Clinician Well-Being at Virginia Mason Kirkland Medical Center: A Case Study

Background
Clinician burnout has become a pervasive issue [1] for U.S. clinicians, students, and trainees. Burnout, a syndrome characterized by a high degree of emotional exhaustion and depersonalization, and a low sense of personal accomplishment from work, is cause for concern in the health care field because it can affect quality, safety, and health care system performance. Clinician burnout is largely a result of external factors outside of the control of an individual clinician. This includes regulations, incentives, policies, culture, stigma and more.
The following case study provides an overview of initiatives that support well-being and reduce burnout in clinicians who work at the Virginia Mason Kirkland Medical Center (Kirkland Medical Center). The purpose of this case study is to provide readers with tangible information to understand how Kirkland Medical Center has adopted programs and policies that support wellbeing. This case study is not a prescriptive roadmap. Rather, the authors hope that this case study will serve as an idea-generating resource for leaders working to improve the well-being of our nation’s clinicians, trainees, and students. The development of this case study was informed by extensive interviews with Kirkland Medical Center health professionals and their leadership team.
Introduction
Kirkland Medical Center is an outpatient clinic that employs more than 30 full-time clinicians and more than 70 non-clinician staff. Kirkland Medical Center is part of the Virginia Mason Health System (Virginia Mason) in Washington State and was one of the first clinics built after Virginia Mason adopted the Virginia Mason Production System1 (VMPS) – an innovative, systemwide management method used to improve patient care and safety. Modeled after the Toyota Production System2, VMPS eliminates waste and inefficiency by streamlining repetitive aspects of care delivery, standardizing clinical roles, and consistently engaging in continuous learning activities. While researchers have shown the value of VMPS in improving care quality [2] and lowering costs [3], little has been written about its role in improving clinician well-being and preventing burnout.
This case study aims to highlight key features of Kirkland Medical Center (and its adoption of VMPS) that have led to improved rates of employee satisfaction, engagement, and overall well-being. At Kirkland Medical Center, two pillars play a central role in improving clinician well-being: (1) workflow optimization and (2) a culture of collegiality, respect, and innovation.
Workflow Optimization
Kirkland Medical Center prioritizes workflow optimization and embeds continuous learning and quality improvement into everyday practice at the clinic. The culture at Kirkland Medical Center is one in which all clinicians and staff are encouraged and expected to employ strategies that improve clinic outcomes via the Plan-Do-Study-Act process3. Executive leadership notes that by optimizing workflows and investing in continuous learning and quality improvement, Kirkland Medical Center creates a sustainable system that does not depend on a single leader to maintain efficient operations. The following are key elements of Kirkland Medical Center’s workflow optimization strategy – all of which can lead to improved patient care and clinician well-being:
- The physical design of the clinic,
- Clinicians practicing to the full extent of their education and training,
- Standardized roles for medical assistants (MAs),
- Purposeful cross-training to minimize disruptions due to absences, and
- Protected time for breaks and documentation throughout the day.
Physical Design of the Clinic
Kirkland Medical Center is designed as two concentric rings with no waiting rooms. Patients are assigned to an exam room immediately upon arrival for their appointment. The inner loop hosts the exam rooms, and the outer loop contains clinician workstations. All exam rooms have a front entrance, through which patients enter, and a back entrance, through which clinicians can enter directly from their work stations.
Kirkland Medical Center arranges advanced registered nurse providers (ARNPs), physician assistants (PAs), pharmacists, and physicians into pods, or clinical teams. Medical assistants (MAs) are on rotation and shared across the pods in which they work. Advanced practice providers have small, independent patient panels but in large part share and have co-ownership of patient panels within their pods. Clinician workstations are positioned side-by-side, enabling pods to easily prepare for, communicate during, and debrief after patient visits. Medical supplies are located in organized drawers on the back of each room, enabling MAs to easily reconcile and restock supplies as part of their workflow.
