually transmitted infections. Available at: https://health.gov/healthypeople/objectives-and-data/browse-objectives/sexually-transmitted-infections (accessed March 24, 2022).
- Institute of Medicine (IOM). 2003. The Future of the Public’s Health in the 21st Century. Washington, DC: The National Academies Press. https://doi.org/10.17226/10548.
- John Hopkins. n.d. The STD prevention training center at Johns Hopkins. Available at: https://www.stdpreventiontraining.com (accessed March 14, 2022).
- Kahn, R. H., K. E. Moseley, J. N. Thilges, G. Johnson, and T. A. Farley . 2003. Community-based screening and treatment for STDs: Results from a mobile clinic initiative. Sexually Transmitted Diseases 30(8):654-658. https://dx.doi.org/10.2307/44966284.
- Link U. 2021. Link U: Making the connection. Available at: https://linkudmv.org/search_results/20037?widget=linku&ref=dchealth.dc.gov (accessed March 24, 2022).
- McLeroy, K. R., D. Bibeau, A. Steckler, and K. Glanz. 1988. An ecological perspective on health promotion programs. Health Education Quarterly 15(4):351-377. https://doi.org/10.1177/109019818801500401.
- Mission Mobile Medical. 2021. Ready for your next mission with Mission Mobile Medical. Available at: https://www.missionmobilemed.com/ (accessed February 2, 2022).
- National Academies of Sciences, Engineering, and Medicine (NASEM). 2021. Sexually transmitted infections: Adopting a sexual health paradigm. Edited by S. H. Vermund, A. B. Geller and J. S. Crowley. Washington, DC: The National Academies Press. https://doi.org/10.17226/25955.
- Quest Diagnostics. n.d. Young women and STDs: Are physicians doing enough to empower their patients and protect their health? Available at: https://mma.prnewswire.com/media/662641/Young_Women_and_STDs_Physicians_Report.pdf?p=original (accessed March 24, 2022).
- Smith, A. 2016. 15% of American adults have used online dating sites or mobile dating apps. Washington, DC: Pew Research Center. Available at: https://www.pewresearch.org/internet/2016/02/11/15-percent-of-american-adults-have-used-online-dating-sites-or-mobile-dating-apps/ (accessed March 24, 2022).
- Wong, T., J. R. Pharr, T. Bungum, C. Coughenour, and N. L. Lough. 2019. Effects of peer sexual health education on college campuses: A systematic review. Health Promotion Practice 20(5):652-666. https://dx.doi.org/10.1177/1524839918794632.