Can Breastfeeding Protect Against Childhood Obesity?
Breastfeeding offers numerous health benefits to children and women globally. For this reason, international health organizations and American expert groups strongly support this infant feeding behavior (Victora et al., 2016). Given the high cost-effectiveness of breastfeeding in the United States (Bartick and Reinhold, 2010; Bartick et al., 2013), the American Academy of Pediatrics (2014) and the American College of Obstetrics and Gynecology (2016) support exclusive breastfeeding for about 6 months followed by the continuation of breastfeeding until the infant is 1 year old once complementary foods are introduced at around 6 months.
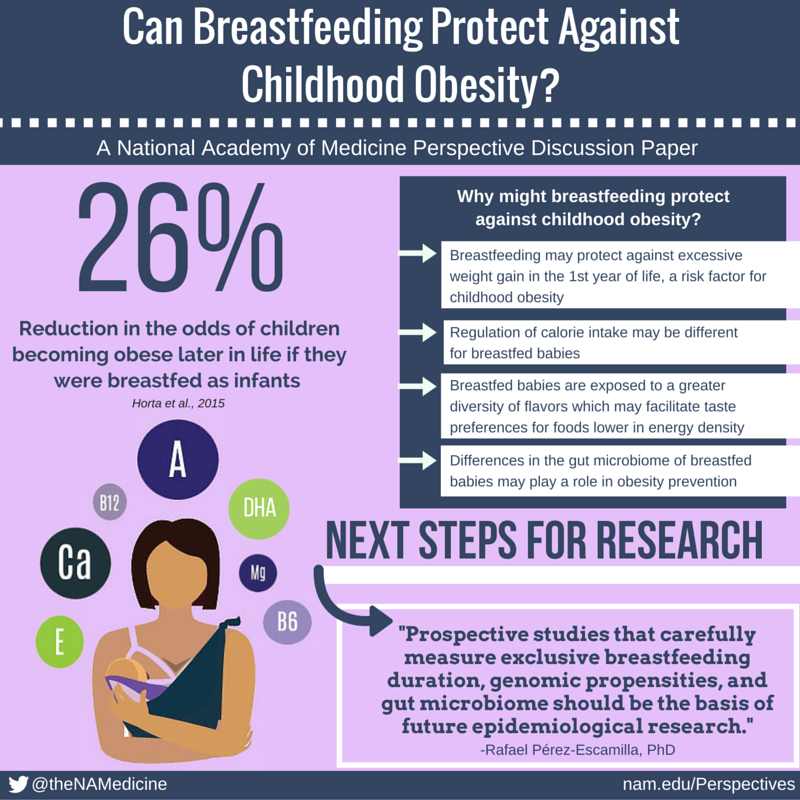
Although the evidence behind breastfeeding recommendations is overall consistent and strong (Victora et al., 2016), expert opinion is still divided on whether breastfeeding protects against the risk of childhood obesity or not (Casazza, 2013; Dewey, 2003; Victora et al., 2016). Thus, the objectives of this perspective are to (1) analyze the biological plausibility for expecting a causal relationship between breastfeeding and risk protection against childhood obesity, (2) present recent epidemiological evidence, and (3) identify future research areas to answer key remaining questions.
Biological Plausibility
A causal relationship between breastfeeding and childhood obesity risk is plausible. First, the endocrinological profiles of breastfed versus formula-fed infants including insulin and leptin levels suggest that breastfeeding may protect babies against the excessive deposition of body fat (Dewey, 2003; Geddes and Prescott, 2013; Koletzko et al., 2009; Luque et al., 2016). Strong and consistent evidence indicates that the overproduction of insulin in response to the relatively higher levels of protein in infant formula may explain, at least in part, the differences in endocrinological profiles between breastfed and formula-fed infants (Dewey, 2003; Koletzko et al., 2009; Luque et al., 2016; Weber et al., 2014). Second, breastfeeding may protect infants against gaining excessive weight during the first year of life, which in turn has been consistently identified as a risk factor for childhood obesity (Dewey, 1998; Koletzco et al., 2009; PérezEscamilla and Kac, 2013; Woo Baidal et al., 2016). Third, regulation of calorie intake may differ between breastfed and formula-fed babies. Whereas breastfed babies may self-regulate the amount of calories they consume based on the energy density of their mother’s milk (PérezEscamilla et al., 1995), it is possible that formula-fed babies may consume more calories, because the caregiver has more control of consumption. This may represent a risk for childhood obesity, especially if babies are pressured to finish the bottle (Li et al., 2014) and/or they are fed formula in large-sized bottles (Wood et al., 2016). Fourth, breastfed babies are exposed to a greater diversity of flavors, which may facilitate the development of taste preferences for fruits, vegetables, and other healthy foods that are lower in energy density (Mennella, 2014), which in turn may protect against the risk of childhood obesity (Pérez-Escamilla et al., 2012). Fifth, it has recently been proposed that the pronounced difference in gut microbiome in breastfed versus formula-fed infants may also be related to a lower risk of childhood obesity among breastfed babies (Woo and Martin, 2015).