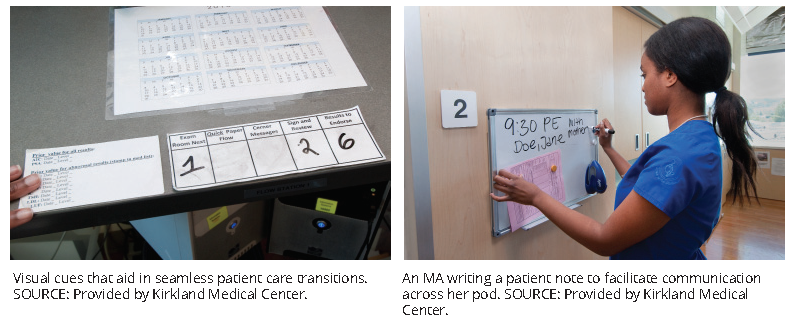
A system of visual cues facilitates streamlined care, coordination, and communication. The back entrance of each exam room is equipped with a whiteboard upon which MAs can notify clinicians of patient concerns prior to their interaction with the patient. Door tags alert primary care providers when MAs have completed their initial evaluation and patients are ready to be seen. Warm handoff s from one clinician to another are still completed when necessary.
Drivers of clinician burnout often include inefficient team structures and lack of collaboration between team members [4]. Kirkland Medical Center clinicians express that the physical design and visual cues aid them in performing seamless transitions between patients and provide a space to collaborate and inform one another of issues that may arise. Clinicians also felt that these aspects reduce their burnout and improve their well-being because they feel more confident in patient transitions throughout the day and are comforted by direct channels of communication, through which it is unlikely that major issues will be missed.
Practicing to the Full Extent of One’s Education and Training
At Kirkland Medical Center, all clinicians practice to the full extent of their education and training. Efficiency is ensured by eliminating the time clinicians spend on tasks that do not require their current level of licensure and certification, a major contributor to clinician dissatisfaction [1]. On a practical level, such efficiency allows for better reimbursement for clinicians and the clinic, but it also improves patient care and clinician joy. Physicians, ARNPs, and PAs note that working to the full extent of their education and training frees up time to contemplate complex patient care issues, which can improve their clinical care skills and enhance patient outcomes. Clinicians interviewed also emphasize a high sense of professional fulfillment, because they can better use their specialized skills and support other team members, ultimately improving patient care.
Clinical pharmacists are an integral part of the care delivery model at Kirkland Medical Center, where they collaborate with primary care providers in the overall care of the patient. They work to the full extent of their education and training and often consult with patients independently, especially those with chronic conditions. Kirkland Medical Center trains pharmacists to address all patient questions regarding medication, including tolerance, adherence, and affordability. They are also trained to provide guidance on lifestyle behaviors that could improve a patient’s overall health. Clinical pharmacists have the authority to discuss and implement changes in pharmacological therapy with patients and make recommendations per standard of care protocols. Kirkland Medical Center pharmacists can also provide direct recommendations to patients on altering medications. Pharmacists communicate these recommendations to the responsible physician through a clinical note in the patient portal.
Intentionally incorporating clinical pharmacists into the care team is a good business model for Kirkland Medical Center because it frees up time for physicians, ARNPs, and PAs to see (and bill for) more acute and complex patients and it contributes to increased fulfillment for pharmacists who are more intimately involved in direct patient care. Private payers do not consistently reimburse pharmacists for their direct patient care services. However, when pharmacists consult patients independently, physicians, ARNPs, and PAs have additional time to consult other more complex patients, who are typically reimbursed at a higher rate. Executive leadership notes that the return on investment typically outweighs the salaried costs of their pharmacists. The integration of clinical pharmacists into the care team also provides substantial benefits to patients by offering them direct access to pharmacists
who are well versed in managing chronic diseases and medications.
Standardized Roles for Medical Assistants
MAs are key players in ensuring that Kirkland Medical Center clinicians are able to practice to the full extent of their education and training. There is a 1:1 MA-to physician/advanced practitioner ratio at Kirkland Medical Center. Leadership leverages their organizational model and MA-practitioner ratio as a recruitment strategy while MAs are still participating in training and externships. Leadership has found great success in retaining MAs, having an 8 percent turnover rate compared to the 25 percent national average.
MAs are a large contributor to strengthened team and patient relationships. They help reduce clinician workload and increase clinician productivity by managing administrative tasks, thereby freeing up time for physicians, ARNPs, and PAs to spend with patients.
