Chronic Disease Prevention: Tobacco, Physical Activity, and Nutrition for a Healthy Start: A Vital Direction for Health and Health Care
 This publication is part of the National Academy of Medicine’s Vital Directions for Health and Health Care Initiative, which commissioned expert papers on 19 priority focus areas for U.S. health policy by more than 100 leading researchers, scientists, and policy makers from across the United States. The views presented in this publication and others in the series are those of the authors and do not represent formal consensus positions of the NAM, the National Academies of Sciences, Engineering, and Medicine, or the authors’ organizations.
Learn more: nam.edu/VitalDirections
This publication is part of the National Academy of Medicine’s Vital Directions for Health and Health Care Initiative, which commissioned expert papers on 19 priority focus areas for U.S. health policy by more than 100 leading researchers, scientists, and policy makers from across the United States. The views presented in this publication and others in the series are those of the authors and do not represent formal consensus positions of the NAM, the National Academies of Sciences, Engineering, and Medicine, or the authors’ organizations.
Learn more: nam.edu/VitalDirections
Smoking, obesity, inactivity, and excess intakes of added sugar, saturated fats, and salt are major contributors to the rates of chronic disease in the United States, and the prevalence and costs of chronic diseases associated with those modifiable behaviors account for a growing share of our gross domestic product. Our medical system has evolved to treat people for diseases that result from these behaviors rather than to prevent the diseases. However, as described in the following sections, the prevalence of the diseases associated with the behaviors greatly exceeds the capacity of our medical system to care for people who have them. Furthermore, few providers are trained to deliver effective behavioral-change strategies that are targeted at the risk factors to prevent their associated diseases. There is a need for broader preventive solutions that focus on the social and environmental determinants of chronic diseases.
A variety of policy and environmental changes have begun to improve those health-related behaviors through deterrents, such as tobacco taxes, or through product reformulation, such as reduction in the sodium content of processed foods. But the contributions of tobacco use, inactivity, and poor diet to chronic-disease rates remain high, and efforts to prevent and control the co-occurring epidemics of obesity, cardiovascular disease, diabetes, and cancer must be sustained. The success of these efforts requires multicomponent strategies implemented in multiple sectors and settings. Many of the strategies are being undertaken. In the sections that follow, we expand on the magnitude of the challenge, point to successful initiatives that are underway, and identify the most promising opportunities. Perhaps the biggest challenge is in learning how to implement what we know needs to be done.
The Magnitude of the Challenge: Key Issues and Cost Implications
Tobacco
Despite substantial efforts to prevent the onset of smoking and increase rates of smoking cessation, smoking is still a major cause of chronic obstructive pulmonary disease, heart attack, and lung cancer. For every person who dies from smoking, 20 suffer serious smoking-related illnesses. Smoking costs the United States $170 billion in health care expenditures and $156 billion in lost productivity—a total economic impact of $326 billion—per year (CDC, 2016).
Obesity
According to the National Health and Nutrition Examination Survey (NHANES), conducted by the Centers for Disease Control and Prevention (CDC), obesity is present in almost 38% of US adults (Ogden et al., 2015), is a major cause of heart disease and type 2 diabetes mellitus, and is associated with 16–20% of adult cancers. Rates of obesity and severe obesity are greatest in Hispanic and black women. A recent estimate suggested that the medical costs of adult obesity in the United States amounted to almost $150 billion per year (Finkelstein et al., 2009).
Some 17% of US children and adolescents have obesity. Although national rates of obesity in children 2–5 years old have recently decreased and rates in older children appear to have stabilized (Ogden et al., 2015), rates of severe obesity in children have increased (Ogden et al., 2016). The increase in the prevalence of severe obesity in children and adults suggests that the associated medical costs will increase. Those observations emphasize the need for continued efforts to prevent obesity in children and young adults and to improve the efficacy and cost-effectiveness of treatment in these groups. “Issue fatigue” and the cultural normalization of obesity constitute major challenges.
Food and Beverages that Contribute to Obesity
Patterns of consumption of foods and beverages that contribute to obesity offer opportunities for improvement and help to identify the ethnic differences that contribute to diet-related health inequities. In 2009–2010, highly processed foods accounted for 58% of total energy intake (TEI) and 90% of energy intake from added sugars (Steele et al., 2016). Sugar drinks (SDs)—sodas, non-100% juices, isotonic and energy drinks, and sweetened teas and coffees—are the largest contributors to sugar intake and accounted for about 150 kcal/day in youth and adults in 2009–2010 (Kit et al., 2013). Despite recent reductions in mean SD consumption, the prevalence of sports/energy drink consumption more than doubled from 1999–2000 to 2007–2008 in all age groups, and the prevalence of heavy SD consumption (≥500 kcal/day) increased in children 2–11 years old and was unchanged in adults (Han and Powell, 2013). The types of SDs consumed vary, but black children and adolescents and low–socioeconomic status children, adolescents, and adults are more likely to be heavy SD consumers (Han and Powell, 2013). Low-cost targeted advertising and the wide availability of SDs contribute to increased consumption by those groups.
Consuming foods away from home (FAFH), particularly from restaurants, has increased in the last few decades. Consumption of FAFH accounted for 18% of TEI in 1977–1978 and 34% in 2010–2012 (USDA, no date). In 2007–2008, 33%, 41%, and 36% of children, adolescents, and adults, respectively, consumed foods or beverages from fast-food restaurants on a given day, which accounted for an average of 10%, 17%, and 13% of TEI (Powell et al., 2012). Black adolescents and adults are more likely than their white counterparts to consume foods from fast-food restaurants (Powell et al., 2009), in part because of the cost of fast foods and because fast-food restaurants are heavily concentrated in their communities. Both the portion size and the caloric content of FAFH may contribute to the consumption of excess calories and to obesity.
Fruits and Vegetables
Fruit and vegetable consumption continues to fall short of recommended intakes. According to the 2007–2010 NHANES, 75% and 87%, respectively, of the US population do not meet their sex–age group recommended fruit and vegetable intakes. In particular, 93% of children consume less than the recommended intake of vegetables (NCI, 2015). Black men and women consistently report lower vegetable intake than their white counterparts (Kant et al., 2007). In 2013, 22% of adults and 39% of high school students reported consuming vegetables less than once per day; consumption by blacks and Hispanics was even less frequent. Expense and availability are major barriers to increasing consumption.
