Burnout and Job and Career Satisfaction in the Physician Assistant Profession: A Review of the Literature
ABSTRACT | While much is known about the prevalence of burnout among physicians and nurses, little is known about burnout in the physician assistant (PA) profession. Approximately 50 percent of physicians and 35 percent of nurses report symptoms of burnout. Burnout is linked to increased health care costs, medical errors, and poor patient outcomes. The PA profession emerged in the 1960s in response to workforce shortages in rural and underserved communities. The profession has evolved from one designed for primary care to one that is adaptable to broad workforce demands. PAs are now employed in almost all medical specialties, including those with physicians reporting high rates of burnout. The authors believe that this is the first paper to explore the literature that relates specifically to PA burnout and career and job satisfaction.
Introduction
Burnout in health care providers, first described in 1974, is generally defined by emotional exhaustion, depersonalization, and a low sense of personal accomplishment [1,2,3]. Burnout is prevalent among many health care professionals, including doctors, nurses, dentists, pharmacists, and physician assistants (PAs) [2]. Contributing factors to the prevalence of burnout include the strain on the US health care system caused by increased demand for health services, due to expanded health care access; increased workloads; and the administrative burden resulting from the implementation of electronic health records [3,4,5,6]. Symptoms of clinician burnout are associated with risks to safe, high-quality, and efficient health care [6,7,8]. In 2014, 54 percent of sampled physicians reported at least one symptom of burnout, and in 2011, 35 percent of sampled nurses reported symptoms of burnout [3,5,9]. Rates of burnout among dentists, pharmacists, and other health care professionals have not been rigorously studied but are assumed, through anecdotal data, to be at least comparable to the rates for physicians and nurses.
The short duration of training and specialty flexibility inherent to the PA profession add to its attractiveness as a profession. Still, small studies suggest that rates of burnout among PAs may be similar to rates among physicians, between 34 percent and 64 percent [10,11]. Although burnout can have a negative impact on job and career satisfaction [12], the available literature suggests that PAs maintain very high levels of job and career satisfaction [11]. However, few studies to date have focused exclusively on PA burnout and career and job satisfaction.
Background
The PA profession was created in the mid-1960s to address health care workforce shortages and the poor distribution of physicians across the United States. Architects of the new profession envisioned a process in which former military service corps personnel were trained to work closely with physicians to provide cost-effective primary medical care in communities experiencing physician shortages [11,13,14]. PAs are trained in the primary care medical model and work collaboratively in physician-PA teams [15]. The average PA education program length is 26 months. The first year includes didactic education in basic medical sciences and clinical medicine, followed by a second year of clinical rotations in family medicine, internal medicine, psychiatry, emergency medicine, general surgery, obstetrics and gynecology, and pediatrics. Rotations may be completed in a variety of settings, including outpatient and ambulatory clinics, inpatient and acute settings, and within rural and urban underserved communities [15]. Following successful completion of PA training at an accredited program, graduates are eligible to complete the Physician Assistant National Certifying Examination, administered by the National Commission on Certification of Physician Assistants (NCCPA), in order to apply for state licensure [15]. Originally created as a “doctor’s assistant” role with a narrow scope of practice, the profession has, over time, gained legal practice and prescribing authority in all 50 states.
In response to generational changes, economic demands, and shifts in societal norms and gender roles, the PA profession has undergone four major trends over the last three decades [16]: growth in the workforce, increased proportion of women in the profession, decline in the age of entry into the career, and movement toward specialty practice.
The first three PAs graduated from Duke University in 1967, and the PA profession now graduates approximately 8,000 students annually from 236 accredited programs [17,18]. There were over 123,000 PAs in the workforce in 2017 [19,20]. PAs currently comprise approximately 10 percent of the combined physician assistant/nurse practitioner (NP)/PA workforce [20,21,22]. In its 2018 “Statistical Profile on Certified Physician Assistants,” the NCCPA reports that the majority (20 percent) of certified PAs practice in family and general medicine, followed by emergency medicine (13 percent), and orthopedic surgery (11 percent) [20]. PAs report working a median 40 hours per week and having a median annual salary of $105,000 [20]. The majority (65 percent) do not have on-call responsibilities [20].
Reflecting the increase in women in higher education and in the workforce [16], the percentage of women in the PA profession has also steadily increased, from 31 percent in 1981 [23], to 68 percent of the workforce in 2018 [20]. Similarly, the age of entry has decreased over the past 20 years. In 1984, 43 percent of first-year students were older than 27 years at age of entry, compared to 39 percent in 2005 [24,25]. This may also reflect the shifting demographics of the profession from veterans to a new workforce of health professionals [16].
PAs are unique among health care providers in that they can, and often do, change specialties during their careers. Half of PAs change specialties at least once during the course of their career; 8.3 percent changed their specialties in 2014 [26,27]. Specialty mobility is an appealing feature of the profession, as it eliminates the pressure for PAs to choose a lifelong specialty in their early career and provides the opportunity to react to workforce demand trends and lifestyle changes. Based on an analysis of national census data, Hooker, Cawley, and Leinweber suggest that higher salaries in medical specialties and the increasing number of job opportunities in medicine may drive career mobility in the PA profession [26].
Surveys of newly matriculating PA students show that they choose the profession for a variety of reasons, including a shorter training time than is required for physician education, resulting in less student debt at graduation [28]. Data on debt load have been discussed elsewhere. In family medicine, the median debt load for female PAs is $100,000, compared to $175,000 for female physicians [29]. PA students also frequently cite the opportunity for specialty mobility throughout their careers and the expectation of a healthy work-life balance [30].
The PA profession is aligned with the principles of the Triple Aim to improve and optimize the US health care system. The profession was created to increase access to care, reduce the total cost of care, and improve the health of the population [31]. A subsequent fourth aim, “joy in work,” addresses the growing incidence and prevalence of burnout among clinicians in health care [7]. While PA contributions to team-based care may help promote work-related well-being among health care providers, relatively little is known about PA burnout and work-life experience. Dyrbye and colleagues have provided a summary of available, reliable measurement tools to assess burnout and career and job satisfaction [32].
Literature Search
Methods
A systematic review, conducted in 2017, of articles published between 2000 and 2016 on PA and NP work-related psychological states (e.g., job satisfaction, burnout, turnover) assessed nine articles involving analyses of PAs [4]. To identify additional and more recent literature for this review, a health sciences librarian was consulted to devise a replicable search strategy, which was undertaken on August 10, 2018, in PubMed (Medline), CINAHL, and PsychINFO. Search strings included the MeSH term (PubMed) and Exact Major Subject Heading (CINAHL and PsychINFO) “physician assistants” and variations for the term “physician assistant” (e.g., “physician’s assistant,” “advanced practice provider”). These terms were combined with multiple terms that reflect work-related experiences. Experience-related terms included those used in the 2017 review (i.e., “job satisfaction,” “career satisfaction,” “work satisfaction,” “burnout,” “turnover,” “intent to stay,” “intent to leave,” and “stress”), as well as “resilience,” “retention,” and “well-being.”
To maintain focus on articles reflective of the current clinical environment for PAs, the search was limited to articles published in English in 2000 or later. The original search of the three databases yielded 246 articles. Articles selected for review were limited to clinically practicing PAs, and they described original research related to work-life experiences in the United States. After excluding duplicates, 20 relevant research articles, including 13 not assessed in the 2017 review, were identified. To ensure that all relevant articles were detected, the reference lists of the initial 20 selected articles were reviewed, and with the support of the health sciences librarian, five additional searches were constructed in PubMed using combinations of terms designed to identify articles that may have been missed, e.g., “‘clinician’ AND ‘burnout’ AND ‘intervention.’” This strategy yielded 231 articles and, after exclusion of duplicates, resulted in 16 additional relevant articles. After the initial searches were conducted, one additional relevant article published in September 2018 was identified. The search yielded 37 articles.