MAs play a substantial role in:
- Identifying care gaps,
- Performing scribing duties,
- Confirming patient medications and prescriptions,
- Processing medication and testing orders,
- Requesting medical records,
- Replying to patient portal messages, and
- Completing paperwork.
All MAs complete standardized training to reduce variability and ensure consistency in workflow and tasks. This standardization ensures that physicians, ARNPs, and PAs can expect the same level of support regardless of which MA is working on their team on a given day. Kirkland Medical Center physicians, ARNPs, and PAs note that this standardization has led to a high level of trust in all MAs.
Cross-Training for Absences
Kirkland Medical Center cross-trains all MAs and administrative staff in at least one other role. Crosstraining and the standardization of roles efficiently distributes workload, prepares everyone to deal with absences in a standardized manner, ensures continuity of practice, and enhances clinician work-life integration by reducing worry about team functionality and patient care while on leave.
Protected Time
Mandatory “Pauses”
An internal Kirkland Medical Center study found that clinicians completed patient visits in 20 minutes, on average. Using this knowledge, Kirkland Medical Center adjusted its patient chart accordingly, scheduling all patient visits in 20-minute intervals and incorporating a mandatory 20-minute “pause” for its clinicians after every three to five patient visits. Scheduling staff cannot override these pauses. Kirkland Medical Center incorporated pauses to protect clinicians’ time and allow them to take mental and physical breaks from patient care and perform indirect care tasks, such as addressing patient portal messages or covering for other colleagues. These 20-minute pauses also allow clinicians to address documentation needs throughout the day, which ensures they can leave for home within one hour of seeing their last patient. Clinicians note that they typically are home every night in time to enjoy quality time with their families and partake in wellness activities, and rarely need to bring work home with them.
Joy at Work Team
Some clinicians use their protected time to participate in the Joy at Work team. The Joy at Work team is dedicated to the emotional well-being of all staff and helps arrange outings such as bowling, visits to sporting events, monthly potlucks, and more. Executive leadership notes that the Joy at Work team helps reduce burnout and creates a culture in which all staff members feel respected and regarded as equals.
Professional Development
Clinicians’ protected time also allows them to partake in professional development activities and organizational improvement processes. All clinicians and administrative staff can participate in one of two “innovation teams”:
- Direct Care Innovation Team: Addresses system inefficiencies related to direct patient care, such as communication and follow-up.
- Indirect Care Innovation Team: Addresses system inefficiencies related to indirect patient care, such as documentation and scheduling.
Although this is not a requirement, most clinicians willingly participate in at least one innovation team. Each team is composed of 12-15 members, consists of different types of health care professionals, and includes administrative staff.
These teams meet on a monthly basis. Teams do their best to schedule meetings during times when most team members can join. Nonclinical staff and nonsalaried staff are compensated for time spent with their innovation teams. By design, 15 percent of clinician compensation is non-production-based and covers time spent on quality improvement initiatives or professional development opportunities, such as the Joy at Work team, innovation teams, publishing, speaking, teaching, and other committee work. Clinicians share that having protected time each day contributes to their work-life integration and overall joy because they are able to partake in (and be compensated for) development opportunities and get home on time.
Ultimately, the factors listed above all contribute to enhanced workflow optimization and increase clinicians’ professional fulfillment, because clinicians are able to take on more responsibility and be more intimately involved in direct patient care. These system-level strategies also optimize team-based care and contribute to trust-building within the Kirkland Medical Center’s care teams. Reduced clinician workload and administrative burden [5], increased professional fulfillment [6], and optimized team-based care [4] can reduce clinician burnout.
Culture of Collegiality, Respect, and Innovation
Kirkland Medical Center prioritizes a culture of collegiality, respect, and innovation. Executive leadership and human resources introduce a culture of collegiality and respect during the hiring process and maintain it through transparent leadership and an enforced code of conduct. Executive leadership engenders a culture of innovation by supporting quality improvement activities at all levels, breaking down hierarchical structures, and leveling power differentials. Kirkland Medical Center grounds its culture of innovation by respecting individual ideas and voices and understanding that the people who know the system best are those who work within it. Leadership encourages all clinicians and staff members to speak up when they encounter administrative or direct care inefficiencies by mobilizing a standardized Plan-Do-Study-Act process3 that addresses these problems using a team-based approach.
