Educating Health Professions Educators to Address the “isms"

Samuel Little and Victoria Stubbs talked about “creating a brave space” for having difficult conversations [1]. Opening such conversations, which can expose painful pasts and personal vulnerabilities, is difficult but can be a first step in the healing process that will help people grow together as human beings and as health professionals. Stubbs described the classroom as a potential brave space. It is safe, she said, if the challenges faced by students and faculty are acknowledged while attempting to engage in difficult and/or sensitive discussions around topics such as “race, power, privilege, and the various forms of oppression for the purpose of learning” [2]. While these difficult conversations can start in the classroom, they may be rendered almost useless if the actions in the clinical environment do not align with those set up in the classroom. The danger in not addressing such underlying frictions in the classroom and in the workplace is the risk of creating intractable barriers between and among people that, over time, become increasingly difficult to undo. This paper is an attempt to guide health professional educators across the learning continuum, in how to create a safe space to discuss racism and other isms (see Box 1).
Discussing the isms in All Their Forms
Educating health professions instructors on how to create a safe environment for students and colleagues to talk authentically about the isms requires transparency that is not common to some, particularly those accustomed to more didactic instructional approaches. It may not be a comfortable topic even for instructors who espouse more interactional styles of teaching. While discussing isms might not be comfortable, it is important for educators in the various health professions to prepare students to work effectively with diverse populations. Mental health and social service professions (e.g., counseling, psychology, and social work) can provide direction to educators on approaches to engage in a genuine dialogue on delicate issues like racism, sexism, ageism, and xenophobia.
The first step for the educator is to conduct a self-assessment of privilege, bias, prejudice, and stereotypes. This assessment would ideally include input from others because of the inherent biases and difficulties associated with accurately assessing oneself. Knowing preconceived notions can impact a person’s actions, can help a person deal with these underlying beliefs if and when they are brought to the person’s attention. It is critically important to uncover one’s unconscious beliefs before opening a discussion on racism, or any of the isms.
In the second step, attention to system-level and historical structural inequities will provide context for creating a safe—but not necessarily a comfortable—space to have difficult conversations and facilitate transformative learning experiences [6,7,8]. Further steps are to invite a dialogue with diverse learners and to be prepared to listen. During these conversations, educators must work to suspend their personal biases and meet people where they are. They also need to self-reflect on their potential for microaggressions toward some students. For example, Ackerman-Barger et al. found racial microaggressions—unconscious communication of subtle, condescending messages directed toward people of color—were experienced by underrepresented health professions students, negatively affecting their learning, academic performance, and well-being [9]. It therefore stands to reason that educators’ self-examination of implicit biases can improve learners’ educational experience [6] by setting the right tone for a culturally rich learning environment.
Creating a Safe Space from Education to Practice
By being in the moment and listening without making assumptions, the educator creates a safe space to more openly discuss how ethnicity and gender identity as well as lived experiences, social networks, and structural forms of discrimination have supported or diminished a learner’s overall wellness [9]. Educators must also take steps toward creating a safe space for difficult conversations. This means role modeling openness and a willingness to listen. It also means creating an awareness of how one’s actions can impact others, and understanding that engaging in difficult conversations is only possible if everyone in the room feels safe to speak up and express themselves. Inviting a productive conversation about isms and using open, neutral questions can lead to powerful experiences for students. These conversations can have a lasting impact on students when they enter the world of practice. Educators must be careful not to alienate people who speak up in order to make this experience productive. Individuals who do speak up risk exposing their own personal vulnerabilities and may fear a mix of repercussions from awkward silence to hostile exchanges. Educators can manage expressed vulnerabilities by acknowledging this concern and demonstrating empathy.
Listening and empathy are critical skills for all health professionals. Clinical educators who model these skills during difficult conversations meaningfully impact the future practice of their students. Another way to teach listening and empathy skills is to provide students with the opportunity to practice these skills during role plays with peers or simulated patients who represent an intersection of diverse backgrounds. It is important for health professionals to be able to apply these skills under pressure. Adding a time constraint to the role play creates a stressful training environment that can closely resemble the realities faced by clinicians working in a busy clinic. In this type of role play, the educator should evaluate students’ ability to support a diverse patient and to provide a warm handoff to colleagues with the requisite expertise in managing the patient’s needs. Successful handoff s are largely a result of an established practice of caring for patients and experiencing effective interprofessional teams during clinical training.