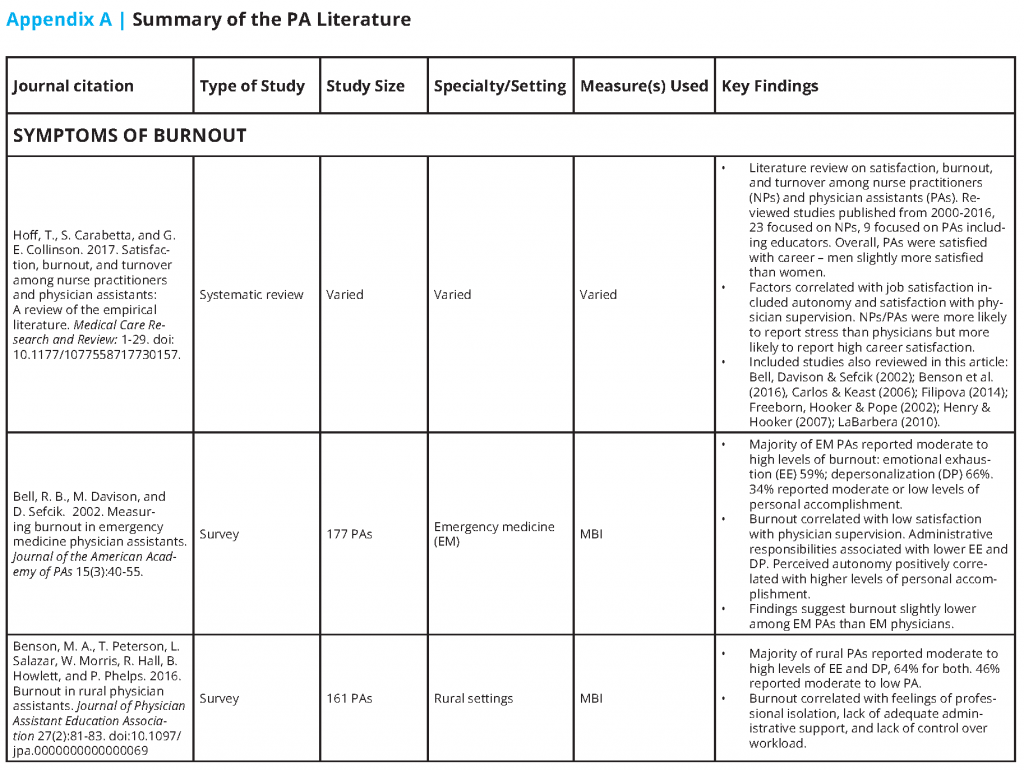
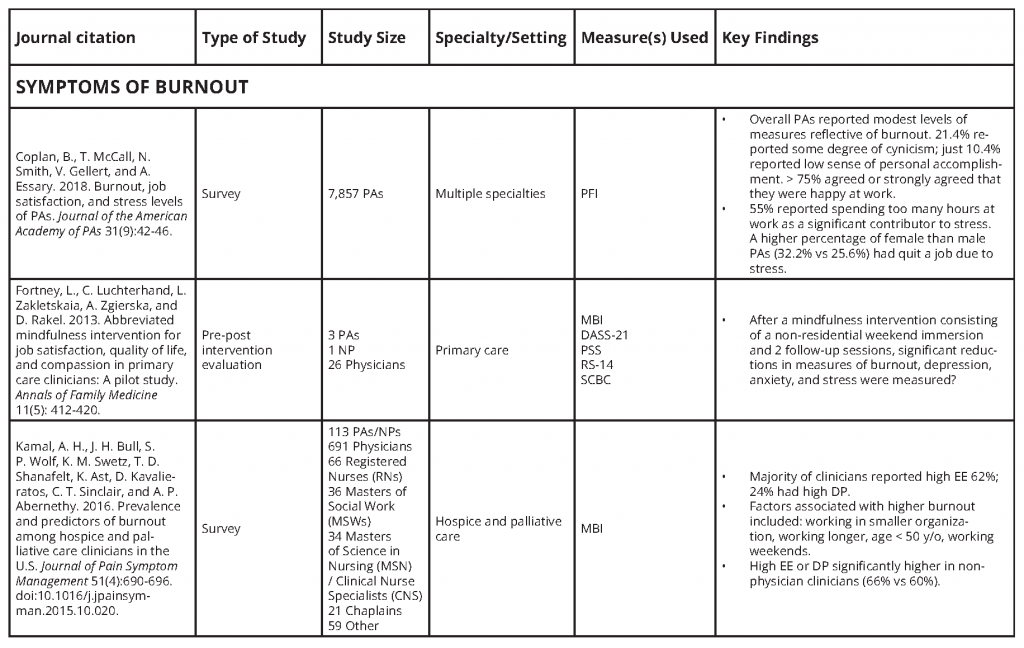
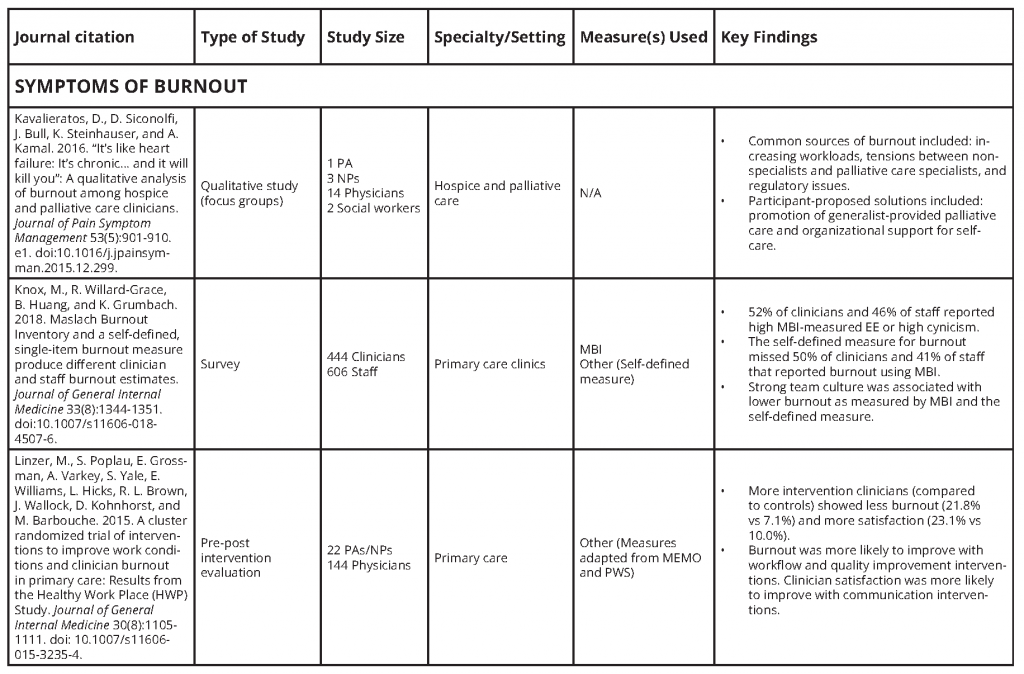
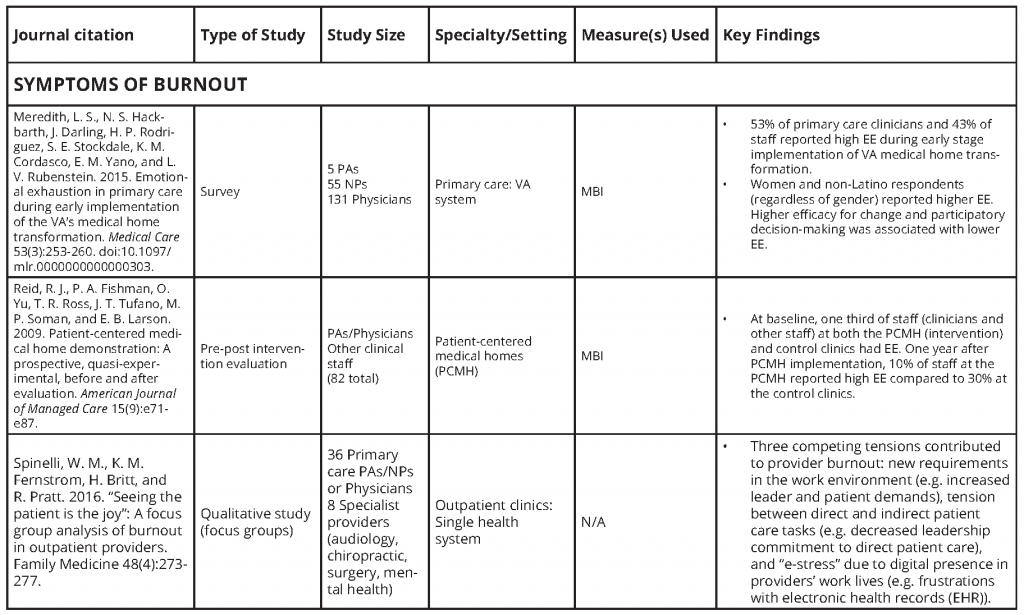
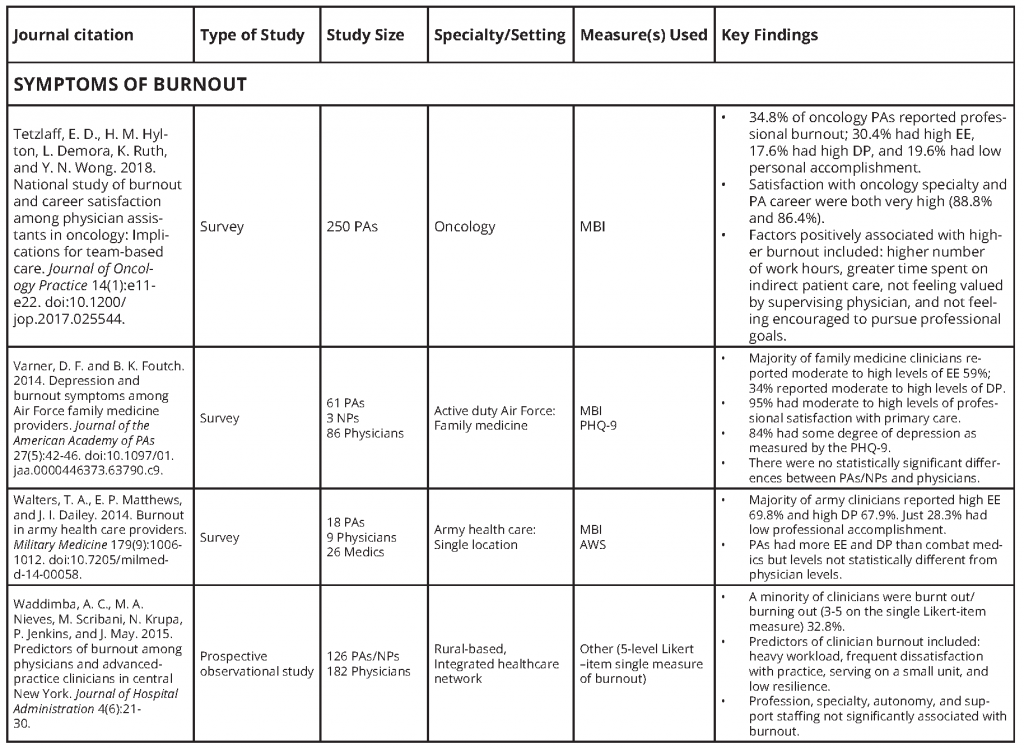
Of those articles, 13 focused exclusively on PAs; of these, four evaluated PAs in rural settings (see Appendix A). Among all studies described in the articles, 10 focused on primary care settings, two on emergency medicine, and two on hospice and palliative care. Other specialties studied included oncology, radiology, orthopedics, and cardiovascular surgery. The majority of research was descriptive in nature; however, three articles on primary care clinicians (including physicians, Pas, and NPs) assessed interventions for burnout or job satisfaction. One examined the impact of practice transition to a patient-centered medical home (PCMH) [33]. The aspects of work-life experience that were examined varied considerably across the various articles. While 18 articles included burnout as a main focus, more than half focused on other aspects of work-life balance, including career and/or job satisfaction. Across those 18 articles, a variety of instruments were used to measure work-life experience. Twelve of these 18 articles that assessed burnout used a version of the Maslach Burnout Inventory (MBI), making it the most commonly used measurement instrument.