Maintaining a Culture of Collegiality and Respect
Beginning with the interview process and throughout onboarding and everyday practice, executive leadership sets expectations and reaffirms a culture of collegiality and respect for all employees. Participating in the Respect for People5 initiative, compulsory for all staff, instills in them Virginia Mason Health System’s 10 transactional behavior principles. These 10 behavior principles are used to help select candidates during the interviewing process and are promulgated during the onboarding process and beyond. Kirkland Medical Center also applies these principles during its first-year nurse program, new-leader mentorship program, medical assistant apprenticeship program, and nurse residency program. The Respect for People initiative is foundational to many process improvement efforts, and has become a key part of organizational vernacular.
One example of the Respect for People initiative in action is that, due to instances of patients displaying disrespectful behavior, the initiative now conducts all-staff trainings to standardize “speaking up” phrases such as “My role here is to take the very best care of you … and I will not tolerate offensive behavior. Now let’s refocus on how I can help you today.”
Additionally, Kirkland Medical Center maintains a culture of collegiality and respect through the following:
- One-hour “huddle discussions” conducted by mid-level leaders about various aspects of respect, such as growth, patient experience, and diversity and inclusion;
- Required online courses focused on lesbian, gay, bisexual, transgender, queer, and questioning identities to support the delivery of accessible, affirming, and patient-centered health care;
- Periodic team discussions using guides developed by Kirkland Medical Center leadership, such as “Being Inclusive and Honoring Diversity”, “Strengths and Commitments for Improvement in Being Respectful,” and “Speaking Up and Connecting with Others”; and
- A quarterly, eight-hour, off-site “Connections” workshop designed by the Virginia Mason Health System. The workshop is offered to all clinicians and builds their relationship-centered and empathic communication skills.
If individual employees do not adhere to the cultural standards of respect and collegiality, members of the executive leadership team coach them through a behavior change process. Executive leadership meets with them to discuss negative behavior and to reaffirm expectations. Leadership may also schedule monthly meetings, provide reading materials, and share tactics for behavior improvement. If employees continue to work outside of the cultural boundaries, executive leadership is prepared to let them go, understanding that maintaining a culture of collegiality and respect may necessitate removing individuals who disrupt a desired culture.
Maintaining a Culture of Innovation
Kirkland Medical Center has implemented a systemwide Plan-Do-Study-Act3 (PDSA) process to solve issues and inefficiencies. PDSA is a core organizational strategy and is completed using a team-based approach to improve overall system efficiency through incremental changes. Leadership encourages all employees, including clinicians and administrative staff, to propose such actions (PDSAs) by completing an electronic form when they encounter an issue. The PDSA process includes the following steps:
- Clinicians or staff submit a PDSA form to leadership. The leadership team sorts submissions and determines whether a submission is ripe for the test implementation phase, in which a solution is tested, refined, and reported.
- Depending on the topic of the submission, either the Direct Care or the Indirect Care Innovation Team identifies and tests a pilot solution.
- A clinical pod enacts this pilot solution for several weeks to work through its viability before it is implemented clinic-wide. A pod is a particular clinical team, composed of an ARNP, a PA, a pharmacist, a physician, and a rotating MA. The pod reports back to the innovation team on the usefulness of the solution and its feasibility. This process is iterated until potential complications are mitigated, modifications are made, and issues are resolved. The average time to implement changes varies substantially depending on the topic.
- Once deemed effective, the lead MAs implement the solution clinic-wide.
For example, a team submitted a PDSA to improve message routing processes, suggesting that certain messages should be sent to team inboxes rather than individual clinician inboxes. The purpose of this message routing change was to facilitate team-based care and reduce the inefficient practice of reviewing several inboxes to address all messages. The solution was refined for about three months and was implemented clinic-wide once all issues were resolved.
On average, four PDSAs are implemented each week, amounting to approximately 200 PDSAs per year. Leadership understands the need to strike a balance between implementing too many PDSAs and contributing to burnout, versus not implementing enough PDSAs to be effective. Leadership constantly assesses the pulse of teams and reduces the amount of PDSAs conducted when necessary.
