Burnout Among Health Care Professionals: A Call to Explore and Address This Underrecognized Threat to Safe, High-Quality Care
TW: suicide
The US health care system is rapidly changing in an effort to deliver better care, improve health, and lower costs while providing care for an aging population with high rates of chronic disease and co-morbidities. Among the changes affecting clinical practice are new payment and delivery approaches, electronic health records, patient portals, and publicly reported quality metrics—all of which change the landscape of how care is provided, documented, and reimbursed. Navigating these changes are health care professionals (HCPs), whose daily work is critical to the success of health care improvement. Unfortunately, as a result of these changes and resulting added pressures, many HCPs are burned out, a syndrome characterized by a high degree of emotional exhaustion and high depersonalization (i.e., cynicism), and a low sense of personal accomplishment from work [1, 2].
What Is the Extent of Burnout Among Health Care Professionals?
Physicians
More than half of US physicians are experiencing substantial symptoms of burnout. Physicians working in the specialties at the front lines of care (e.g., emergency medicine, family medicine, general internal medicine, neurology) are among the highest risk of burnout. Burnout is nearly twice as prevalent among physicians as US workers in other fields after controlling for work hours and other factors [1,2]. Between 2011 and 2014, the prevalence of burnout increased by 9 percent among physicians while remaining stable in other US workers. Several studies have also found a high prevalence of burnout and depression among medical students and residents, with rates higher than those of age-similar individuals pursuing other careers [3-9].
Nurses and Other Health Care Professionals
Studies of nurses report a similarly high prevalence of burnout and depression. In a 1999 study of more than 10,000 registered inpatient nurses, 43 percent had high degree of emotional exhaustion [10]. A subsequent study of approximately 68,000 registered nurses in 2007 reported that 35 percent, 37 percent, and 22 percent of hospital nurses, nursing home nurses, and nurses working in other settings had high degree of emotional exhaustion [11]. The prevalence of depression may also be higher among nurses than other US workers. In a study of 1,171 registered inpatient nurses, 18 percent had depression versus a national prevalence of approximately 9 percent [12]. Less is known about other members of the health care team, although existing data suggest a similar prevalence of burnout among nurse practitioners and physician assistants [13].
Why Should We Be Concerned About Burnout Among Health Care Professionals?
Quality and Safety
There are cross-sectional studies of physicians that suggest a significant effect on quality and risk of medical malpractice suits. In cross-sectional studies of more than 7,100 US surgeons, burnout was an independent predictor of reporting a recent major medical error [14] and being involved in a medical malpractice suit [15] on multivariate analysis that is controlled for other personal and professional factors. The relationship between burnout and medical error is likely bidirectional. In a longitudinal study of internal medicine residents, higher levels of burnout were associated with increased odds of reporting an error in the subsequent 3 months. Self-perceived medical errors were also associated with worsening burnout, depressive symptoms, and decrease in quality of life, suggesting a cyclical relationship between medical errors and distress [16, 17]. Mean stress levels of hospital employees have also been shown to correlate with the number of hospital malpractice suits [18], and mean burnout levels among hospital nurses are an independent predictor of health care–associated infection [19]. Other studies have found that as mean emotional exhaustion levels of physicians and nurses working in intensive care units rose, so did standardized patient mortality ratios [20], while perceived quality of interpersonal teamwork deteriorated [21].
Patient Satisfaction
Cross-sectional studies with modest sample sizes have reported significant correlations between a physician’s degree of depersonalization and patient satisfaction with their hospital care [22] and between a physician’s job satisfaction and patient satisfaction with their health care [23] and patient-reported adherence to medical advice [24]. Additional studies have reported an inverse relationship between nurse job satisfaction and emotional exhaustion and patient satisfaction ratings across a variety of domains [11, 25, 26].
Turnover and Reduction of Work Effort
Cross-sectional studies of physicians have found burnout to be independently associated with job dissatisfaction [27] and more than 200 percent increased odds of intent to leave [28, 29] the current practice for reasons other than retirement. Similarly, in studies of nurses, burnout and job dissatisfaction were associated with plans to leave the current job or nursing field [30, 31, 32]. This dissatisfaction and intent often translates into action. A longitudinal study of physicians reported that each 1-point increase in emotional exhaustion or 1-point decrease in job satisfaction between 2011 and 2013 was associated with a 28 percent and 67 percent greater likelihood, respectively, of reduction in professional effort (i.e., reduction in work hours according to payroll records) over the following year [33], resulting in a loss of productivity at the national level estimated to equate to eliminating the graduating classes of seven medical schools [34]. Other studies support this relationship between burnout and leaving the clinical practice [27, 35, 36]. Although leaving one’s current job or reducing work hours may provide individual relief [34], these tactics further strain a health care system already struggling to meet access needs [37].