Sodium
The average sodium intake in the United States is 3,400 mg/day, well above the 2015 Dietary Guidelines for Americans recommendation of 2,300 mg/day (Dietary Guidelines Advisory Committee, 2015). It is estimated that a 40% reduction in US sodium intake would save 280,000–500,000 lives over the next 10 years. Adults who have prehypertension or hypertension, which together affects 32% of US adults, or over 70 million people, would benefit from further reduction to 1,500 mg/day (Dietary Guidelines Advisory Committee, 2015). However, because most of the sodium in foods is added during processing by the food and restaurant industry (Dietary Guidelines Advisory Committee, 2015), it is difficult for consumers to regulate their intake. Educational efforts directed at sodium reduction have had limited success. Therefore, policy efforts to reduce sodium and cardiovascular diseases are warranted.
Physical Activity
About 6–10% of all deaths from chronic diseases worldwide can be attributed to physical inactivity. Regular physical activity reduces the risk of premature death and disability from a variety of conditions, including coronary heart disease, diabetes, osteoarthritis, osteoporosis, and some types of cancer. According to CDC, only about 20% of US adults and less than 30% of high-school students meet the 2008 Physical Activity Guidelines for Americans (Physical Activity Guidelines Advisory Committee, 2013). The public health goal is to get people moving—some activity is better than none, and more is better than some.
A wide array of physical-activity interventions have proved effective in a variety of populations and geographic settings (IOM, 2013a; Task Force on Community Preventive Services, 2016). The National Physical Activity Plan (NPAP (2016) has extended the Guidelines in a comprehensive set of evidence-based strategies and tactics to increase physical activity in all segments of the US population. Each of the plan’s “societal sectors” articulates multiple strategies, and each strategy includes multiple tactics.
Opportunities for Progress and Policy Implications
The following sections recommend efforts to prevent and control tobacco use, improve levels of physical activity and dietary intake, and reduce obesity, with emphasis on opportunities and policies that will prevent chronic diseases.
Tobacco
Since 1965, the year after publication of the US Surgeon General’s first report linking cigarette smoking to lung cancer in men (US Public Health Service, 1964), reduction in smoking rates due to the effectiveness of tobacco control advocacy and policy adoption policies, and advocacy efforts has saved about 8 million lives in the United States. Nearly one-third of the 10-year increase in average adult life expectancy since 1965 is due directly to lower smoking rates.
However, cigarette smoking persists as the leading preventable cause of death in the United States, and an estimated 480,000 people die each year from cigarette smoking and exposure to secondhand tobacco smoke. Since 1965, cigarette smoking has taken more than 20 million lives. Tobacco manufacturers have continued to market their products aggressively to the most vulnerable members of our society, particularly those who have less education and lower socioeconomic status, while engineering their products for maximum addictive effect. Another critical aspect of the tobacco epidemic is that people who have mental illnesses have roughly twice the rate of smoking prevalence of the overall population. As many as half the cigarettes smoked in the United States are consumed by people who have co-occurring psychiatric or addictive disorders.
The 50th anniversary report of the surgeon general, published in 2014, states that “the burden of death and disease from tobacco use in the United States is overwhelmingly caused by cigarettes and other combusted tobacco products; rapid elimination of their use will dramatically reduce this burden.” Although it is imperative to continue public health efforts to reduce the use of all forms of tobacco, the conventional cigarette remains by far the most important target.
Current Successes in Tobacco
Clear guidelines exist for tobacco control. CDC’s Best Practices for Comprehensive Tobacco Control Programs—2014 sets forth a comprehensive, science-based plan to reduce tobacco use, smoking prevalence, and exposure to secondhand tobacco smoke (CDC, 2007). Each of the approaches outlined below has been pursued at both federal and state levels. These policy interventions have proved highly effective in the general population and have also reduced disparities by accelerating reductions in tobacco use by the most vulnerable members of society. The strategies include the continued promotion and enforcement of smoke-free environments, increased taxes on tobacco products, aggressive public-information campaigns, and carefully targeted litigation against the tobacco industry by the government and the private sector. The Patient Protection and Affordable Care Act (ACA) provides for tobacco-dependence treatment for the 70% of smokers who wish to quit. Wide availability of such treatment is critical for its success.
Policy Needs in Tobacco
The advent of new nicotine-delivery products, such as electronic cigarettes, requires new smoke-free, youth access, and other tobacco-control policies. Nicotine poisoning in children as a result of exposure to the liquid used in these devices is a growing problem. The Food and Drug Administration’s Center for Tobacco Products, which was formed pursuant to the Family Smoking Prevention and Tobacco Control Act, should use its authority to order product changes that are designed to render tobacco products less harmful and less addictive or even nonaddictive and to better inform the public about the hazards posed by these products through improved labeling and other communication tools.
As described later, some of the most promising strategies for reducing tobacco use are to increase the age at which cigarettes can be purchased, to increase taxes on tobacco, and to limit access to nicotine-containing products.
Nutrition, Physical Activity, and Obesity: Existing Efforts and Policy Improvements
Early Care and Education: Current Successes in Nutrition and Activity
Most US children, including almost half of those under 6 years old, spend an average of 35 hours a week in nonparental care. Early care and education (ECE) facilities include child-care centers, day-care homes, Head Start programs, and preschool and prekindergarten programs and are ideal settings in which to implement nutrition and physical activity strategies to prevent obesity. Interventions in ECE settings that have effectively reduced excess weight gain in young children incorporate both nutrition and physical activity (Dietary Guidelines Advisory Committee, 2015). The interventions include improvements in the nutrition quality of meals and snacks, in the mealtime environment, and in food-service practices; increases in physically active play; reductions in sedentary behaviors, such as watching television; improvements in outdoor play environments; enhancement of classroom education in nutrition and physical activity; and outreach to engage parents about making changes in the home environment. Two Institute of Medicine (IOM) committee reports (IOM, 2011, 2013b) include recommendations for improving nutrition and physical activity in ECE settings. Nonetheless, more evidence on the effects of these strategies on early childhood obesity is warranted.