The literature review below is organized by 1) symptoms of burnout, and “burnout” is defined as emotional exhaustion (EE), depersonalization (DP), and a reduced sense of personal accomplishment; and 2) “career satisfaction” and “job satisfaction,” defined respectively as satisfaction with career choice and satisfaction with the expectation of one’s job and the reward it provides (e.g., working conditions, supervision, benefits, job security). When referring to physicians, NPs, and PAs collectively, the term “clinician” is used.
Burnout
The literature focused on PA burnout is primarily limited to rural and specialty settings. However, one national survey that assessed work-life experiences—including burnout, happiness, and work-related stress—consisted of responses from 7,857 PAs from multiple specialties and locations [34]. Results of this national survey revealed that 21.4 percent of PAs felt some degree of cynicism, and 10.4 percent reported experiencing a low sense of personal accomplishment. Compared to male PAs, a higher percentage of female PAs had quit a job due to stress (25.6 percent versus 32.2 percent). Overall, more than 75 percent of PAs surveyed reported feeling happy at work [34].
In a study of rural PAs, Benson and colleagues found that 64 percent of PAs experienced moderate to high levels of both EE and DP, as measured by MBI subscores; 46 percent reported low to moderate scores for personal accomplishment [10]. Bell, Davison, and Sefcik found similar rates of moderate or high EE (59 percent) and DP (66 percent) among emergency medicine PAs [36]. Those who reported symptoms of burnout were more likely to report planning to leave emergency medicine within one year. Respondents who self-identified as female were more likely to report symptoms of burnout. Reports of symptoms of burnout were also positively associated with reports of dissatisfaction with supervising physicians (SPs), insomnia, and regular alcohol and tobacco use [35]. Research on PAs in oncology revealed that 35 percent experienced at least one symptom of burnout as measured by the MBI. Positively associated factors included not feeling valued by their SPs, not feeling encouraged professionally, and not receiving recognition for their contributions [36]. Despite the prevalence of burnout, however, most oncology PAs reported very high levels of job and career satisfaction (89 percent and 86 percent respectively) [36].
Kamal et al. and Kavalieratos et al. evaluated burnout among clinicians in hospice and palliative care [37,38]. Kamal et al. found that 66 percent of nonphysician clinicians (NPs, PAs, nurses, social workers, and chaplains) experienced at least one symptom of burnout as measured by the MBI, compared to 60 percent of physicians [37]. Kamal et al. also noted a correlation between higher reported symptoms of burnout and PAs who were over 50 years old [37]. Kavalieratos et al. conducted focus groups of hospice and palliative care clinicians to identify common sources of, and solutions for, burnout [38]. Both articles noted the positive influence of team-based, collaborative relationships on professional attitudes and perspectives [37,38]. A focus group study by Spinelli and colleagues echoed these findings, citing barriers to teamwork and lack of recognition for work done as factors that contributed to burnout among primary care clinicians [39].
Clinicians in the military serve in unique and stressful environments and experience higher rates of burnout than civilian providers [11,40]. Walters, Matthews, and Dailey found a positive correlation between self-reported measures of EE and DP and accrued leave days (e.g., not taking time off) among active duty army clinicians [40]. Varner and Foutch found medium to high levels of burnout among air force family medicine clinicians (59 percent EE, 34 percent DP), while 95 percent reported medium to high levels of professional satisfaction. Interestingly, older age (being over 44 years) was associated with lower burnout levels [11].