The PDSA process underscores Kirkland Medical Center’s commitment to problem solving and cultivates a culture in which employees trust that if they encounter a problem, their input will be valued, executive leadership will take it seriously, and a dedicated team of employees will address it. PDSAs ultimately improve workflow inefficiencies, which can reduce burnout and improve well-being [7].
Measuring Staff Engagement, Satisfaction, and Turnover
Leadership annually surveys staff and clinicians using an advisory board survey to measure clinician wellbeing, engagement, satisfaction, and turnover. Leadership also uses the Agency for Healthcare Research and Quality’s Surveys on Patient Safety Culture6 to measure communication and teamwork.
Kirkland Medical Center’s most recent survey data shows that 90 percent of Kirkland Medical Center’s non-clinician staff is “content” or “engaged”, and 93 percent of clinicians are “content” or “engaged” (Internal survey data, September 2018). Executive leadership mandates that all operational leaders review their team’s disaggregated data and work continuously to improve clinician outcomes. Operational leaders also meet monthly with clinicians to discuss practice issues, career goals, and other professional growth opportunities.
For example, in response to recent survey data, local supervisors worked with their teams to develop shared goals. Some teams indicated they “would like more VMPS education and training.” Therefore, leadership organized a central improvement office specialist to teach deeper process improvement concepts to teams on a monthly basis.
Challenges
Kirkland Medical Center employees note two main challenges:
- Not everyone will naturally thrive in Kirkland Medical Center’s work environment because some may perceive a loss of autonomy or control.
- The PDSA process may not always prioritize clinician well-being.
Natural Fit
Kirkland Medical Center’s employees admit that certain clinicians might hesitate to accept Kirkland Medical Center’s workflow optimization strategy, fearing that it will reduce autonomy and control. The fast-paced and constant urgency for systems improvement may be overwhelming for some clinicians, and other organizations should consider this if implementing a similar system. However, Kirkland Medical Center staff believe that because of this system, the clinician experience is more efficient and mental energy can be primarily devoted to direct patient care, rather than workflow and workload issues.
Emphasis on Process Improvement
Although Kirkland Medical Center employees credit the PDSA process with improving quality by preventing errors, eliminating waste, and increasing system efficiency, this process may also have unintended consequences if implemented too frequently. The PDSA process may introduce added barriers to patient care, because, at times, it can take clinicians out of their normal workflow. Kirkland Medical Center employees note that it is important for leadership not to over-value urgency and constant innovation in a way that exacerbates clinician burnout.
Conclusion
Through the adoption of VMPS, the Virginia Mason Kirkland Medical Center has built a system-wide quality improvement methodology7 in which standardized processes reduce variation and improve outcomes for patients and the health care team. Kirkland Medical Center employees believe that the seamless integration of the VMPS management method into Kirkland Medical Center has directly improved their well-being and has reduced certain drivers of burnout.
Kirkland Medical Center’s workflow optimization strategies have transformed the physical space to facilitate team-based care, enhance communication, and reduce inefficiencies. By practicing to the full extent of their education and training, clinicians have distributed workload across team members and deepened their sense of professional fulfillment. The standardized role of MAs has reduced administrative burden and increased workflow efficiency. Cross-training team members has lowered stress during absences, and clinicians’ mandatory protected time has improved work-life integration and enhanced overall joy.
Kirkland Medical Center has fostered a culture of collegiality, respect, and innovation present in everyday practice at the clinic. It has engendered a sense of community, an appreciation of everyone’s value, and a commitment to problem-solving that has enriched clinician well-being and engagement.
Join the conversation!