Health Care Costs
HCP turnover has financial implications for health care organizations. The cost of turnover among RNs is estimated at 1.2 to 1.3 times their salary (estimated total costs of $82,000–$88,000 per RN in 2007) [38, 39]. Costs to replace one physician depend on specialty, location, and length of vacancy, with estimated costs ranging from hundreds of thousands to more than $1 million [40, 41]. Several small studies point to the possibility of physicians experiencing burnout or high workloads making more referrals and ordering more tests [42, 43]. Burnout may also increase health care expenditures indirectly via higher rates of medical errors [14, 16, 17] and malpractice claims [14, 15], absenteeism, and lower job productivity [12, 44-47].
Personal Consequences
HCP burnout represents real suffering among people dedicated to preventing and relieving the suffering of others. Cross-sectional studies of physicians have found burnout to be independently associated with 25 percent increased odds of alcohol abuse/dependence and 200 percent increased odds of suicidal ideation among physicians [48, 49]. In a longitudinal study of medical students, burnout predicted development of suicidal thoughts over the ensuing year, independent of symptoms of depression [7]. Physicians are at increased risk of suicide compared with the US general population [50], with the suicide rate among male physicians 40 percent higher than that of other males in the population and the suicide rate among female physicians 130 percent higher than that of other females in the population [50].
What Is Driving Burnout Among Health Care Professionals?
Work-Related Factors
A large number of studies suggest that work-related stress fuels burnout [51] and job dissatisfaction among HCPs [52, 53]. Work process inefficiencies (e.g., computerized order entry and documentation), excessive workloads (e.g., work hours, overnight call frequency, nurse-patient ratios), work-home conflicts, organizational climate factors (e.g., management culture; lack of physician-nurse collaboration, value congruence, opportunities for advancement, and social support), and deterioration in control, autonomy, and meaning at work have been associated with burnout among physicians and nurses [1, 10, 11, 27, 30, 31, 45, 54-65]. For example, multivariate analyses of data from cross-sectional studies of physicians have reported independent relationships between burnout and work hours (3 percent increased odds for each additional hour/week), night or weekend call (3–9 percent increased odds for each additional night or weekend on call), time spent at home on work-related tasks (2 percent increased odds for each additional hour/week), and work-home conflict (200–250 percent increased odds). In a study of inpatient nurses, each increase of one patient per nursing staff ratio (self-reported staffing levels) increased odds of high degree of emotional exhaustion by 23 percent and job dissatisfaction by 15 percent [10]. Moral distress, stemming from factors such as perceived powerlessness, unnecessary/futile care, inadequate informed consent, and false hope [66], is also a significant predictor of burnout among nurses [65]. Registered nurses who worked in nursing homes may also be at higher risk for burnout and lower job satisfaction than nurses who work in other settings [11].
Cross-sectional studies have consistently found physician specialty to be an independent predictor of burnout, with some specialties associated with 40 percent lower odds of burnout (e.g., dermatology) and others associated with up to 300 percent increased odds of burnout (e.g., emergency medicine, general internal medicine, neurology) in comparison with other specialties [1, 2, 27, 35, 55, 57, 58, 67], suggesting there is something unique to the work lives in these specialties that contributes to increased risk. There may also be distinct work-related drivers for physicians in private practice, as several studies have found them at approximately 20 percent higher odds for burnout independent of specialty, work hours, incentive pay, and a variety of other factors [2, 35, 55, 58]. Multivariate analyses of data from cross-sectional studies of physicians have reported independent relationships between burnout and incentive pay (130 percent increased odds versus other salary models), career stage (25 percent more likely among midcareer physicians than early or late-career), career fit (275 percent more likely among physicians who spend less than 20 percent of their work effort on the activity they find most personally meaningful), and use of computerized physician order entry (29 percent more likely among physicians who enter orders into a computer) [35, 57, 58]. Other aspects within the work environment that drive clerical burden likely also contribute [58, 68, 69]. Additionally, leadership behaviors matter [70]. How well leaders seek input from, inform, mentor, and recognize individuals for their contributions relates to burnout and the career satisfaction of the physicians they lead [70]. Large national studies of physicians also suggest that organizations that provide physicians with control over workplace issues are more likely to employ physicians with higher career satisfaction and lower reported stress [36, 52].
Demographic Profiles of Those at Higher Risk
Cross-sectional studies of physicians have found independent relationships between burnout and physician sex, age, relationship status, age of children, and spousal/partner occupation [2, 27, 57, 71]. Although gender is not consistently an independent predictor of burnout after adjusting for age and other factors, some studies have found female physicians to have 30–60 percent increased odds of burnout [2, 58, 67]. Female physicians are more likely to experience depressive symptoms than male physicians; however, depression is not more common among female physicians than other females in the general population [50]. Younger physicians are also at increased odds of burnout, with those who are less than 55 years old at 200 percent increased risk compared with those older than 55. Having a child younger than 21 years old increases the odds of burnout by 54 percent, and having a spouse/partner who works as a nonphysician HCP increases the odds by 23 percent. We are unaware of any studies that have explored ethnic or racial differences in the prevalence of burnout among practicing physicians, although some work has been done in medical students [72]. Among other helping professionals, the prevalence of burnout among African Americans has been shown to be lower than among Caucasians [51, 73]. Individual characteristics, such as personality and interpersonal skills, and experiences may influence how HCPs deal with stress and adjust to rapidly changing work environments [74-77]. Research, however, suggests that individuals who choose to become physicians are not inherently more vulnerable to stress and burnout [78].