Policy Needs in Nutrition and Activity
A variety of existing or emergent policy opportunities can improve nutrition and physical activity in ECE settings. The US Department of Agriculture (USDA) plays a central role. Implementation of the revised Child and Adult Care Food Program (CACFP) will improve nutrition standards and meal requirements. The challenge is in the implementation of the policies and programs. USDA can work with state agencies to increase participation in the CACFP through program simplification, paperwork reduction, and other strategies. In addition, USDA could seek the authority needed to require adequate daily physical activity and limits on television watching as conditions of participation in the CACFP. Within the Department of Health and Human Services (DHHS), Head Start performance standards should reflect an increased emphasis on healthy eating and physical activity, including increasing linkages to community resources, staff training, and parent engagement.
Schools
Children and adolescents consume up to 50% of their total daily calories in school, and USDA’s National School Lunch Program (NSLP) and School Breakfast Program (SBP) are key components of the school food environment. Those programs are important for all youth but are especially important for the more than 21.5 million school-age children in low-income families who receive free or reduced-price school meals.
Current Successes in Schools
The Healthy, Hunger-Free Kids Act (HHFKA) of 2010 directed USDA to update and revise nutrition standards for the NSLP and SBP. The standards, implemented in 2012, were based on recommendations in the IOM report School Meals: Building Blocks for Healthy Children (IOM, 2009) and required schools to offer more servings and more varieties of fruits and vegetables, more whole grains, and less saturated fats and sodium and to set limits on portion size. Recent studies have shown substantial improvements in the nutritional content of school meals, plate waste has not increased, and student acceptance of the healthier offerings is high and improving (Cohen et al., 2014).
A number of other policies and programs that are now in place can help to improve children’s nutrition in school, such as federal school wellness policies, farm-to-school programs that focus on fruits and vegetables, and the Fresh Fruit and Vegetable Program. Those programs foster a healthier food and activity culture, especially in schools in low-income communities.
Policy Needs in Schools
The HHFKA also mandated that free potable water be available where meals are served. However, the recent water crisis in Flint, Michigan, has renewed concerns about water safety, particularly in older schools. A national task force should be formed to address the scope of the issue and possible remedies, including providing funds to health departments for testing water supplies for lead and other contaminants.
In addition to school meals, foods and beverages available to students throughout the school day can contribute to a child’s excess calorie intake, such as those sold a la carte in school cafeterias, vending machines, and school stores (competitive foods). The IOM report Nutrition Standards for Foods in Schools: Leading the Way Toward Healthier Youth (IOM, 2007) concluded that school breakfast and lunch programs should be the main source of nutrition in school, that opportunities for competitive foods should be limited, and that if competitive foods are available, they should consist of nutritious fruits, vegetables, whole grains, and nonfat or low-fat milk and dairy products. The 2010 HHFKA required USDA for the first time to establish minimum nutrition standards for competitive foods (Smart Snacks), which were implemented in 2014.
As with ECE, the challenge is in implementation, such as meeting the increased cost of serving healthier meals (for example, more fruits, vegetables, and whole grains) and updated kitchen equipment and storage, staff training, and technical assistance. Congress, USDA, and states need to find innovative ways to ensure training and technical assistance that address those needs and the added cost of healthier meals. Adequate resources should be provided to monitor effects and scale up these and other interventions as appropriate.
School wellness policies are an important mechanism for engaging families and communities in schools and thereby for increasing the likelihood of sustaining and expanding the programs. USDA should complete regulations related to local wellness policies and work actively with states and localities on full implementation.
Because most children are enrolled in formal education programs at the pre-K, K–12, or postsecondary level, the education sector offers an important opportunity to increase physical activity. The recent revision of the NPAP includes a number of recommendations for the education sector. The plan recommends that states implement standards to ensure that children in child care and early-childhood education programs are appropriately physically active. Furthermore, as we emphasize in “Vital Directions” below, states and local school districts should adopt the Comprehensive School Physical Activity Program (CSPAP) model, including provision of high-quality physical education, in K–12 schools. Opportunities and incentives to adopt and maintain physically active lifestyles should be extended to students and employees in postsecondary education institutions.
Worksites
Workplace health promotion (wellness) programs can potentially reach a large segment of adults who are not otherwise exposed to or engaged in organized health-improvement efforts. Employers have a strong incentive to keep people healthy because healthy and fit workers are absent less often, are more productive in their jobs, have fewer accidents, and consume fewer expensive health care resources than workers who are at risk for or suffering from illness because of their health behaviors. However, most employers lack the skills, knowledge, and resources needed to build and sustain effective wellness programs.
Current Successes in Worksites
Research has demonstrated that properly designed, appropriately implemented, and rigorously evaluated programs can improve workers’ health, reduce the rate of increase in health care spending, and improve employee productivity. A 2010 systematic review by CDC’s Task Force on Community Preventive Services found that evidence-based wellness programs exert a favorable influence on health behaviors (for example, with respect to smoking, diet, physical activity, alcohol consumption, and seatbelt use), on such biometric measures as blood pressure and cholesterol, and on organizational outcomes important to employers, such as health care use and worker productivity (Soler et al., 2010). A widely cited meta-analysis of the literature on medical costs, medical-cost savings, and absenteeism associated with wellness programs estimated returns on investment averaging $3.27 and $2.70 saved over 3 years, respectively, for every $1.00 invested (Baicker et al., 2010).
Policy Needs in Worksites
The federal government can play an important role in engaging the business community in building and sustaining effective workplace health-promotion programs. Because the federal government spends more than $40 billion per year on health care for 8 million employees and annuitants (OPM, 2016), there is potential for substantial cost savings through improvement in government workers’ health and well-being and reduced spending. As the nation’s largest employer, the federal government should lead by example by implementing evidence-based programs in all federal agency worksites.
The federal government should also improve communication and dissemination of best and promising practices associated with workplace health promotion. The strategies require up-front investment, but they will yield a large return on investment to the federal government and the business community in general.
Federal support for the CDC resource center, the Guide to Community Preventive Services (Community Guide), and similar dissemination outlets will ensure that the right audiences learn from best and promising practices. Similar communication and dissemination programs should be established in other agencies, such as the Department of Labor, and nonprofits, including the US Chamber of Commerce, in which ideas, experiences, and resources become available through learning cooperatives, newsletters, webinars, and Wikipedia-like computer applications.