Recent Epidemiological Evidence
Two recent meta-analyses assessed the global epidemiological evidence behind the hypothesis that breastfeeding offers protection against the development of childhood obesity. Horta et al. (2015), in a review of 105 studies, found a significant reduction—26 percent—in the odds of children becoming obese later in life if they were breastfed as infants. This systematic review covered evidence from low-, middle-, and high-income countries and did not impose restrictions in terms of the experimental or observational designs allowed. The studies varied widely on breastfeeding modalities and comparison groups included. The range of ages at which obesity was assessed was 1 year to more than 20 years of age, with the effect being less in older children. Also, the larger the sample size included in the study, the lower the effect size detected. In addition, there were differences between children born before 1980 and after 1980, perhaps related to differences in formula composition. Cohort studies tended to show the smallest effect size (odds ratio [OR] = 0.79) relative to case-control (OR = 0.68) and cross-sectional studies (OR = 0.67). In addition, the more adjustment that took place for confounding, the smaller the effect size. Effects sizes were almost identical across high-, middle-, and low-income countries, and exclusive breastfeeding tended to produce the strongest protection. When looking at the studies with the highest possible quality, the review found a statistically significant effect size of 13 percent in obesity risk reduction. The findings from this systematic review are fully consistent with previous reviews conducted over the past 15 years (Beyerlein and Von Kries, 2011; Dewey, 2003; Weng et al., 2012).
In the second meta-analysis, Giugliani et al. (2015) looked at 35 studies, but only 12 studies reported body mass index (BMI) or weight-for-length (or height). Of these, 10 were randomized control trials, and two were quasi experimental. The meta-analysis covered high-, middle-, and low-income countries and a wide variety of interventions and ages. Giugliani et al. found a reduction in the risk of childhood obesity as a function of maternal exposure to breastfeeding promotion and support programs. The overall effect was statistically significant although the effect size was small, a reduction of 0.06 Z score mean difference in BMI or weight-for-length (or height).
Effect Modification by Genomic Propensity to Obesity
In a study involving over 14,000 German children assessed for weight and height between 4.7 and 7.3 years of age, Beyerlein and Von Kries (2011) found that breastfeeding was associated with a lower BMI compared with formula feeding only among children with the highest BMI (i.e., the 90th and 97th BMI percentiles). This finding suggests that children with higher genomic propensity to become obese may benefit the most from breastfeeding when it comes to obesity risk. Subsequent studies (Dedoussis et al., 2011) found that particular alleles in the fat mass and obesity-associated (FTO) gene may help explain why breastfeeding protection is stronger among babies who have a genetic propensity to become obese. Specifically, two Greek cohort studies showed that although children or preadolescents who were not breastfed and who were carriers of the obesity propensity allele had higher BMI, weight-for-height, or waist circumference, no differences were found among the FTO genotype groups for any of the obesity indices in breastfed individuals. The researchers were unable to replicate the Greek findings with data from the United Kingdom Avon Longitudinal Study of Parents and Children (ALSPAC) cohort study, perhaps because these individuals were leaner than their Greek counterparts (Dedoussis et al., 2011). Consistent with the Greek findings, Abarin et al. (2012) found in Australia that among girls with an FTO obesity risk allele there was a dose-response relationship between how long they received only breast milk and the degree of protection against childhood obesity they received by 14 years of age. Among boys, how long they received only breast milk protected against the risk of obesity after 10 years of age among both carriers and noncarriers of an FTO obesity risk allele. Among boys who had an AA or AT genotype (mutations of the FTO gene that have been associated with obesity), none of them were overweight if they received only breast milk for 5 months. By contrast, over half of the boys with these genotypes who received only breast milk for less than 2 months were overweight. These findings strongly suggest that breastfeeding confers protection against obesity among children genetically predisposed to obesity (those with the AA or AT genotypes).