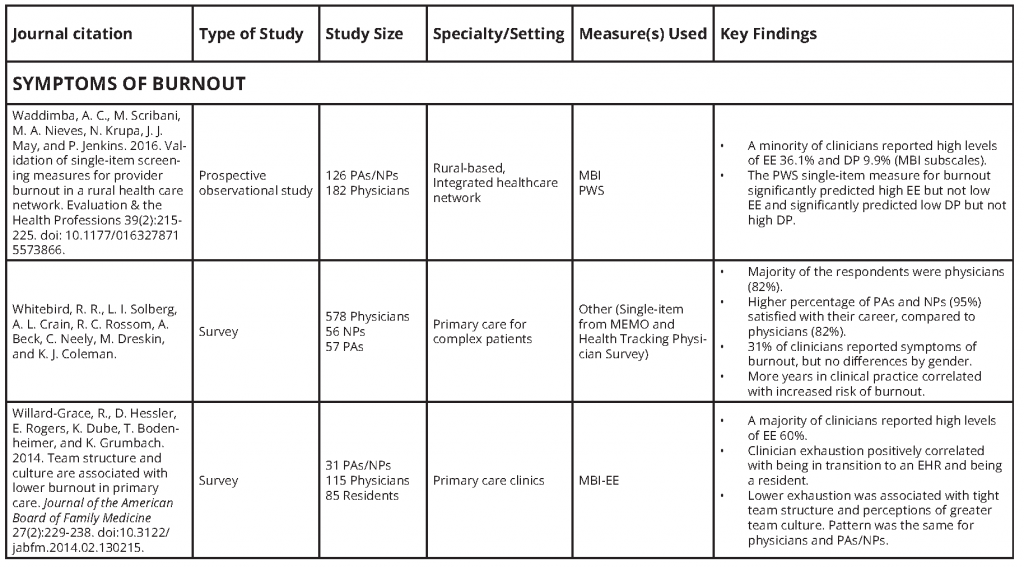
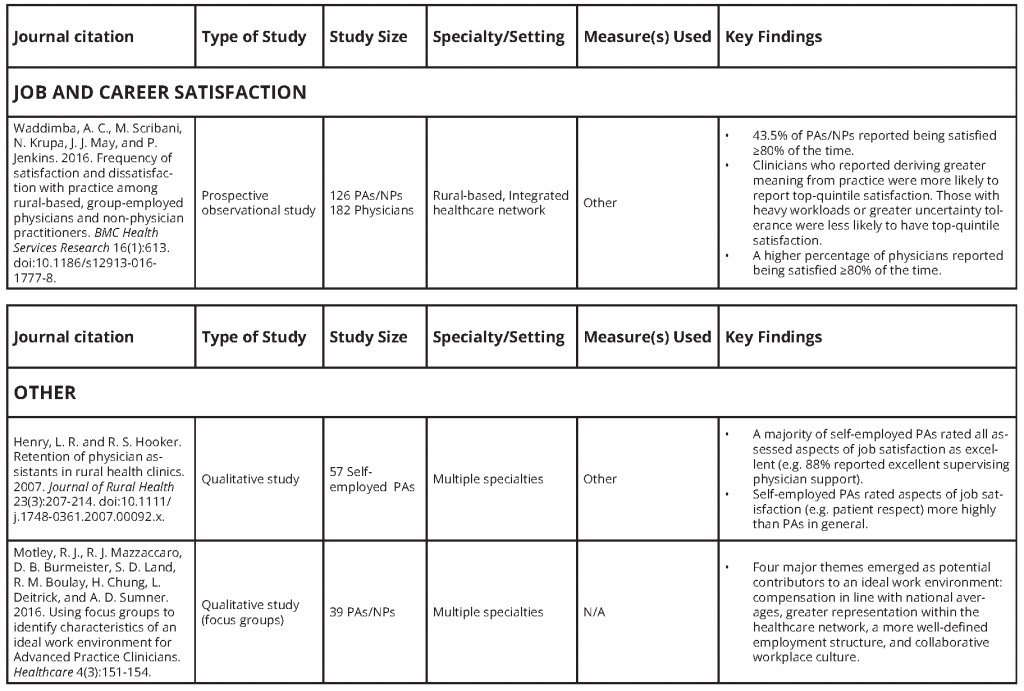
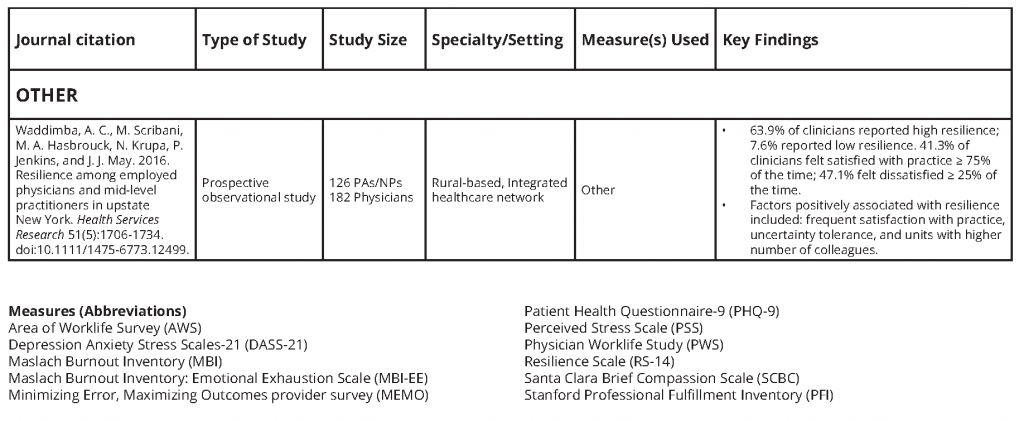
Whitebird et al. evaluated burnout and career satisfaction among primary care clinicians across multiple states [12]. Thirty-one percent reported symptoms of burnout using the single-item Physician Work Life Study (PWS) measure. Burnout positively correlated with number of years in practice and negatively correlated with career satisfaction and comfort in managing complex medical conditions. PAs and NPs experienced higher rates of career satisfaction (95 percent) compared to physicians (82 percent). In addition, lower career satisfaction was associated with insufficient resources for managing patients with complex clinical conditions [12]. Using cross-sectional data from the Practitioner Resilience, Adaptability and Wellbeing Study [41], Waddimba and colleagues evaluated burnout among rural clinicians in an integrated health care system in New York. Similar to Whitebird et al., researchers found that nearly a third of clinicians reported symptoms of burnout using the single-item PWS measure. Risk factors for burnout included employment in smaller clinics, lower tolerance of stress, more frequent dissatisfaction with practice, and unmet relationship needs [41].
Linzer and colleagues also used the PWS to evaluate clinician burnout in primary care settings. In their study, involving various interventions designed to improve work conditions, burnout was more likely to improve with workflow and quality improvement interventions, whereas clinician satisfaction was more likely to improve with communication interventions [42]. In a study of clinician burnout pre- and post-implementation of PCMHs in clinics at a large, nonprofit integrated health system, Reid et al. found that PAs and physicians had similar rates of high EE at baseline [33]. After implementation, EE improved significantly among PAs and physicians in PCMHs; just 14.2 percent reported high EE, compared to 35.2 percent of clinicians in clinics that did not implement a PCMH. The authors felt this finding may be attributable to more supportive and collaborative work environments in PCMHs. Meredith et al. evaluated burnout among primary care clinicians during PCMH transformation in facilities run by the Department of Veterans Affairs and found that 53 percent of clinicians were experiencing high EE during the early phases of transformation [43]. Factors associated with lower EE included higher efficacy for change and engaging in participatory decision making.
Career and Job Satisfaction
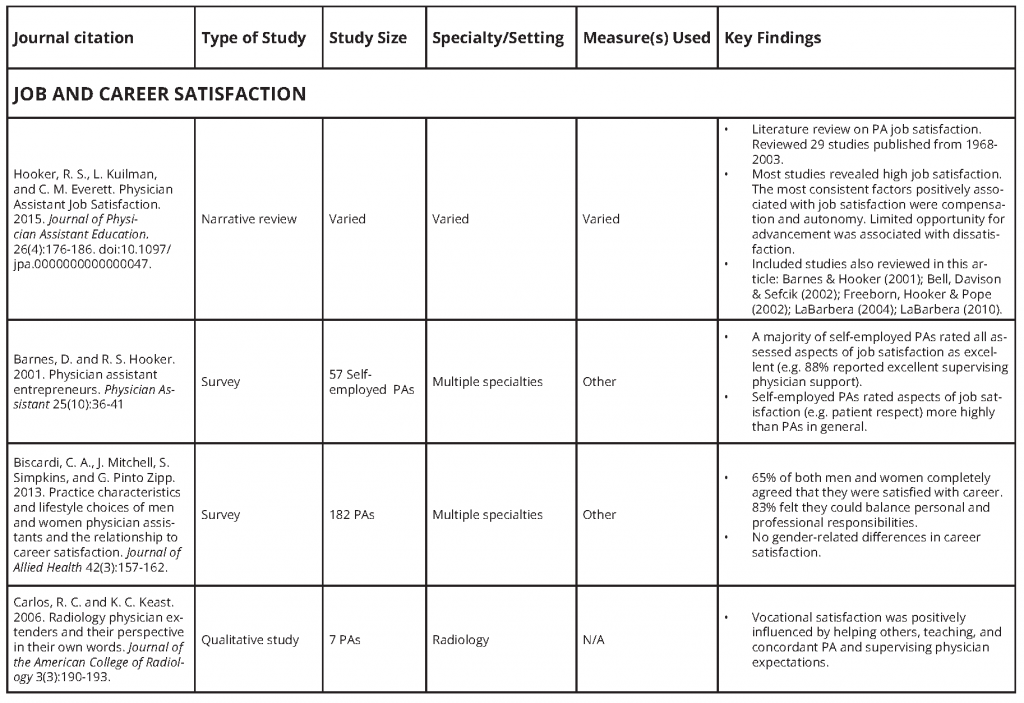
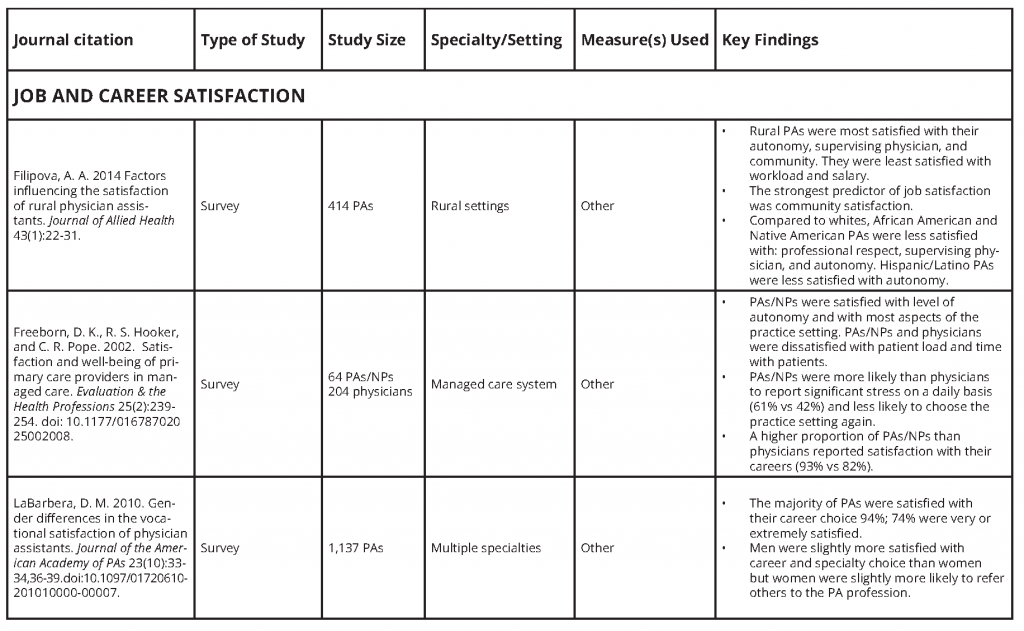
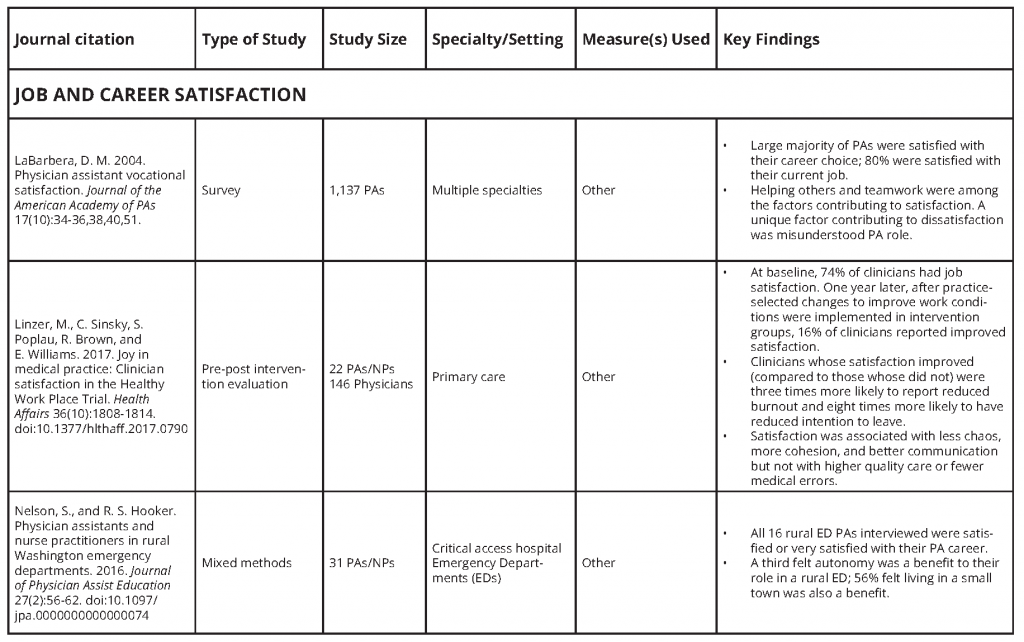
LaBarbera conducted a national survey of PAs in 2003 (N=1,137) that revealed a large majority were satisfied with their career choices as well as their current jobs (92 percent and 82 percent respectively) [44]. Although men were slightly more satisfied with their careers and specialty choices than women, women were more likely to refer others to the PA profession [45]. Helping others and teamwork were among the factors that PAs felt contributed to their satisfaction, whereas general misunderstanding of the PA role (role ambiguity) resulted in dissatisfaction. In a smaller 2013 study involving a random national sample of PAs (N=182), Biscardi and colleagues found that male and female PAs were equally satisfied with their careers; 64 percent completely agreed they were satisfied with their PA careers and 80 percent felt that they were able to balance their personal and professional lives [46].