The federal government should also provide incentives to implement high-quality and innovative programs. The ACA authorized $200 million for workplace health-promotion pilot efforts, but the funds were never appropriated. The small amount of funding, $10 million per year, set aside for CDC-supported workplace health-promotion programs and research has been eliminated in the federal budget. Those funds should be restored. In addition, “smart” incentive programs should be encouraged. Section 2705 of the ACA allows employers to reduce insurance premiums to employees who participate in wellness programs and, under some conditions, to offer financial incentives for achieving specific health outcomes, such as quitting smoking, losing weight, managing blood pressure or cholesterol concentrations, and lowering blood glucose concentrations. Employees affected by evolving incentive rules should be included in the programs’ design to avoid the possibility of cost-shifting and discrimination based on preexisting conditions.
Communities
Policy Needs in Communities
Community initiatives to address nutrition, physical activity, and obesity include joint-use agreements for the after-hours use of school facilities for physical activity. States and communities can adopt Complete Streets policies to ensure that active modes of transportation are included in the planning, design, and construction of roadways. The National Complete Streets Coalition maintains a database that includes a template for model policies. Implementation of state, regional, and local land-use policies, comprehensive plans, subdivision regulations, and zoning codes that support physical activity by encouraging mixed uses and infrastructure for short-distance trips, such as walking or taking public transit from home to work, could substantially increase physical activity and thereby reduce the incidence of a number of chronic diseases.
As indicated earlier, research shows that the consumption of SDs is a major contributor to obesity and diabetes. An SD excise tax of $0.01 per ounce in the United States has emerged as one of the policy changes that can potentially slow the growth in obesity prevalence in children and adults, prevent new cases of obesity, improve quality-adjusted and disability-adjusted life-years and mortality, and save much more in health care costs over the next decade than the intervention costs to implement—a saving of an estimated $31 for every dollar spent on the intervention (Gortmaker et al., 2015).
Early data indicate that excise taxes have reduced consumption of SDs in Berkeley, California, and sales in Mexico, and the recently passed beverage excise tax in Philadelphia, Pennsylvania, will be a substantial source of revenue for the city’s pre-K program. State and municipal government procurement policies that specify foods with lower amounts of sodium and added sugars, like those in place in the federal government, will improve the health and productivity of the workforce and ultimately reduce the costs associated with obesity. CDC should work with local and state health departments to identify and disseminate model programs.
DHHS initiatives have supported CDC’s programs in community health that target obesity, nutrition, physical activity, and tobacco. Over the last 10–15 years, annual funding of over $100 million has supported a variety of programs, such as Racial and Ethnic Approaches to Community Health, the Steps to a Healthier US Initiative (targeting asthma, diabetes, and obesity), Communities Putting Prevention to Work, and Community Transformation Grants (as part of the ACA). Those funds have been substantially reduced, but the growing evidence of the value of social-environmental interventions in communities to improve behavior and health outcomes (Evaluating obesity prevention efforts, 2015) emphasizes that funding for the programs should be restored and sustained.
Medical Settings
Current Successes in Medical Settings
Because people who have severe obesity probably will not achieve substantial weight loss solely in response to the policy and environmental changes outlined here, new effective treatment strategies will be required. The Diabetes Prevention Program (DPP) is a model of care that demonstrated that counseling about nutrition, physical activity, and weight loss in adults who had obesity and prediabetes was more effective than medication in the prevention of the development of type 2 diabetes (Knowler et al., 2002). The DPP was adapted for delivery by trained providers in community settings by the Y-USA, and outcomes were comparable with those observed in the DPP and at lower cost. The DPP in community settings is an ideal example of value-based care inasmuch as payment occurs only if enrollees meet specific attendance and weight-loss goals. The Centers for Medicare & Medicaid Services recently announced that it would expand Medicare to cover programs to prevent diabetes. Like Medicare, state Medicaid programs should expand coverage for the prevention of diabetes that includes the delivery of the DPP in community settings by qualified providers.
Policy Needs in Medical Settings
Lack of a standard of care and lack of payment for obesity treatment are major barriers to the effective medical management of obesity. US Preventive Services Task Force recommendations for treatment for adult and childhood obesity have recommended intensive behavioral interventions, defined as at least 26 hours for children and 6 months of visits every 2 weeks for adults. Both recommendations received a B rating from the task force. Because the DPP constitutes an effective weight-loss program, this weight-loss therapy should be expanded to Medicaid with payment if patients meet identified attendance and weight-loss goals.
Medical solutions alone are inadequate to address diseases as prevalent as obesity, diabetes, and cardiovascular disease. Although incentives to integrate clinical and community services have begun, studies that demonstrate the business case for integration could speed the development and implementation of this approach. The Center for Medicare and Medicaid Innovation should fund studies that explore the effects of delivery of services for chronic diseases that integrate clinical and community services for the prevention and treatment of obesity (Dietz et al., 2015). Such studies should assess how to reimburse community systems when community interventions add health value.
Physicians and other health care providers are trusted advocates of favorable health behaviors, and the health care system has the potential to influence physical activity at the individual and population level. However, assessment of and counseling for both physical activity and dietary intake are not well established in clinical practice in the United States. Only about one-third of patients report receiving such counseling during office visits. In contrast with nutritional counseling, in which registered dietitians constitute an existing workforce, few providers are trained in counseling about physical activity. Because physical activity has such a powerful effect on the prevention and mitigation of many chronic diseases, the NPAP recommended several strategies to enhance the role of health care providers in promotion of physical activity. They included the recommendation that DHHS establish physical activity as a “vital sign” that all health care providers assess and discuss with their patients. DHHS should also support inclusion of physical activity in clinical guidelines for management of conditions for which there is evidence of health and cost benefits. Organizations that assess the quality of care should review the implementation of these practices in health systems. The lack of reimbursement for providers who help patients to improve their diet and physical activity level is a major barrier to clinical efforts to prevent and treat for obesity and chronic diseases related to it.
Health in All Policies of State and Local Governments
Multiple community strategies have been developed to address the food environment, but fewer have been directed at increasing physical activity. The principles outlined below are specific to physical activity but also apply to improving nutrition.