Discussion and Research Recommendations
Recent epidemiological evidence, including a major meta-analysis that adjusted for high heterogeneity across studies, strongly suggests that there is a significant, albeit small, overall effect of breastfeeding against childhood obesity in the general population (Victora et al. 2016). The finding that the effect size in the general population is small is not surprising given the constellation of life course factors that have been found to affect the risk of childhood obesity (Pérez-Escamilla and Kac, 2013).
The biological plausibility for expecting a causal association between breastfeeding and risk of childhood obesity is strong and may be explained by multiple mechanistic pathways, including genomic propensity to become obese. Indeed, recent findings indicate that the benefit of breastfeeding against the risk against childhood obesity may be more pronounced among children who have a genetic propensity to become obese (Abarin et al., 2012; Dedoussis et al., 2011). This genetic effect modification of a breastfeeding benefit (in this instance protection against childhood obesity) is fully consistent with what has been found regarding modification of the benefit of breastfeeding on intellectual development as a function of a fatty acid metabolism genomic modification. Specifically, a genetic variant in the fatty acid desaturase 2 (FADS2) gene has been found to moderate the effect of breastfeeding on improved intellectual development in children (Caspi et al., 2007).
The Promotion of Breastfeeding Intervention Trial (PROBIT) has called into question the findings of observational studies that have documented an association between breastfeeding and reduced childhood obesity risk. PROBIT, a large-scale randomized controlled study conducted in Belarus to test the effect of the Baby Friendly Hospital Initiative (BFHI) on breastfeeding outcomes, failed to document such an association despite showing a major positive effect on breastfeeding outcomes. This has understandably been a strong reason behind questioning findings from observational studies documenting such association.
It is important however to acknowledge that the preponderance of the epidemiological evidence does not support generalizing the PROBIT findings as this trial has major external validity and statistical power limitations. First, the PROBIT trial excluded infants who were never breastfed, thus it lacks an internal reference group of infants who were exclusively formula-fed since birth. Second, PROBIT is severely underpowered to examine the association of interest-based on the relatively small effect size that would need to be detected. Indeed, Beyerlein and Von Kries (2011) have estimated that PROBIT has a statistical power of 4 percent to answer the question of interest, compared with the expected 80 percent.
The findings that have emerged from recent epidemiological evidence, combined with the biological plausibility of a protective effect of breastfeeding throughout the lifecourse, strongly support the development and support of a research agenda to answer questions based on potential effect modification by the presence or absence of risk factors for childhood obesity. Specific questions that should be answered include finding out if the magnitude of the protective effect of breastfeeding on childhood obesity depends on any of the following:
- Genomic propensity to obesity in the child,
- Maternal prepregnancy obesity,
- Excessive weight gain during pregnancy,
- Excessive infant weight gain during infancy,
- Types of beverages and foods fed to infants in lieu or in addition to breast milk,
- Protein content of infant formula,
- Human milk offered from the breast (versus expressed and fed via a bottle or cup), and
- Degree and duration of breastfeeding exclusivity.
Prospective studies that carefully measure exclusive breastfeeding duration, genomic propensities, and the gut microbiome should be the basis for future epidemiological and basic mechanistic research as it is clear that the relationship between breastfeeding and childhood obesity is likely to follow multiple pathways that form a complex web, including epigenetic mechanisms (Geddes and Prescott, 2013; Woo 2015). These studies should be designed with adequate statistical power to test for effect modification by other maternal-child life course factors, including pre-pregnancy BMI, gestational weight gain, and the timing of introduction and the type of complementary feeding (Daniels et al., 2015; Pérez-Escamilla and Bermudez, 2012). These studies also need to carefully assess diet and physical activity between the period of breastfeeding and the time when follow-up anthropometric measurements are taken as these have generally not been corrected in previous prospective studies, which is a major gap that needs to be addressed.