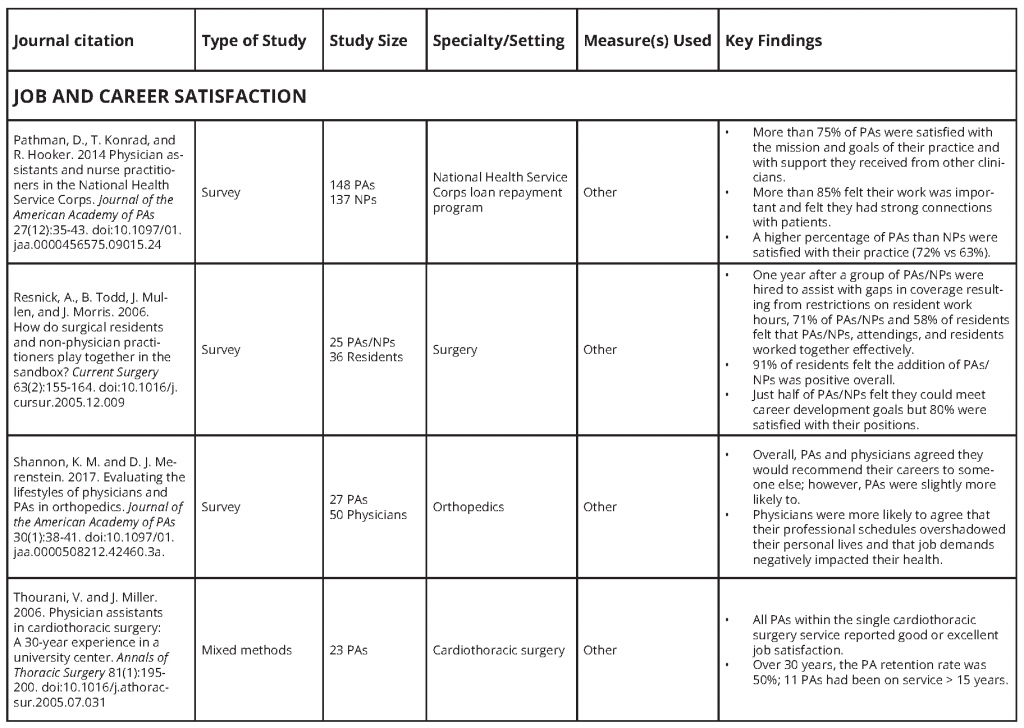
Small studies of PAs in rural settings support these findings. Nelson and Hooker completed a mixed methods evaluation of 31 PAs and NPs working in rural Washington emergency departments and found that all 16 PAs were either “satisfied” or “very satisfied” with the PA career [47]. Similarly, Pathman, Konrad, and Hooker found high levels of job satisfaction (74 percent) among PAs in the National Health Service Corps (NHSC) [48]. Of note, 93 percent felt they were doing important work in their practice, and less than a third reported that work encroached on personal time [48]. Henry and Hooker conducted an in-depth qualitative analysis of eight PAs working in rural clinics in Texas to assess factors associated with retention in remote areas [49]. They found that retention (considered a proxy for satisfaction) was closely linked to confidence in clinical abilities and community embeddedness [49]. Filipova’s investigation of satisfaction among 414 rural PAs supports these findings. Among factors associated with overall job satisfaction, which included autonomy and satisfaction with one’s supervising physician, satisfaction with the community was the most significant predictor [50].
In studies that compared PAs to other clinicians, PAs generally reported more favorable attitudes toward their profession. Like Whitebird et al., Freeborn, Hooker, and Pope, in their study of primary care clinicians, found that a higher proportion of PAs and NPs were satisfied with their careers, compared to physicians (93 percent versus 82 percent) [12,51]. Waddimba’s study of rural clinicians demonstrated that being a PA or NP had a modest positive association with job satisfaction [52]. Among the NHSC PAs and NPs that Pathman, Konrad, and Hooker surveyed, a higher proportion of PAs than NPs were satisfied with their practice (72 percent versus 63 percent) [48]. Finally, Shannon and Merenstein examined physicians and PAs in orthopedics and found that PAs were more likely to recommend their profession to others [53].
Factors Unique to the PA Profession
Scope of Practice, Team Dynamics, and Career Flexibility
Several occupational factors unique to the PA profession likely contribute to career and job satisfaction, and to symptoms of burnout. PAs are trained in the context of a broad primary care curriculum but, as noted above, are granted the flexibility by state PA practice laws to move between specialties without additional training or certification [15]. The relative youth of the PA profession and limited emphasis on research as a component of PA education necessitate further evaluation of the potential influence of career mobility on career and job satisfaction and burnout.
The PA’s scope of practice is primarily determined by the supervising physician’s scope of practice, state law, and the needs of the community [15]. Also tied to the PA’s scope of practice is the physician’s understanding of, and confidence in, the PA’s capabilities [15]. Supervisory [38] and leadership skills [8,36,53-58] have been correlated with decreased symptoms of burnout and increased job satisfaction in PAs and physicians. Engaging PAs in work-related decisions and finding value in their full range of clinical contributions has been correlated with increased job satisfaction [4,57], decreased symptoms of burnout [36], and lower attrition [7,56,59,60]. The influence of scope of practice, team-based dynamics, and career flexibility on symptoms of burnout and career and job satisfaction warrants further evaluation.
Practice Setting and Burnout among PAs
According to the National Commission on Certification of Physician Assistants, in 2017, 26.7 percent of certified PAs practiced in primary care settings, including family medicine and general practice, general internal medicine, and general pediatrics [20]. Research focused specifically on PA burnout [10,11] and literature on clinician burnout in general [9,55] reveal high levels of burnout among primary care clinicians. As PA practice has become increasingly specialized, PAs have entered high burnout fields such as emergency medicine (where 59 percent of PAs reported symptoms of EE [20,35]) and oncology (where 30 percent of PAs reported symptoms of EE [20,36]). In both settings, higher reported symptoms of burnout correlated with low satisfaction with physician supervision. Additionally, in fields where physician shortages are expected—such as primary care, orthopedics, and oncology—PAs are increasingly viewed as part of the health care workforce solution and may become even more susceptible to burnout over time [36,53,54]. In 2017, 10.8 percent of PAs worked in orthopedics, and oncology was the third most common internal medicine subspecialty in which PAs practiced [20].