Policy Needs in State and Local Health
State and local health departments are essential actors in promoting physical activity interventions because of their ability to assess public health problems, develop appropriate programs and policies, and ensure that the programs and policies are effectively delivered and implemented. Fulfilling their obligation to promote physical activity in a variety of community settings will require several steps. CDC’s Community Guide has established a number of evidence-based strategies to increase physical activity. They should be widely disseminated.
Leadership, funding, and workforce capacity are important barriers to the implementation of evidence-based recommendations to improve the food environment and increase physical activity. State and local governments should be funded to provide coordinated leadership and support for efforts to promote physical activity, particularly efforts focused on high-risk populations, by increasing resources and strengthening policies in all sectors related to physical activity and nutrition. Improved support for evidence-based programs can be accomplished by identifying new funding opportunities and redirecting existing funding to issues, such as physical inactivity, that result in high health and economic burdens for society. In collaboration with the Association of State and Territorial Health Officers and the National Association of City and County Health Officers, new curricula should be developed in schools and programs in public health, and short courses for practitioners and certification by such groups as the National Physical Activity Society should be developed to help public health practitioners to develop cross-sectoral partnerships and implement evidence-based physical activity interventions. Sectors should include education, parks and recreation, transportation, city planning, business, nonprofit organizations, and health care; all have a role in increasing physical activity. Those steps should be complemented by the development and maintenance of an ethnically diverse, culturally diverse, and sex-diverse public-health workforce with competence in physical activity, nutrition, and health through new curricula in training programs and with scholarship support for underrepresented minority groups and disadvantaged populations.
Federal and Cross-Sector Initiatives
Policy Needs for Federal and Cross-Sector Initiatives
More national, state, and local initiatives have focused on nutrition than on physical activity. Achieving progress in promoting physical activity will involve sectors outside health care and public health. To implement effectively many of the strategies outlined above, a set of diverse sectors needs to be engaged. Promotion of physical activity may not be seen as a primary objective of many sectors (such as schools and transportation), but strategies will often have benefits that resonate with multiple sectors. For example, a strong set of actions to support physical education in schools will increase rates of physical activity and may also improve student achievement (CDC, 2010). In cross-sector efforts, high priority should be given to improving access to physical activity-related services and opportunities, particularly for disadvantaged populations that have limited access (Committee on Prevention of Obesity in Children and Youth, 2005; National Physical Activity Plan Alliance, 2016). In communities that receive support from the Prevention and Public Health Fund (which resulted from the ACA), high priority should be given to the development of infrastructure for underserved populations. CDC should identify successful cross-sector partnerships so that it can identify key elements of success and incorporate them into future physical-activity initiatives.
Because physical activity has such benefits for a wide array of chronic diseases, DHHS should establish at CDC an Office of Physical Activity and Health and allocate to it the resources needed to provide effective national leadership in identifying, implementing, and monitoring high-impact strategies for promotion of physical activity.
Public-Private Partnerships
Current Successes in Obesity Reduction
The nationwide concern about the obesity epidemic in children and adults has engaged organizations and businesses that want to help, especially with regard to children. Many efforts have been undertaken by single sectors or companies, but there have been several important public-private partnerships, the most notable being the Partnership for a Healthy America (PHA). PHA was founded in 2010 in conjunction with Let’s Move! and remains an independent nonpartisan organization. PHA works with public, private, and nonprofit leaders to make voluntary commitments to address childhood obesity. Large grocery chains have committed to reducing added sugars and sodium in store brand foods and increasing access to healthy foods in food deserts, hotel and restaurant chains are reducing their calorie footprint, and colleges and hospitals around the country are adopting nutrition and physical activity criteria. Notable in the PHA approach is the third-party validation to collect data, monitor progress, and report findings publicly each year (http://ahealthieramerica.org/about/annual-progress-reports/[accessed March 30, 2016]). The connection of PHA to the Obama Administration has facilitated improved business practices that affect the health of children and families. PHA’s approach should be adopted by the next administration.
The Healthy Food Financing Initiative (HFFI) is a program through which the federal government (Department of the Treasury, USDA, and DHHS) has provided financial assistance to local development agencies, such as low-interest loans, to improve food access. The funds have enabled private developers to build supermarkets and convenience stores and to establish farmer’s markets in neighborhoods that were formerly classified as food deserts. The HFFI also provides employment opportunities in neighborhoods that have high unemployment rates. States and some cities have established programs for the same purpose that engage the private sector.
Policy Needs in Obesity Reduction
Because access to supermarkets constitutes a major inequity, funding for the HFFI should be sustained. However, some early data suggest that although new supermarkets provide increased access, dietary intakes may not change; access alone might not improve diets (Dubowitz et al., 2015). Both the short- and the longer-term effects of new supermarkets on dietary intake and health should be evaluated. This funding approach should also be explored relative to other issues, such as the development of small-city green spaces and parks as places to increase opportunities for physical activity.
Such programs as Double Up Food Bucks (2016) double the value of federal nutrition assistance (usually the Supplemental Nutrition Assistance Program, SNAP) used predominantly in farmer’s markets, helping low-income people to purchase more locally grown fruits and vegetables. Funds for such programs often come from foundations and the private sector. The return on this investment is threefold: low-income consumers eat more healthful food, local farmers gain new customers and make more money, and more food dollars stay in the local economy.
On the basis of the success of SNAP incentive programs, the 2014 Farm Bill included $100 million for Food Insecurity Nutrition Incentive grants. All the projects funded through these grants include a public-private component through the contribution of matching funds. Support for this program should be sustained and expanded.
Support for programs like the HFFI is closely connected to the growing interest in the linkage between community development, housing, and health led by the Federal Reserve Bank of San Francisco and its sister banks (Moon, 2016). Federal Reserve’s interest grew out of the recognition that life expectancy was widely divergent between nearby ZIP codes and that improved housing can directly improve health and well-being. Furthermore, indirectly subsidized housing frees low-income families’ resources so that they can buy food, pay for medicine, or support their children’s school costs. In addition to its support for low-income housing, Federal Reserve banks help to direct funding for supermarkets in food deserts and charter and other schools and additional investments amounting to about $100 billion per year (Erickson and Andrews, 2011; David Erickson, personal communication), and they have urged the inclusion of health benefits in the assessment of community-development funding projects.