![]() Tweet this! #Burnout is widespread among clinicians. Solutions ARE possible. New case studies, published in #NAMPerspectives, offer actionable insights from @OhioState and @VirginiaMason. Let’s build a better system to help clinicians thrive: nam.edu/Perspectives #ClinicianWellBeing
Tweet this! #Burnout is widespread among clinicians. Solutions ARE possible. New case studies, published in #NAMPerspectives, offer actionable insights from @OhioState and @VirginiaMason. Let’s build a better system to help clinicians thrive: nam.edu/Perspectives #ClinicianWellBeing
![]() Tweet this! How can health care organizations begin to address the factors that affect clinician #burnout? New case studies from @theNAMedicine, now published in #NAMPerspectives, provide actionable solutions. Read more: nam.edu/Perspectives #ClinicianWellBeing
Tweet this! How can health care organizations begin to address the factors that affect clinician #burnout? New case studies from @theNAMedicine, now published in #NAMPerspectives, provide actionable solutions. Read more: nam.edu/Perspectives #ClinicianWellBeing
![]() Tweet this! .@VirginiaMason Kirkland Medical Center’s #ClinicanWellBeing Case Study, now published in #NAMPerspectives, offers insights into workflow optimization, a culture of respect, quality improvement, continuous learning, and standardized processes: nam.edu/Perspectives
Tweet this! .@VirginiaMason Kirkland Medical Center’s #ClinicanWellBeing Case Study, now published in #NAMPerspectives, offers insights into workflow optimization, a culture of respect, quality improvement, continuous learning, and standardized processes: nam.edu/Perspectives
Download the graphics below and share them on social media!

Notes
Identified as superscript numbers throughout the text
- https://www.virginiamason.org/vmps
- https://global.toyota/en/company/vision-and-philosophy/production-system/
- http://www.ihi.org/resources/Pages/Tools/PlanDoStudyActWorksheet.aspx
- https://www.wsparx.org/page/ProviderStatus
- https://www.virginiamasoninstitute.org/2013/01/respect-for-people-building-block-for-engagedstaff-satisfied-patients/
- https://www.ahrq.gov/sops/surveys/index.html
- https://www.ahrq.gov/professionals/preventionchronic-care/improve/system/pfhandbook/mod4.html
References
- Dyrbye, L. N., T. D. Shanafelt, C. A. Sinsky, P. F. Cipriano, J. Bhatt, A. Ommaya, C. P. West, and D. Meyers. 2017. Burnout Among Health Care Professionals: A Call to Explore and Address this Underrecognized Threat to Safe, High-Quality Care. NAM Perspectives. Discussion Paper, National Academy of Medicine, Washington, DC. https://doi.org/10.31478/201707b
- Blackmore, C. C., R. S. Mecklenburg, and G. S. Kaplan. 2011. At Virginia Mason, Collaboration Among Providers, Employers, and Health Plans to Transform Care Cut Costs and Improved Quality. Health Affairs 30(9). https://doi.org/10.1377/hlthaff .2011.0291
- Blackmore, C. C., J. W. Edwards, C. Searles, D. Wechter, R. Mecklenburg, and G. S. Kaplan. 2013. Nurse Practitioner-Staff ed Clinic at Virginia Mason Improves Care and Lowers Costs for Women with Benign Breast Conditions. Health Affairs 32(1). https://doi.org/10.1377/hlthaff .2012.0006
- Smith, C. D., C. Balatbat, S. Corbridge, A. L. Dopp, J. Fried, R. Harter, S. Landefeld, C. Martin, F. Opelka, L. Sandy, L. Sato, and C. Sinsky. 2018. Implementing optimal team-based care to reduce clinician burnout. NAM Perspectives. Discussion Paper, National Academy of Medicine, Washington, DC. https://doi.org/10.31478/201809c
- Ommaya, A. K., P. F. Cipriano, D. B. Hoyt, K. A. Horvath, P. Tang, H. L. Paz, M. S. DeFrancesco, S. T. Hingle, S. Butler and C. A. Sinsky. 2018. Care-Centered Clinical Documentation in the Digital Environment: Solutions to Alleviate Burnout. NAM Perspectives. Discussion Paper, National Academy of Medicine, Washington, DC. https://doi.org/10.31478/201801c
- Brigham, T., C. Barden, A. L. Dopp, A. Hengerer, J. Kaplan, B. Malone, C. Martin, M. McHugh, and L. M. Nora. 2018. A Journey to Construct an All-Encompassing Conceptual Model of Factors Affecting Clinician Well-Being and Resilience. NAM Perspectives. Discussion Paper, National Academy of Medicine, Washington, DC. https://doi.org/10.31478/201801b
- Shipman, S. A. and C. A. Sinsky. 2013. Expanding Primary Care Capacity by Reducing Waste and Improving the Efficiency of Care. Health Affairs 32(11). https://doi.org/10.1377/hlthaff .2013.0539