Potential Protective Factors
It is worth noting certain aspects of the PA profession may serve to protect against burnout. First, PAs are trained to practice medicine as part of a health care team, and such team-based practice has been shown to cultivate an environment that reduces symptoms of burnout in primary care [61,62,63]. In addition to demonstrating the positive impact of a strong team culture, a study of primary care clinicians revealed that those working on a team in which they were regularly paired with the same medical assistant experienced less emotional exhaustion than non-team-based clinicians [62]. Teaching may also serve as a protective measure for clinically practicing PAs. Emergency medicine PAs whose professional responsibilities included teaching reported fewer symptoms of burnout than those whose duties did not include such an element [35]. Finally, the PA’s expanding role in health care may serve to invigorate and motivate, thus serving to counteract burnout [4]. All of these protective factors can potentially serve as resources that may buffer against occupational challenges unique to PAs and the development of professional burnout.
PA Faculty and the Academic Environment
Forister and Blessing found statistically significant lower mean levels of burnout for PA faculty compared to their medical education counterparts [64]. Smaller studies support reportings of high levels of job satisfaction [65,66] and low intent to leave [67] among PA faculty. Increased age of PA faculty positively correlates with job satisfaction [66] and inversely correlates with intent to leave academia [67]. Although teaching is identified as a protective factor among emergency medicine PAs [35], a close examination of national data suggests that new research is required to evaluate the state of burnout and job satisfaction among PA faculty. While most faculty identify work-life balance as the primary reason for entering academia [68], national survey data reveal that 44 percent have considered leaving academia for another position, and only 58 percent would again select the same career path [68], leading to concerns about retention of a skilled academic workforce. Further, 14 percent of PA faculty reported working clinically outside of their academic position (reported as “on own time”), with the two most common specialties identified as family and general medicine (29 percent) and emergency medicine (18 percent)[68]. Fifty-three percent of PA programs reported attrition of at least one faculty member in the 2016-17 academic year [17].
Gaps in Research
More research using consistent, rigorous methodology is needed to investigate PA work-life experiences and their impact on the health care delivery system and patient care. Specifically, the authors identify the following high-priority research areas:
- Length of training and burnout. Evaluate the length of training on burnout in the profession, including the influence of debt and work-life balance permitted by the profession [16]. Though the scant literature is mixed regarding age [11,37] versus years in practice [12] as risk factors for symptoms of burnout, time in practice may predispose PAs to burnout, given the relatively young age of entry into clinical practice compared to other clinicians.
- Career flexibility and burnout. Although economic (salaries) and market demands (job opportunities) appear to be the primary drivers of career mobility in the profession, the fact that PAs can change work settings may provide relief from aspects of burnout by enabling a transition to new environments and bolstering career satisfaction. The option to change specialties may partially explain high PA career satisfaction, even when job satisfaction is low or burnout is high, a phenomenon observed among oncology PAs [36]. How these characteristics interface with principles of team-based care may warrant further evaluation.
- Practice setting and its effect on burnout. While PAs can change specialties, Hooker, Cawley, and Leinweber found that half of all PAs remained in their first specialty throughout their careers [26]. This finding requires additional research, given that there may be an increased risk of burnout among clinicians in rural areas [10] and primary care settings [11,12,40,42,61]. The positive (engagement) and negative (burnout) influences on PA employment in specialties and practice settings may assist with PA recruitment and retention efforts in areas with clinician shortages.
- Team culture and burnout. Team-based practice is foundational to the PA profession and is a core component of contemporary health care delivery. The culture of the PA profession, or the “hidden curriculum” of PA training, places an emphasis on teamwork and collaboration [15]. Teamwork, or “team culture,” is associated with job and career satisfaction [42,44] and lower reported symptoms of burnout [61,62]. Further evaluation of team culture in organizations and in the physician-PA team, using validated instruments and rigorous methodology, would serve both professions in advancing patient-centered care.
- The influence of role ambiguity and role-related emotional labor on burnout. Role ambiguity may lead to conflict [60] and role-related emotional labor [69], which correlate with burnout and intent to leave in nursing [60]. Evaluating whether role ambiguity affects PA professional well-being would be useful. Gaining a deeper understanding of the interplay among role ambiguity, team culture, and burnout in the PA profession would also be worthwhile.
- Diversity and inclusion in the PA profession. One cross-sectional study suggested that PAs who identified as African American, Native American, and Hispanic/Latino may be less satisfied with the PA profession [50]. Although the results of this small study are not generalizable, it is a reminder that the PA profession lacks diversity [20]. Eighty-seven percent of certified PAs are white [20], and the profession has experienced a 10-year decline in diversity in the profession, despite an increase in the growth of the profession [70]. Evaluation of factors that contribute to diversity in the profession, and factors that contribute to satisfaction among PAs who identify as racial or ethnic minorities, is necessary to support and cultivate a representative workforce.
Conclusion
While few articles focus exclusively on PA work-life experiences, the existing data demonstrate several fundamental themes that can be extrapolated to the experiences of PAs. PAs working in high burnout specialties—such as emergency medicine, primary care, hospice and palliative care, and oncology—appear to develop burnout at levels similar to their physician colleagues [10,11,35,36,40]. However, some studies indicate that job and career satisfaction remain high [11,36]. The adaptable nature of the PA role lends itself to specialty transition, which may serve as a buffer against the long-term effects of burnout [34]. However, the profession lacks rigorous, longitudinal, and robust studies on factors that contribute to burnout. There is clearly much work to be done to support patients and communities in need of high-quality, safe, and accessible team-based care. PA burnout, like burnout among other health care professionals, ultimately damages the health care system and patient care. Discovering insights that prevent burnout and promote engagement will be valuable not only for health care teams but also for society’s overall health.
APPENDIX A
Join the conversation!
![]() Tweet this! New from @theNAMedicine: Burnout and Job and Career Satisfaction in the Physician Assistant Profession: A Review of the Literature: https://doi.org/10.31478/201812b #NAMPerspectives #ClinicianWellBeing
Tweet this! New from @theNAMedicine: Burnout and Job and Career Satisfaction in the Physician Assistant Profession: A Review of the Literature: https://doi.org/10.31478/201812b #NAMPerspectives #ClinicianWellBeing
![]() Tweet this! Physician assistants are an important part of health care teams, but little research has been done to understand how to best support their well-being & career satisfaction: https://doi.org/10.31478/201812b #NAMPerspectives #ClinicianWellBeing
Tweet this! Physician assistants are an important part of health care teams, but little research has been done to understand how to best support their well-being & career satisfaction: https://doi.org/10.31478/201812b #NAMPerspectives #ClinicianWellBeing
![]() Tweet this! More people are entering the physician assistant profession than ever before, but little is known about PA burnout and contributors to well-being. Here’s what we do know: https://doi.org/10.31478/201812b #NAMPerspectives #ClinicianWellBeing
Tweet this! More people are entering the physician assistant profession than ever before, but little is known about PA burnout and contributors to well-being. Here’s what we do know: https://doi.org/10.31478/201812b #NAMPerspectives #ClinicianWellBeing
![]() Tweet this! A comprehensive literature review reveals some trends in burnout and well-being among physician assistants, but additional research is needed: https://doi.org/10.31478/201812b #NAMPerspectives #ClinicianWellBeing
Tweet this! A comprehensive literature review reveals some trends in burnout and well-being among physician assistants, but additional research is needed: https://doi.org/10.31478/201812b #NAMPerspectives #ClinicianWellBeing
Download the graphics below and share them on social media!


References
NOTE: This list of references was updated on February 4, 2021 to reflect the retraction of reference #6, Panagioti et al., 2018. Locations where this reference was cited throughout the paper have been struck through. This reference did not significantly impact the development of this paper or the conclusions posited therein.
- Heinemann, L. V., and T. Heinemann. 2017. Burnout research: Emergence and scientific investigation of a contested diagnosis. Sage Open 7(1):1-12. https://doi.org/10.1177/2158244017697154
- Zellar, K. L., P. L. Perrewe, and W. A. Hochwarter. 2000. Burnout in health care: The role of the five factors of personality. Journal of Applied Social Psychology 30(8):1570-1598. https://doi.org/10.1111/j.1559-1816.2000.tb02456.x
- Shanafelt, T. D., S. Boone, L. Tan, N. Dyrbye, W. Sotile, D. Satele, C. P. West, J. Sloan, and M. R. Oreskovich. 2012. Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Archives of Internal Medicine 172(18):1377-1385. https://doi.org/10.1001/archinternmed.2012.3199
- Hoff, T., S. Carabetta, and G. E. Collinson. 2017. Satisfaction, burnout, and turnover among nurse practitioners and physician assistants: A review of the empirical literature. Medical Care Research and Review. https://doi.org/10.1177/1077558717730157.