Contrary to what has been argued before (Casazza et al., 2013) there are strong reasons for expecting a causal association between breastfeeding and the prevention of childhood obesity, especially among children with a genomic predisposition to become obese. Given the impracticability of screening for genomic propensity to tailor individual infant feeding recommendations and the large number of additional benefits offered by breastfeeding for maternal–child health (Victora et al., 2016), from a public health perspective it is recommended to continue including breastfeeding as part of comprehensive childhood obesity prevention strategies. These strategies can acknowledge that the level of benefit will be different as a function of genetic factors and epigenetic processes. Thankfully, we have a number of evidence-based strategies that work at both the facility and the community level, and some that work on the macroenvironment, protecting the ability of mothers who wish to breastfeed their babies to do so. These include the Baby Friendly Hospital Initiative (Pérez-Escamilla, 2007; Pérez-Escamilla and Hall Moran, 2016; Pérez-Escamilla et al., 2016), breastfeeding community-based peer counseling (Chapman et al., 2010), and breastfeeding protection policies (Hawkins et al., 2013; Smith-Gagen et al., 2014).
In conclusion, the preponderance of the epidemiological evidence suggests that the effect size of the benefit that breastfeeding may offer against obesity risk in the general population is small, as expected. The biological plausibility for expecting this association to be causal is likely to be strong. The apparent effect modification by genetic predisposition strengthens the causality argument, although much more research is needed to confirm this finding across diverse populations.
Download the graphic below and share it on social media!
References
- Abarin, T., Y. Yan Wu, N. Warrington, S. Lye, C. Pennell, and L. Briollais. 2012. The impact of breastfeeding on FTO-related BMI growth trajectories: An application to the Raine pregnancy cohort study. International Journal of Epidemiology 41(6):1650-1660. https://doi.org/10.1093/ije/dys171
- American Academy of Pediatrics. 2014. AAP Pediatric Nutrition Handbook, 7th ed. Elk Grove Village, IL: AAP.
- American College of Obstetricians and Gynecologists. 2016. Optimizing support for breastfeeding as part of obstetric practice. Committee opinion 658. Available at: http://www.acog.org/Resources-And-Publications/Committee-Opinions/Committee-onObstetric-Practice/Optimizing-Support-for-Breastfeeding-as-Part-of-Obstetric-Practice (accessed June 5, 2016).
- Bartick, M., and A. Reinhold. 2010. The burden of suboptimal breastfeeding in the United States: A pediatric cost analysis. Pediatrics 125(5):e1048-e1056. https://doi.org/10.1542/peds.2009-1616
- Bartick, M. C., A. M. Stuebe, E. B. Schwarz, C. Luongo, A. G. Reinhold, and E. M. Foster. 2013. Cost analysis of maternal disease associated with suboptimal breastfeeding. Obstetrics and Gynecology 122(1):111-119. https://doi.org/10.1097/AOG.0b013e318297a047
- Beyerlein, A., and R. von Kries. 2011. Breastfeeding and body composition in children: Will there ever be conclusive empirical evidence for a protective effect against overweight? American Journal of Clinical Nutrition 94(6 Suppl):1772S-1775S. https://doi.org/10.3945/ajcn.110.000547
- Casazza, K., K. R. Fontaine, A. Astrup, L. L. Birch, A. W. Brown, M. M. Bohan Brown, N. Durant, G. Dutton, E. M. Foster, S. B. Heymsfield, K. McIver, T. Mehta, N. Menachemi, P. K. Newby, R. Pate, B. J. Rolls, B. Sen, D. L. Smith Jr, D. M. Thomas, and D. B. Allison. 2013. Myths, presumptions, and facts about obesity. The New England Journal of Medicine 368(5):446-454. https://doi.org/10.1056/NEJMsa1208051