Few sources of funding for housing projects have used health benefits as a justification for funding, and there are still only early efforts to understand how health improvements can be measured and monetized to capture the added value. Policies that lower the capital costs of developments that include elements to improve health could be expected to influence billions of dollars in new investment each year. Pilot and modeling studies should be funded to identify the most promising strategies and to make the business case their impact on health.
A sustainable food system provides nutritious and safe food while ensuring that ecosystems can provide food for future generations; develops agricultural and production practices that reduce environmental effects and conserve resources; makes healthy food available, accessible, and affordable to all; and is humane and just, protecting farmers and other workers, consumers, and communities. Recognizing that the US food-supply chain is deeply interconnected with human and environmental health and with social and economic systems, IOM convened a public workshop in 2013, “Mapping the Food System and its Effects (IOM, 2013c), and later released a committee report, A Framework for Assessing Effects of the Food System (IOM, 2015a). Those activities led the 2015 Dietary Guidelines Advisory Committee to link public health, food systems, and sustainability; and for the first time, the committee recommended food-system sustainability as part of the Dietary Guidelines for Americans (Dietary Guidelines Advisory Committee, 2015). The committee concluded that “a dietary pattern that is higher in plant-based foods, such as vegetables, fruits, whole grains, legumes, nuts and seeds, and lower in animal-based foods is more health promoting and is associated with lesser environmental impact (greenhouse gas emissions and energy, land, and water use) than is the current average U.S. diet.” Federal, state, and local governments should develop public-education campaigns that focus on the benefits of a more plant-based diet and on the health and planetary benefits of reduced meat consumption. The 2020 Dietary Guidelines for Americans will provide an opportunity to revisit this issue.
Metrics and Monitoring
An important gap in many settings is the capacity to identify and disseminate model programs and to monitor the national uptake of these programs. Agencies within DHHS, most notably CDC, are ideally suited for that function. For example, because ECE settings have such a profound effect on young children, CDC should establish a national monitoring system to assess progress and policies that improve nutrition and physical activity in ECE settings. Although many workplaces have successful initiatives, the recognition and spread of successful programs remain low. Additional funds would enable CDC to conduct applied research in real world settings, to evaluate the effects of established and long-standing workplace programs, and to monitor uptake of worksite wellness practices throughout the United States. A portion of research funding should be directed at evaluating innovative programs aimed at improving the health and well-being of federal workers and members of the armed services. Active transportation, such as walking or biking, increases physical activity and reduces car use and thereby reduces the generation of greenhouse gases. CDC and the Department of Transportation have a joint interest in expanding the use and monitoring of policy and environmental approaches that increase walking, biking, or use of public transportation, all of which increase physical activity.
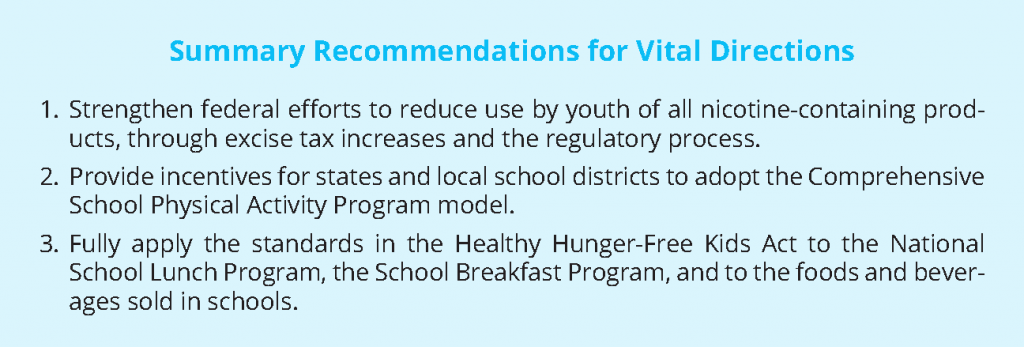
Vital Directions for Reducing Tobacco Use and Improving Nutrition and Physical Activity
The following vital directions were based on the authors’ consensus that these strategies were the most feasible and of those considered were likely to have the greatest effect.
Strengthen Federal Efforts to Reduce Use by Youth of All Nicotine-Containing Products, Through Excise Tax Increases and the Regulatory Process
Despite recent progress in reducing smoking rates, tobacco use remains the leading cause of preventable deaths in the United States. Abundant research demonstrates that later initiation of tobacco use is associated with lower = rates of addiction. Three strategies should be used to reduce the initiation of tobacco use. The policy likely to have the greatest population-based effect is raising the minimum age of tobacco purchase to 21 years (IOM, 2015b) and applying this minimum to all products that contain nicotine. The recent report that 24% of adolescents are using e-cigarettes compared with the 11% of adolescents who are smoking traditional cigarettes emphasizes the urgency of this step (Kann et al., 2016). Increased taxes on tobacco clearly reduce the initiation of smoking, and may also reduce smoking by people who are already addicted.
Fully Apply the Standards in the Healthy Hunger-Free Kids Act (HHFKA) to the National School Lunch Program, the School Breakfast Program, and to the Foods and Beverages Sold in Schools
The changes mandated by the HHFKA must be sustained. The HHFKA transformed the healthfulness of school meals, set limits on portion sizes, and set the first national nutrition standards for all foods and beverages sold in schools (Smart Snacks). Those changes resulted in an increase in the consumption of healthier foods, such as fruits and vegetables, without an increase in plate waste (Cohen et al., 2014). An evidence review and modeling of cost effectiveness of childhood nutrition interventions found that these improvements make the HHFKA “one of the most important national obesity-prevention policy achievements in recent decades” (Gortmaker et al., 2015). Of nine dietary interventions evaluated, improvements in school meals due to HHFKA were projected to have the largest effect on childhood obesity. For example, implementation of Smart Snacks was projected to prevent 345,000 cases of childhood obesity in 2025 and save more in reduced health costs over the next decade than the intervention would cost to implement. The net savings to society for each dollar spent was projected to be $4.56 (Gortmaker et al., 2015).