- McHugh, M. D., A. Kutney-Lee, J. P. Cimiotti, D. M. Sloane, and L. H. Aiken. 2011. Nurses’ widespread job dissatisfaction, burnout, and frustration with health benefits signal problems for patient care. Health Affairs 30:202-210. https://doi.org/10.1377/hlthaff.2010.0100
Panagioti, M., K. Geraghty, J. Johnson, Zhou, E. Panagopoulou, C. Chew-Graham, D. Peters, A. Hodkinson, R. Riley, and A. Esmail. 2018. Association between physician burnout and patient safety, professionalism, and patient satisfaction: A systematic review and meta-analysis. JAMA Internal Medicine 178(10):1317-1330. https://doi.org/10.1001/jamainternmed.2018.3713- Bodenheimer, T., and C. Sinsky. 2014. From triple to quadruple aim: Care of the patient requires care of the provider. Annals of Family Medicine 12(6):573-576. https://doi.org/10.1370/afm.1713
- Shanafelt, T. D., G. Gorringe, R. Menaker, K. A. Storz, D. Reeves, and S. J. Buskirk. 2015. Impact of organizational leadership on physician burnout and satisfaction. Mayo Clinic Proceedings 90(4):432. https://doi.org/10.1016/j.mayocp.2015.01.012
- Shanafelt, T. D., O. Hasan, L. N. Dyrbye, C. Sinsky, D. Satele, J. Sloan, and C. P. West. 2015. Changes in burnout and satisfaction with work-life balance in physicians and the general US working population between 2011 and 2014. Mayo Clinic Proceedings 90(12):1600-1613. https://doi.org/10.1016/j.mayocp.2015.08.023
- Benson, M. A., T. Peterson, L. Salazar, W. Morris, R. Hall, B. Howlett, and P. Phelps. 2016. Burnout in rural physician assistants. Journal of Physician Assistant Education Association 27(2):81-83. https://doi.org/10.1097/JPA.0000000000000069
- Varner, D. F., and B. K. Foutch. 2014. Depression and burnout symptoms among air force family medicine providers. Journal of the American Academy of Physician Assistants 27(5):42-46. https://doi.org/10.1097/01.JAA.0000446373.63790.c9
- Whitebird, R. R., L. I. Solberg, A. L. Crain, R. C. Rossom, A. Beck, C. Neely, M. Dreskin, and K. J. Coleman. 2017. Clinician burnout and satisfaction with resources in caring for complex patients. General Hospital Psychiatry 44(1):91-95. https://doi.org/10.1016/j.genhosppsych.2016.03.004
- Hudson, C. L. 1961. Expansion of medical professional services with non-professional personnel. JAMA 176(10):839-841. https://doi.org/10.1001/jama.1961.03040230005002
- Jones, P. E., and J. F. Cawley. 1994. Physician assistants and health system reform. JAMA 271(16):1266-1272. https://doi.org/10.1001/jama.1994.03510400052031
- PA scope of practice. 2018. Alexandria, VA: American Academy of Physician Assistants. Available at: https://www.aapa.org/wp-content/uploads/2017/01/Issue-brief_Scope-of-Practice_0117-1.pdf (accessed September 3, 2018).
- Curtis, L. G., L. Dobbs, and C. A. Hildebrandt. 2017. Female PAs—where are we today? Journal of the American Academy of Physician Assistants 30(9):44-48. https://doi.org/10.1097/01.jaa.0000522137.14188.90
- By the numbers: Program report 31: Data from the 2016 program survey. Washington, DC: Physician Assistant Education Association. Available at: https://paeaonline.org/wp-content/uploads/2017/06/Program-Survey-31_V4_Updated-June-2017.pdf (accessed August 3, 2018).
- Accredited programs. 2018. Johns Creek, GA: Accreditation Review Commission on Education for the Physician Assistant. Available at: http://www.arc-pa.org/accreditation/accredited-programs (accessed August 2, 2018).
- Cawley J. F. 1994. Physician assistants in the health care workforce. JAMA 271(16):1266-1272. https://doi.org/10.1001/jama.1994.03510400052031
- 2017 statistical profile on certified physician assistants: An annual report of the National Commission on Certification of Physician Assistants. Johns Creek, GA: National Commission on Certification of Physician Assistants. Available at: http://prodcmsstoragesa.blob.core.windows.net/uploads/files/2017StatisticalProfileofCertifiedPhysicianAssistants%206.27.pdf (accessed August 31, 2018).
- Number of nurse practitioners hits new record high. 2018. Austin, TX: American Association of Nurse Practitioners. Available at: https://www.aanp.org/press-room/press-releases/173-press-room/2018-press-releases/2190-number-of-nurse-practitioners-hits-new-record-high (accessed August 3, 2018).
- Professionally active physicians. 2018. Oakland, CA: Henry J. Kaiser Family Foundation. Available at: https://www.kff.org/other/state-indicator/total-active-physicians/?currentTimeframe=0&selectedRows=%7B%22states%22:%7B%22all%22:%7B%7D%7D,%22wrapups%22:%7B%22united-states%22:%7B%7D%7D%7D&sortModel=%7B%22colId%22:%22Location%22,%22sort%22:%22asc%22%7D (accessed August 3, 2018).
- Carter, R. D., and D. R. Oliver. 1983. An analysis of salaries for clinically active physician assistants. Physician Assistant 7(7):14-16, 19, 23-24.
- First annual report on physician assistant educational programs in the United States, 1984-85. 1985. Edited by D. Oliver, J. Baker, and W. Donahue. Washington, DC: Association of Physician Assistant Programs.
- Twenty-second annual report on physician assistant educational programs in the United States, 2005-2006. 2006. Edited by A. Simon, and M. Link. Washington, DC: Physician Assistant Education Association.
- Hooker, R. S., J. F. Cawley, and W. Leinweber. 2010. Career flexibility of physician assistants and the potential for more primary care. Health Affairs 29(5):880-886. https://doi.org/10.1377/hlthaff.2009.0884
- Smith, N. 2017. Career flexibility within the PA profession. AAPA News Central. Available at: https://www.aapa.org/news-central/2017/07/career-flexibility-within-pa-profession (accessed August 31, 2018).
- By the numbers: Matriculating students 2015. 2016. Washington, DC: Physician Assistant Education Association. Available at: https://paeaonline.org/wp-content/uploads/2016/12/2015-matriculating-student-survey.pdf (accessed August 2, 2018).
- Essary, A. C., B. H. Coplan, J. F. Cawley, S. Schneller, and R. L. Ohsfeldt. 2016. Women, family medicine and career choice: An opportunity cost analysis. Journal of the American Academy of Physician Assistants 29(9):44-48. https://doi.org/10.1097/01.JAA.0000490949.02814.bc
- Hooker, R. S., S. P. Robie, J. M. Coombs, and J. F. Cawley. 2013. The changing physician assistant profession: A gender shift. Journal of the American Academy of Physician Assistants 26(9):36-44. https://doi.org/10.1097/01.jaa.0000433914.54617.a0
- Berwick, D. M., T. W. Nolan, and J. Whittington. 2008. The triple aim: Care, health, and cost. Health Affairs 27(3):759-769. https://doi.org/10.1377/hlthaff.27.3.759
- Dyrbye, L. N., D. Meyers, J. Ripp, N. Dalal, S. B. Bird, and S. Sen. 2018. A Pragmatic Approach for Organizations to Measure Health Care Professional Well-Being. NAM Perspectives. Discussion Paper, National Academy of Medicine, Washington, DC. https://doi.org/10.31478/201810b
- Reid, R. J., P. A. Fishman, O. Yu, T. R. Ross, J. T. Tufano, M. P. Soman, and E. B. Larson. 2009. Patient-centered medical home demonstration: A prospective, quasi-experimental, before and after evaluation. American Journal of Managed Care 15(9):e71-e87. Available at: https://pubmed.ncbi.nlm.nih.gov/19728768/ (accessed September 2, 2020).
- Coplan, B., T. McCall, N. Smith, V. Gellert, and A. Essary. 2018. Burnout, job satisfaction, and stress levels of PAs. Journal of the American Academy of Physician Assistants 31(9):42-46. https://doi.org/10.1097/01.JAA.0000544305.38577.84
- Bell, R. B., M. Davison, and D. Sefcik. 2002. A first survey: Measuring burnout in emergency medicine physician assistants. Journal of the American Academy of Physician Assistants 15(3):40-55. Available at: https://pubmed.ncbi.nlm.nih.gov/11949543/ (accessed September 2, 2020).
- Tetzlaff, E. D., H. M. Hylton, L. Demora, K. Ruth, and Y.-N. Wong. 2018. National study of burnout and career satisfaction among physician assistants in oncology: Implications for team-based care. Journal of Oncology Practice 14(1):e11-e22. https://doi.org/10.1200/JOP.2017.025544
- Kamal, A. H., J. H. Bull, S. P. Wolf, M. Swetz, T. D. Shanafelt, K. Ast, D. Kavalieratos, C. T. Sinclair, and A. P. Abernethy. 2016. Prevalence and predictors of burnout among hospice and palliative care clinicians in the U.S. Journal of Pain Symptom Management 51(4):690-696. https://doi.org/10.1016/j.jpainsymman.2015.10.020
- Kavalieratos, D., D. Siconolfi, J. Bull, R. M. Arnold, K. M. Swetz, and A. H. Kamal. 2016. “It’s like heart failure. It’s chronic . . . and it will kill you”: A qualitative analysis of burnout among hospice and palliative care clinicians. Journal of Pain Symptom Management 53(5):901-910.e1. https://doi.org/10.1016/j.jpainsymman.2016.12.337
- Walters, T. A., E. P. Matthews, and J. I. Dailey. 2014. Burnout in army health care providers. Military Medicine 179(9):1006-1012. https://doi.org/10.7205/MILMED-D-14-00058
- Spinelli, W. M., Fernstrom, K. M., Britt, H., and Pratt, R. 2016. “Seeing the patient is the joy”: A focus group analysis of burnout in outpatient providers. Family Medicine 48(4):273-277.