Ultimately, the message for learners is to connect and build relationships from a position of cultural humility. Hook et al. defined cultural humility as “having an interpersonal stance that is other-oriented rather than self-focused, characterized by respect and lack of superiority toward an individual’s cultural background and experience” [10]. Cultural humility must be part of every patient interaction, and it must be applied to coworkers to reinforce the practice. In an interprofessional setting, clinical educators must model the desired behaviors and purposefully create a safe space for sharing personal experiences.
Tools for Educating Students About the isms
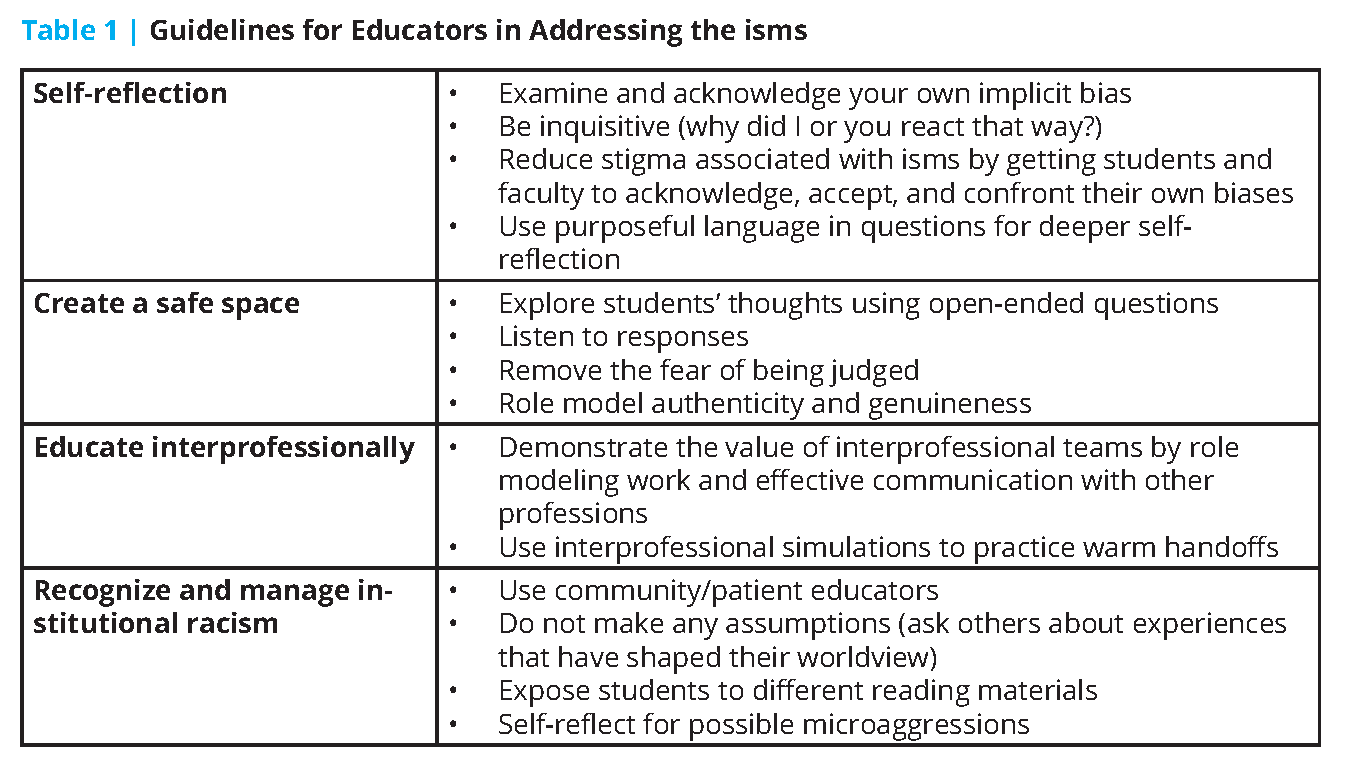
Interactive class exercises provide a forum for beginning to address deeply held beliefs about stereotypes. A suggested activity from the authors is to ask each person in the class to write words on a flip chart that describe who they are. Afterward, the class can engage in facilitated discussion that celebrates each person’s background and heritage. The purpose of this activity is to highlight the intersectionality of race, gender, culture, socioeconomic status, and other demographic variables in the development of self-identity. The key to success in this exercise is for the educator to use the self-descriptions in an instructive manner and to create an environment where everyone feels safe in sharing their “authentic self” (see Table 1).