- Caspi, A., B. Williams, J. Kim-Cohen, I. W. Craig, B. J. Milne, R. Poulton, L. C. Schalkwyk, A. Taylor, H. Werts, and T. E. Moffitt. 2007. Moderation of breastfeeding effects on the IQ by genetic variation in fatty acid metabolism. Proceedings of the National Academy of Sciences 104(47):18860-18865. https://doi.org/10.1073/pnas.0704292104
- Chapman, D. J., K. Morel, A. K. Anderson, G. Damio, and R. Pérez-Escamilla. 2010. Breastfeeding peer counseling: From efficacy through scale-up. Journal of Human Lactation 26(3):314-326. https://doi.org/10.1177/0890334410369481
- Daniels, L., M. K. M. Mallan, A. Fildes, and J. Wilson. 2015. The timing of solid introduction in an ‘obesogenic’ environment: A narrative review of the evidence and methodological issues. Australian New Zealand Journal of Public Health 39:366-373. https://doi.org/10.1111/1753-6405.12376
- Dedoussis, G. V., M. Yannakoulia, N. J. Timpson, Y. Manios, S. Kanoni, R. A. Scott, C. Papoutsakis, P. Deloukas, Y. P. Pitsiladis, G. Davey-Smith, J. N. Hirschhorn, and H. N. Lyon. 2011. Does a short breastfeeding period protect from FTO-induced adiposity in children? International Journal of Pediatric Obesity 6(2-2):e326-e335. https://doi.org/10.3109/17477166.2010.490269
- Dewey, K. G. 1998. Cross-cultural patterns of growth and nutritional status of breast-fed infants. American Journal of Clinical Nutrition 67(1):10-17. https://doi.org/10.1093/ajcn/67.1.10
- Dewey, K. G. 2003. Is breastfeeding protective against child obesity? Journal of Human Lactation 19(1):9-18. https://doi.org/10.1177/0890334402239730
- Geddes, D. T., and S. L. Prescott. 2013. Developmental origins of health and disease: The role of human milk in preventing disease in the 21(st) century. Journal of Human Lactation 2:123-127. https://doi.org/10.1177/0890334412474371
- Giugliani, E. R., B. L. Horta, C. L. de Mola, B. O. Lisboa, and C. G. Victora. 2015. Effect of breastfeeding promotion interventions on child growth: A systematic review and metaanalyses. Acta Paediatrica 104(467):20-29. https://doi.org/10.1111/apa.13160
- Hawkins, S. S., A. D. Stern, and M. W. Gillman. 2013. Do state breastfeeding laws in the USA promote breast feeding? Journal of Epidemiology and Community Health 67(3):250-256. https://doi.org/10.1136/jech-2012-201619
- Horta, B. L., C. L. de Mola, and C. G. Victora. 2015. Long-term consequences of breastfeeding on cholesterol, obesity, systolic blood pressure, and type-2 diabetes: Systematic review and meta-analysis. Acta Paediatrica 104(467):30-37. https://doi.org/10.1111/apa.13133
- Koletzko, B., R. von Kries, R. C. Monasterolo, J. E. Subías, S. Scaglioni, M. Giovannini, J. Beyer, H. Demmelmair, B. Anton, D. Gruszfeld, A. Dobrzanska, A. Sengier, J. P. Langhendries, M. F. Cachera, V. Grote, and the European Childhood Obesity Trial Study Group. 2009. Infant feeding and later obesity risk. Advances in Experimental Medicine and Biology 646:15-29. https://doi.org/10.1007/978-1-4020-9173-5_2
- Li, R., K. S. Scanlon, A. May, C. Rose, and L. Birch. 2014. Bottle-feeding practices during early infancy and eating behaviors at 6 years of age. Pediatrics 134(Suppl 1):S70-S77. https://doi.org/10.1542/peds.2014-0646L
- Luque, V., R. Closa-Monasterolo, J. Escribano, and N. Ferré. 2016. Early programming by protein intake: The effect of protein on adiposity development and the growth and functionality of vital organs. Nutritional and Metabolism Insights 8(Suppl 1):49-56. https://doi.org/10.4137/NMI.S29525
- Mennella, J. A. 2014. Ontogeny of taste preferences: Basic biology and implications for health. American Journal of Clinical Nutrition 99(3):704S-711S. https://doi.org/10.3945/ajcn.113.067694