- Waddimba, A. C., M. A. Nieves, M. Scribani, N. Krupa, P. Jenkins, and J. May. 2015. Predictors of burnout among physicians and advanced-practice clinicians in central New York. Journal of Hospital Administration 4(6):21-30. Available at: http://www.sciedu.ca/journal/index.php/jha/article/download/7332/4555 (accessed September 2, 2020).
- Linzer, M., S. Poplau, E. Grossman, Varkey, S. Yale, E. Williams, L. Hicks, R. L. Brown, J. Wallock, D. Kohnhorst, and M. Barbouche. 2015. A cluster randomized trial of interventions to improve work conditions and clinician burnout in primary care: Results from the Healthy Work Place (HWP) Study. Journal of General Internal Medicine 30(8):1105-1111. https://doi.org/10.1007/s11606-015-3235-4
- Meredith, L. S., N. S. Hackbarth, J. Darling, H. P. Rodriguez, S. E. Stockdale, K. M. Cordasco, E. M. Yano, and L. V. Rubenstein. 2015. Emotional exhaustion in primary care during early implementation of the VA’s medical home transformation. Medical Care 53(3):253-260. https://doi.org/10.1097/MLR.0000000000000303
- LaBarbera, D. M. 2004. Physician assistant vocational satisfaction. Journal of the American Academy of Physician Assistants 17(10):34-36, 38, 40, 51. Available at: https://pubmed.ncbi.nlm.nih.gov/15532322/ (accessed September 2, 2020).
- LaBarbera, D. M. 2010. Gender differences in the vocational satisfaction of physician assistants. Journal of the American Academy of Physician Assistants 23(10):33-34, 36-39. https://doi.org/10.1097/01720610-201010000-00007.
- Biscardi, C. A., J. Mitchell, S. Simpkins, and Z. G. Pinto. 2013. Practice characteristics and lifestyle choices of men and women physician assistants and the relationship to career satisfaction. Journal of Allied Health 42(3):157-162. Available at: https://pubmed.ncbi.nlm.nih.gov/24013246/ (accessed September 2, 2020).
- Nelson, S., and R. S. Hooker. 2016. Physician assistants and nurse practitioners in rural Washington emergency departments. Journal of Physician Assistant Education 27(2):56-62. https://doi.org/10.1097/jpa.0000000000000074
- Pathman, D., T. Konrad, and R. Hooker. 2014. Physician assistants and nurse practitioners in the National Health Service Corps. Journal of the American Academy of Physician Assistants 27(12):35-43. https://doi.org/10.1097/01.jaa.0000456575.09015.24
- Henry, L. R., and R. S. Hooker. 2007. Retention of physician assistants in rural health clinics. Journal of Rural Health 23(3):207-214. https://doi.org/10.1111/j.1748-0361.2007.00092.x
- Filipova, A. A. 2014. Factors influencing the satisfaction of rural physician assistants. Journal of Allied Health 43(1):22-31. Available at: https://europepmc.org/article/med/24598896 (accessed September 2, 2020).
- Freeborn, D. K., R. S. Hooker, and C. R. Pope. 2002. Satisfaction and well-being of primary care providers in managed care. Evaluation & the Health Professions 25(2):239-254. https://doi.org/10.1177/01678702025002008
- Waddimba, A. C., M. Scribani, N. Krupa, J. J. May, and P. Jenkins. 2016. Frequency of satisfaction and dissatisfaction with practice among rural-based, group-employed physicians and non-physician practitioners. BMC Health Services Research 16(1):613. https://doi.org/10.1186/s12913-016-1777-8
- Shannon, K. M., and D. J. Merenstein. 2017. Evaluating the lifestyles of physicians and PAs in orthopedics. Journal of the American Academy of Physician Assistants 30(1):38-41. https://doi.org/10.1097/01.jaa.0000508212.42460.3a
- Coplan, B., N. Smith, and J. F. Cawley. 2017. PAs in primary care: Current status and workforce implications. Journal of American Association of Physician Assistants 30(9):35-42. https://doi.org/10.1097/01.JAA.0000522136.76069.15
- Dyrbye, L. N., T. D. Shanafelt, C. A. Sinsky, P. F. Cipriano, J. Bhatt, A. Ommaya, C. P. West, and D. Meyers. 2017. Burnout among health care professionals: A call to explore and address this underrecognized threat to safe, high-quality care. NAM Perspectives. Discussion Paper, National Academy of Medicine, Washington, DC. https://doi.org/10.31478/201707b
- Brown, S.D., M. J. Goske, and C. M. Johnson. 2009. Beyond substance abuse: Stress, burnout, and depression as causes of physician impairment and disruptive behavior. Journal of the American College of Radiology 6(7):479-485. https://doi.org/10.1016/j.jacr.2008.11.029
- Hooker, R. S., L. Kuilman, and C. M. Everett. 2015. Physician assistant job satisfaction: A narrative review of empirical research. Journal of Physician Assistant Education 26(4):176-186. https://doi.org/10.1097/JPA.0000000000000047
- West, C. P., L. N. Dyrbye, and T. D. Shanafelt. 2018. Physician burnout: Contributors, consequences and solutions. Journal of Internal Medicine 283(6):516-529. https://doi.org/10.1111/joim.12752
- Bartram, T., G. Casimir, N. Djurkovic, S. G. Leggat, and P. Stanton. 2012. Do perceived high performance work systems influence the relationship between emotional labour, burnout and intention to leave? A study of Australian nurses. Journal of Advanced Nursing 68(7):1567-1578. https://doi.org/10.1111/j.1365-2648.2012.05968.x
- Moran, B. 2014. The physician assistant will see you. The New York Times, August 1. Available at: https://www.nytimes.com/2014/08/03/education/edlife/the-physician-assistant-will-see-you.html (accessed September 2, 2020).
- Knox, M., R. Willard-Grace, B. Huang, and K. Grumbach. 2018. Maslach Burnout Inventory and a self-defined, single-item burnout measure produce different clinician and staff burnout estimates. Journal of General Internal Medicine 33(8):1344-1351. https://doi.org/10.1007/s11606-018-4507-6
- Willard-Grace, R., D. Hessler, E. Rogers, K. Dube, T. Bodenheimer, and K. Grumbach. 2014. Team structure and culture are associated with lower burnout in primary care. Journal of the American Board of Family Medicine 27(2):229-238. https://doi.org/10.3122/jabfm.2014.02.130215
- Bodenheimer, T., and R. Willard-Grace. 2016. Teamlets in primary care: Enhancing the patient and clinician experience. Journal of the American Board of Family Medicine 29(1):135-138. https://doi.org/10.3122/jabfm.2016.01.150176
- Forister, J. G., and D. Blessing. 2007. Professional burnout: A study of physician assistant educators. Journal of Physician Assistant Education 18(4):10-15. Available at: https://journals.lww.com/jpae/Abstract/2007/18040/Professional_Burnout__A_Study_of_Physician.3.aspx (accessed September 2, 2020).
- Graeff, E. C., J. S. Leafman, L. Wallace, and G. Stewart. 2014. Job satisfaction levels of physician assistant faculty in the United States. Journal of Physician Assistant Education 25(2):15-20. https://doi.org/10.1097/01367895-201425020-00004
- Boeve, W. D. 2007. A national study of job satisfaction factors among faculty in physician assistant education. Master’s theses and doctoral dissertations, 60. Available at: http://commons.emich.edu/theses/60 (accessed October 24, 2018).
- Coniglio, D., and D. Akroyd. 2015. Factors predicting physician assistant faculty intent to leave. Journal of Physician Assistant Education 26(3):113-122. https://doi.org/10.1097/jpa.0000000000000031
- By the numbers: Faculty report. Data from the 2017 faculty and directors survey. 2018. Washington, DC: Physician Assistant Education Association. Available at: https://paeaonline.org/wp-content/uploads/2018/04/FacultyDirectors3_20180418.pdf (accessed October 24, 2018).
- Grandey, A., S. C. Foo, M. Groth, and R. E. Goodwyn. 2012. Free to be you and me: A climate of authenticity alleviates burnout from emotional labor. Journal of Occupational Health Psychology 17(1):1-14. https://doi.org/10.1037/a0025102
- Coplan, B., T. G. Bautista, and R. W. Dehn. 2018. PA program characteristics and diversity in the profession. Journal of the American Academy of Physician Assistants 31(3):38-46. https://doi.org/10.1097/01.JAA.0000530295.15656.51