While these exercises can be conducted online, the facilitator will need to have a heightened sensitivity with regard to the students’ comfort levels in expressing their feelings through synchronous or asynchronous virtual platforms. Online educators should incorporate appropriate “check-ins” to monitor students’ emotional states. This is especially important during times of crisis. The class check-ins can be live, interactive conversations for welcoming students, introducing assignments, or reviewing new material. They can be written directly into the course syllabus along with a statement focusing on the importance of culture in the delivery of the course material. This statement goes beyond the goals and objectives of a course by providing the tone for how the course will be run as opposed to what the material will cover.
Another exercise that can lead to a productive discussion about diversity, stigma, and bias is for educators to compile a list of resources (e.g., reading, YouTube, and/or podcast lists) that extend beyond traditional peer-reviewed journals. After reviewing the materials, a purposeful class discussion can ensue about the diversity of the authors or presenters, and about the potential for institutionalized racism or bias in the publication process. This simple action can be useful in highlighting inequities. Students can then be asked to conduct personal reflections of carefully selected resources to explore their own biases and how such biases may be influencing their perceptions of reality and their surroundings. Through this type of exercise, students can become better prepared to understand the diversity of experiences that their patients will bring to the treatment room.
The Institutional Stance on isms
Colleges and universities that train health professionals can also take a cultural stance in addressing isms. By adopting values that combat racism and by recognizing the importance of individuals understanding their own biases, an educational institution can become a role model for similar organizations. For example, there have been cases in which health professionals from diverse backgrounds have been requested to participate in activities to represent the voice of diversity—a form of performative allyship called tokenism. To reduce institutional tokenism, a school’s leadership can acknowledge that every individual is unique and that diverse individuals represent their own intersectionality of race, gender, culture, and socioeconomic status rather than the perspective of their racial or cultural background. By taking a conscious step to acknowledge and mitigate isms through sound policy, an institution creates a culture where difficult conversations are appreciated and where diversity is supported.
Lifelong Interprofessional Learning
Addressing isms and changing culture involves a lifelong commitment to learning; it is not a one-time event. The more health professional learners and educators listen to people from diverse cultures, professions, backgrounds, and ethnicities, the deeper their understanding becomes about others’ challenges and assets. Mandated continuing education (CE) that reinforces these principles may be what is needed to understand and appreciate the perspective of patients and peers from various cultures. There is precedent for mandated interprofessional CE. Governors across the country have begun requiring suicide prevention training for diverse groups of mental health professionals [11]. The mandates led to interprofessional CE opportunities within mental health that extended beyond those who were required by law to get the CE credit. Though mandated interprofessional education is a valuable step toward culture change, there are mixed results on the effectiveness of CE. Therefore, many professional groups are moving away from blanket CE to models based on continuing competence and targets based on need and context. In this regard, interprofessional competence might give rise to intercultural education. Discussing the isms through this more transformative approach has the potential to open conversations among health professionals and educators about the critical importance of addressing racism, xenophobia, gender discrimination, and all the isms across the learning continuum.
Conclusion
Health professions educators must first learn and acknowledge their own biases before they can create a safe space for others to learn. Educational institutions with sound policies emphasizing cultural humility help educators work together to break down social, professional, and cultural barriers that impede productive communication. Interprofessional, intercultural role modeling can begin in the classroom, but it cannot end there. Lifelong learning is needed to grow continuously through listening and self-reflection. Educating the educators on how to create a brave space to bring these skills to their students will be one major step toward addressing and dismantling the isms.
Join the conversation!