Provide Incentives for States and Local School Districts to Adopt the Comprehensive School Physical Activity Program Model (CSPAP)
States and local school districts should adopt the CSPAP model (CDC, 2013), including the provision of high-quality physical education, in K—12 schools. Although the HHFKA has transformed school meals, comparable progress has not been achieved in physical activity. Comprehensive programs for physical activity in schools include high-quality physical education; physical activity before, during, and after school; staff involvement; and family and community engagement. The recent NPAP, the National Physical Activity Guidelines for Americans, and the Institute of Medicine report Accelerating Progress in Obesity Prevention and Educating the Student Body point to the importance of physical activity in improving learning and behavior, preventing obesity, and reducing the risks of other chronic diseases and support the need for high-quality physical-education programs. Such programs may have the added benefit of increasing the number of recruits eligible for military service.
References
- Baicker, K., D. Cutler, and Z. Song. 2010. Workplace wellness programs can generate savings. Health Affairs (Millwood) 29(2):304-311. https://doi.org/10.1377/hlthaff.2009.0626
- CDC (Centers for Disease Control and Prevention). 2007. Best practices for comprehensive tobacco control programs. Atlanta, GA: CDC, U.S. Department of Health and Human Services. Available at: https://www.cdc.gov/tobacco/stateandcommunity/best_practices/index.htm (accessed July 28, 2020).
- CDC. 2010. The association between school-based physical activity, including physical education, and academic performance. Atlanta, GA: CDC. Available at: https://www.cdc.gov/healthyyouth/health_and_academics/pdf/pape_executive_summary.pdf (accessed July 28, 2020).
- CDC. 2013. Comprehensive school physical activity programs: A guide for schools. Atlanta, GA: CDC. Available at: https://www.cdc.gov/healthyschools/professional_development/e-learning/CSPAP/index.html (accessed July 28, 2020).
- CDC. 2016. Economic facts about U.S. tobacco production and use. Available at: http://www.cdc.gov/tobacco/data_statistics/fact_sheets/economics/econ_facts/ (accessed August 18, 2016).
- Cohen, J. F., S. Richardson, E. Parker, P. J. Catalano, and E. B. Rimm. 2014. Impact of the new U.S. Department of Agriculture school meal standards on food selection, consumption, and waste. American Journal of
Preventive Medicine 46(4):388-394. https://doi.org/10.1016/j.amepre.2013.11.013 - Institute of Medicine. 2005. Preventing Childhood Obesity: Health in the Balance. Washington, DC: The National Academies Press. https://doi.org/10.17226/11015
- Dietary Guidelines Advisory Committee. 2015. Scientific report of the 2015 Dietary Guidelines Advisory Committee. Washington, DC: US Department of Health and Human Services and US Department of Agriculture. Available at: https://health.gov/sites/default/files/2019-09/Scientific-Report-of-the-2015-Dietary-Guidelines-Advisory-Committee.pdf (accessed July 28, 2020).
- Dietz, W. H., L. S. Solomon, N. Pronk, S. K. Ziegenhorn, M. Standish, M. M. Longjohn, D. D. Fukuzawa, I. U. Eneli, L. Loy, N. D. Muth, E. J. Sanchez, J. Bogard, and D. W. Bradley. 2015. An integrated framework for the prevention and treatment of obesity and its related chronic diseases. Health Affairs (Millwood) 34(9):1456-1463. https://doi.org/10.1377/hlthaff.2015.0371
- Double Up Food Bucks: A win for families, farmers, and communities. 2016. Available at: http://www.doubleupfoodbucks.org/about/ (accessed April 10, 2016).
- Dubowitz, T., M. Ghosh-Dastidar, D. A. Cohen, R. Beckman, E. D. Steiner, G. P. Hunter, K. R. Flórez, C. Huang, C. A. Vaughan, J. C. Sloan, S. N. Zenk, S. Cummins, and R. L. Collins. 2015. Diet and perceptions change
with supermarket introduction in a food desert, but not because of supermarket use. Health Affairs (Millwood) 34(11):1858-1868. https://doi.org/10.1377/hlthaff.2015.0667 - Erickson, D., and N. Andrews. 2011. Partnerships among community development, public health, and health care could improve the well-being of low-income people. Health Affairs (Millwood) 30(11):2056-2063. https://doi.org/10.1377/hlthaff.2011.0896
- Evaluating Obesity Prevention Efforts: What have we learned? 2015. Available at: https://publichealth.gwu.edu/sites/default/files/downloads/Redstone-Center/Evaluating Obesity Prevention Efforts What Have We Learned.pdf (accessed July 31, 2016).
- Finkelstein, E. A., J. G. Trogdon, J. W. Cohen, and W. Dietz. 2009. Annual medical spending attributable to obesity: Payer- and service-specific estimates. Health Affairs (Millwood) 28(5):w822-w831. https://doi.org/10.1377/hlthaff.28.5.w822
- Gortmaker, S. L., Y. C. Wang, M. W. Long, C. M. Giles, Z. J. Ward, J. L. Barrett, E. L. Kenney, K. R. Sonneville, A. Sadaf Afzal, S. C. Resch, and A. L. Cradock. 2015. Three interventions that reduce childhood obesity are projected to save more than they cost to implement. Health Affairs (Millwood) 34(11):1932-1939. https://doi.org/10.1377/hlthaff.2015.0631
- Han, E., and L. M. Powell. 2013. Consumption patterns of sugar-sweetened beverages in the United States. Journal of the Academy of Nutrition and Dietetics 113(1):43-53. https://doi.org/10.1016/j.jand.2012.09.016
- Institute of Medicine. 2007. Nutrition Standards for Foods in Schools: Leading the Way Toward Healthier Youth. Washington, DC: The National Academies Press. https://doi.org/10.17226/11899
- Institute of Medicine. 2010. School Meals: Building Blocks for Healthy Children. Washington, DC: The National Academies Press. https://doi.org/10.17226/12751
- Institute of Medicine. 2011. Child and Adult Care Food Program: Aligning Dietary Guidance for All. Washington, DC: The National Academies Press. https://doi.org/10.17226/12959
- Institute of Medicine. 2013a. Educating the Student Body: Taking Physical Activity and Physical Education to School. Washington, DC: The National Academies Press. https://doi.org/10.17226/18314
- Institute of Medicine. 2013b. Evaluating Obesity Prevention Efforts: A Plan for Measuring Progress. Washington, DC: The National Academies Press. https://doi.org/10.17226/18334
- IOM. 2013c. Workshop on mapping the food system and its effects. Washington, DC: The National Academies Press.