- Pérez-Escamilla, R. 2007. Evidence based breast-feeding promotion: The Baby-Friendly Hospital Initiative. Journal of Nutrition 137(2):484-487. https://doi.org/10.1093/jn/137.2.484
- Pérez-Escamilla, R., and O. Bermúdez. 2012. Early life nutrition disparities: Where the problem begins? Advances in Nutrition 3(1):71-72. https://doi.org/10.3945/an.111.001453
- Pérez-Escamilla, R., and V. Hall Moran. 2016. Scaling up breastfeeding programmes in a complex adaptive world. Maternal and Child Nutrition. https://doi.org/10.1111/mcn.12335
- Pérez-Escamilla, R., and G. Kac. 2013. Childhood obesity prevention: A life-course framework. International Journal of Obesity Supplement 3(Suppl 1):S3-S5. https://doi.org/10.1038/ijosup.2013.2
- Pérez-Escamilla, R., R. J. Cohen, K. H. Brown, L. L. Rivera, J. Canahuati, and K. G. Dewey. 1995. Maternal anthropometric status and lactation performance in a low-income Honduran population: Evidence for the role of infants. American Journal of Clinical Nutrition 61(3):528-534. https://doi.org/10.1093/ajcn/61.3.528
- Pérez-Escamilla, R., J. E. Obbagy, J. M. Altman, E. V. Essery, M. M. McGrane, Y. P. Wong, J. M. Spahn, and C. L. Williams. 2012. Dietary energy density and body weight in adults and children: A systematic review. Journal of Academic Nutrition and Diet 112(5):671-684. https://doi.org/10.1016/j.jand.2012.01.020
- Pérez-Escamilla, R., J. L. Martinez, and S. Segura-Pérez. 2016. Impact of the Baby-Friendly Hospital Initiative on breastfeeding and child health outcomes: A systematic review. Maternal and Child Nutrition 2016;12(3):375-80. https://doi.org/10.1111/mcn.12294
- Smith-Gagen, J., R. Hollen, S. Tashiro, D. M. Cook, and W. Yang. 2014. The association of state law to breastfeeding practices in the US. Maternal and Child Health Journal 18(9):2034-2043. https://doi.org/10.1007/s10995-014-1449-4
- Victora, C. G., R. Bahl, A. J. Barros, G. V. França, S. Horton, J. Krasevec, S. Murch, M. J. Sankar, N. Walker, N. C. Rollins, and Lancet Breastfeeding Series Group. 2016. Breastfeeding in the 21st century: Epidemiology, mechanisms, and lifelong effect. Lancet 387(10017):475-490. https://doi.org/10.1016/S0140-6736(15)01024-7
- Weber, M., V. Grote, R. Closa-Monasterolo, J. Escribano, J. P. Langhendries, E. Dain, M. Giovannini, E. Verduci, D. Gruszfeld, P. Socha, B. Koletzko, and European Childhood Obesity Trial Study Group. 2014. Lower protein content in infant formula reduces BMI and obesity risk at school age: Follow-up of a randomized trial. American Journal of Clinical Nutrition 99(5):1041-1051. https://doi.org/10.3945/ajcn.113.064071
- Weng, S. F., S. A. Redsell, J. A. Swift, M. Yang, and C. P. Glazebrook. 2012. Systematic review and meta-analyses of risk factors for childhood overweight identifiable during infancy. Archives of Disease in Childhood 97:1,019-1,026. https://doi.org/10.1136/archdischild-2012-302263
- Woo, J. G., and L. J. Martin. 2015. Does breastfeeding protect against childhood obesity? Moving beyond observational evidence. Current Obesity Reports 4(2):207-216. https://doi.org/10.1007/s13679-015-0148-9
- Woo Baidal, J. A, L. M. Locks, E. R. Cheng, T. L. Blake-Lamb, M. E. Perkins, and E. M. Taveras. 2016. Risk factors for childhood obesity in the first 1,000 days: A systematic review. American Journal of Preventive Medicine 50(6):761-779. https://doi.org/10.1016/j.amepre.2015.11.012
- Wood, C. T., A. C. Skinner, H. S. Yin, R. L. Rothman, L. M. Sanders, A. Delamater, S. N. Ravanbakht, and E. M. Perrin. 2016. Association between bottle size and formula intake in 2-month-old infants. Academic Pediatrics 16(3):254-259. https://doi.org/10.1016/j.acap.2015.08.001