![]() Tweet this! Educating health professionals on how to address the “isms” in their daily work is critical in working to reduce existing health disparities and ensure historically marginalized populations receive appropriate care: https://doi.org/10.31478/202008e #NAMPerspectives
Tweet this! Educating health professionals on how to address the “isms” in their daily work is critical in working to reduce existing health disparities and ensure historically marginalized populations receive appropriate care: https://doi.org/10.31478/202008e #NAMPerspectives
![]() Tweet this! The classroom can be a “brave space” to openly discuss how to address racism, sexism, homophobia and other “isms” – and as such, health profession educators have a critical role to play in creating this space for students: https://doi.org/10.31478/202008e #NAMPerspectives
Tweet this! The classroom can be a “brave space” to openly discuss how to address racism, sexism, homophobia and other “isms” – and as such, health profession educators have a critical role to play in creating this space for students: https://doi.org/10.31478/202008e #NAMPerspectives
![]() Tweet this! Listening & empathy are critical skills for health professionals, and educators can help learners develop these skills through courageous conversations about the “isms” in all their forms. A new #NAMPerspectives provides some potential approaches: https://doi.org/10.31478/202008e
Tweet this! Listening & empathy are critical skills for health professionals, and educators can help learners develop these skills through courageous conversations about the “isms” in all their forms. A new #NAMPerspectives provides some potential approaches: https://doi.org/10.31478/202008e
Download the graphics below and share them on social media!
References
- Little, S., and V. D. Stubbs. 2018. Creating a brave space for difficult dialogues and critical thinking. In Race and the intersection of abuse, power and control: Research & reflections from the black perspective, edited by R. Cosby and R. Grant. Washington, DC: Howard University School of Social Work.
- UMB Diversity Advisory Council. 2019. DAC spotlight: Victoria D. Stubbs, MSW. The Elm. Available at: https://elm.umaryland.edu/elm-stories/Elm-Stories-Content/DAC-Spotlight-Victoria-D-Stubbs-MSW.php (accessed June 29, 2020).
- Richman, L. S., and M. R. Leary. 2009. Reactions to discrimination, stigmatization, ostracism, and other forms of interpersonal rejection. Psychological Review 116(2):365–383. https://doi.org/10.1037/a0015250.
- Lee, D. B., M. K. Peckins, A. L. Miller, M. O. Hope, E.W. Neblett, S. Assari, J. Munoz-Velazquez, and M. A. Zimmerman. 2018. Pathways from racial discrimination to cortisol/DHEA imbalance: Protective role of religious involvement. Ethnicity & Health 1–18. https://doi.org/10.1080/13557858.2018.1520815.
- Berger, M. and Z. Sarnyai. 2015. “More than skin deep”: Stress neurobiology and mental health consequences of racial discrimination. Stress 18(1):1–10. https://doi.org/10.3109/10253890.2014.989204.
- Sukhera J., C. J. Watling, and C. M. Gonzalez. 2020. Implicit bias in health professions: From recognition to transformation. Academic Medicine 95(5):717–723. https://doi.org/10.1097/ACM.0000000000003173.
- Sherman, M. D., J. Ricco, S. C. Nelson, S. J. Nezhad, and S. Prasad. 2019. Implicit bias training in a residency program: Aiming for enduring effects. Family Medicine 51(8):677–681. https://doi.org/10.22454/FamMed.2019.947255.
- Sukhera, J, A. Milne, P. W. Teunissen, L. Lingard, and C. Watling. 2018. The actual versus idealized self: Exploring responses to feedback about implicit bias in health professionals. Academic Medicine 93(4):623–629 https://doi.org/10.1097/ACM.0000000000002006.
- Ackerman-Barger, K., D. Boatright, R. Gonzalez-Colaso, R. Orozco, and D. Latimore. 2020. Seeking inclusion excellence: Understanding racial microaggressions as experienced by underrepresented medical and nursing students. Academic Medicine 95(5):758–763. https://doi.org/10.1097/ACM.0000000000003077.
- Hook, J. N., D. E. Davis, J. Owen, E. L. Worthington Jr., and S. O. Utsey. 2013. Cultural humility: Measuring openness to culturally diverse clients. Journal of Counseling Psychology 60(3):353–366. https://doi.org/10.1037/a0032595.
- American Foundation for Suicide Prevention (AFSP). 2020. State laws on suicide prevention training for health professionals. Available at: https://www.datocms-assets.com/12810/1592504844-health-professional-training-issue-brief-6-18-20.pdf (accessed June 29, 2020).