- Institute of Medicine and National Research Council. 2015. A Framework for Assessing Effects of the Food System. Washington, DC: The National Academies Press. https://doi.org/10.17226/18846
- Institute of Medicine. 2015. Public Health Implications of Raising the Minimum Age of Legal Access to Tobacco Products. Washington, DC: The National Academies Press. https://doi.org/10.17226/18997
- Kann, L., T. McManus, W. A. Harris, S. L. Shanklin, K. H. Flint, J. Hawkins, B. Queen, R. Lowry, E. O’Malley Olsen, D. Chyen, L. Whittle, J. Thornton, C. Lim, Y. Yamakawa, N. Brener, and S. Zaza. 2016. Youth Risk Behavior Surveillance-United States, 2015. MMWR Surveillance Summaries 65(6):1-174. https://doi.org/10.15585/mmwr.ss6506a1
- Kant, A. K., B. I. Graubard, and S. K. Kumanyika. 2007. Trends in black-white differentials in dietary intakes of U.S. adults, 1971-2002. American Journal of Preventive Medicine 32(4):264-272. https://doi.org/10.1016/j.amepre.2006.12.011
- Kit, B.K., T. H. Fakhouri, S. Park, S. J. Nielsen, and C. L. Ogden. 2013. Trends in sugar-sweetened beverage consumption among youth and adults in the United States: 1999-2010. American Journal of Clinical Nutrition 98(1):180-188. https://doi.org/10.3945/ajcn.112.057943
- Knowler, W. C., E. Barrett-Connor, S. E. Fowler, R. F. Hamman, J. M. Lachin, E. A. Walker, and D. M. Nathan. 2002. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. New England Journal of Medicine 346(6):393-403. https://doi.org/10.1056/NEJMoa012512
- Moon, J. 2016. Investing to Reduce Economic and Racial Disparities. Available at: http://www.frbsf.org/community-devel-opment/blog/investing-to-reduceeconomic-racial-disparities/ (accessed August 1,
2016). - National Physical Activity Plan. 2016. Available at: http://www.physicalactivityplan.org/theplan.ph (accessed April 1, 2016).
- National Physical Activity Plan Alliance. 2016. The National Physical Activity Plan. Available at: http://www.physica-lactivityplan.org/index.php (accessed March 23, 2016).
- NCI (National Cancer Institute). 2015. Usual Dietary Intakes: Food Intakes, U.S. Population, 2007-10. Epidemiology Research Program Updated May 20, 2015. Available at: http://epi.grants.cancer.gov/diet/usualintakes/pop/2007-10/ (accessed March 23, 2016).
- Office of Personnel Management (OPM). 2016. Tribal Employers – General Information. Available at: https://www.opm.gov/healthcare-insurance/tribal-employers/generalinformation/ (accessed December 5, 2016)
- Ogden, C. L., M. D. Carroll, C. D. Fryar, and K. M. Flegal. 2015. Prevalence of obesity among adults and youth: United States, 2011–2014. Hyattsville, MD. National Center for Health Statistics Data Brief. Available at: https://www.cdc.gov/nchs/products/databriefs/db219.htm (accessed July 28, 2020).
- Ogden, C. L., M. D. Carroll, H. G. Lawman, C. D. Fryar, D. Kruszon-Moran, and K. M. Flegal. 2016. Trends in obesity prevalence among children and adolescents in the United States, 1988-1994 through 2013-2014. JAMA 315(21):2292-2299. https://doi.org/10.1001/jama.2016.6361
- Physical Activity Guidelines Advisory Committee. 2013. PAG Midcourse Report: Strategies to Increase Physical Activity Among Youth. Washington, DC: US Department of Health and Human Services. Available at: https://health.gov/our-work/physical-activity/previous-guidelines/2013-midcourse-report (accessed July 28, 2020).
- Powell, L. M., B. T. Nguyen, and E. Han. 2012. Energy intake from restaurants: Demographics and socioeconomics, 2003-2008. American Journal of Preventive Medicine 43(5):498-504. https://doi.org/10.1016/j.amepre.2012.07.041
- Soler, R. E., K. D. Leeks, S. Razi, D. P. Hopkins, M. Griffith, A. Aten, S. K. Chattopadhyay, S. C. Smith, N. Habarta, R. Z. Goetzel, N. P. Pronk, D. E. Richling, D. R. Bauer, L. R. Buchanan, C. S. Florence, L. Koonin, D. MacLean, A. Rosenthal, D. Matson Koffman, J. V. Grizzell, and A. M. Walker. 2010. A systematic review of selected interventions for worksite health promotion. The assessment of health risks with feedback. American
Journal of Preventive Medicine 38(2 Suppl):S237-S262. Available at: https://www.ncbi.nlm.nih.gov/books/NBK79491/ (accessed July 28, 2020). - Steele, E. M., L. G. Baraldi, M. L. da Costa Louzada, J. C. Moubarac, D. Mozaffarian, and C. A. Monteiro. 2016. Ultra-processed foods and added sugars in the US diet: Evidence from a nationally representative cross-sectional study. BMJ 6(3):e009892. https://doi.org/10.1136/bmjopen-2015-009892
- Task Force on Community Preventive Services. 2016. The guide to community preventive services: What works to promote health? Atlanta, GA: CDC. US Public Health Service. 1964. Available at: https://www.thecommunityguide.org/ (accessed July 28, 2020).
- Smoking and health: A report of the Advisory Committee to the Surgeon General of the Public Health Service. Washington, DC: US Public Health Service. Available at: https://www.cdc.gov/tobacco/data_statistics/sgr/history/index.htm (accessed July 28, 2020).
- USDA (US Department of Agriculture). No date. What we eat in America, NHANES 2011-2012, individuals 2 years and over (excluding breast-fed children), day 1. Available at: http://www.ars.usda.gov/nea/bhnrc/fsrg
(accessed April 6, 2016).