What Research Is Needed?
Despite decades of publications documenting the problem and some of its causes and potential consequences, many questions remain, and information on effective interventions remains limited [2, 79-81]. A major limitation of the existing research is that the vast majority of studies have been cross-sectional, hampering our ability to understand causality. Many studies lack the multivariate analyses needed to elucidate the extent to which hypothesized variables are independent predictors or interacting or confounding correlates. Only a limited number of the complex array of factors (e.g., workplace conditions and personal characteristics) that may contribute to burnout and poor job dissatisfaction among HCPs have been studied. There is a scarcity of research studies exploring differences by work setting (e.g., inpatient, outpatient, skilled nursing home) and the work experience of other members of the health care team, including nurse practitioners, physician assistants, pharmacists, medical assistants, and nonclinical staff. Terminology and measurement tools used vary substantially across studies, limiting comparisons across HCP populations, hampering efforts to quantitatively summarize outcomes (for example through meta-analyses), and slowing the rate of advancement in the field. Most intervention studies have used convenience sampling, lacked appropriate comparison groups, were short in duration, involved only a single discipline or organization, and focused primarily on individual interventions, such as mindfulness-based stress reduction, despite problems within the health care system being a much greater contributing factor to burnout and dissatisfaction [82]. These shortcomings should be addressed.
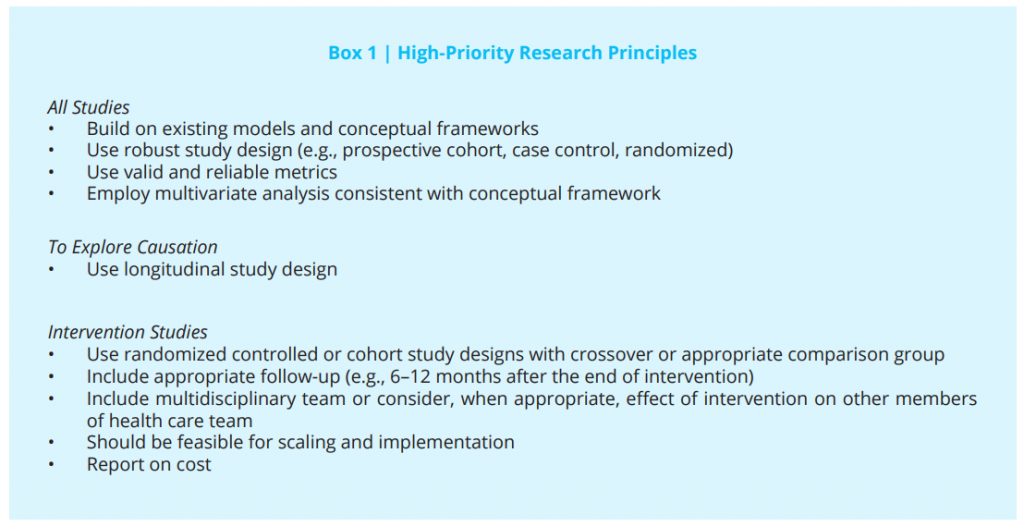
Future research should adhere to core research principles (Box 1). Methodologically rigorous research should build on existing models and conceptual frameworks [53, 83-87] and use instruments to measure domains of HCPs’ work-lives, experiences, burnout, and well-being (i.e., emotional, psychological, and social well-being) that have acceptable levels of reliability and validity. Despite the widespread use of study-specific and often single-item approaches to explore these dimensions, instruments with established reliability and validity to measure burnout, stress, engagement, quality of life, fatigue, and other dimensions of mental health exist, and their use should be encouraged [87]. The Maslach Burnout Inventory (MBI) is the gold standard for measuring burnout, with the MBI-Human Services Survey version most suitable for measuring burnout among HCPs (e.g., nurses, physicians, health aides, social workers, counselors, therapists) and the MBI-General Survey) version for others working in jobs such as customer service, management, and most other professions. Instruments designed to measure multiple dimensions of well-being (burnout, stress, work-life integration, meaning/purpose in work) specifically for physicians have also been developed [88-93] and validated [87]. These instruments have also proved useful for workers in other fields [88], and studies to establish national benchmarks for nurses, nurse practitioners, and physician assistants are ongoing. Those instruments with published national benchmarks for HCPs and demonstrated to have predictive validity for relevant outcomes are particularly useful [87-91]. Development of additional instruments to measure new constructs need to apply established rigorous scientific processes of instrument development and validation, including particular attention to concurrent and predictive validity.
To move the field forward, methodologically rigorous research should be conducted within the following three major areas:
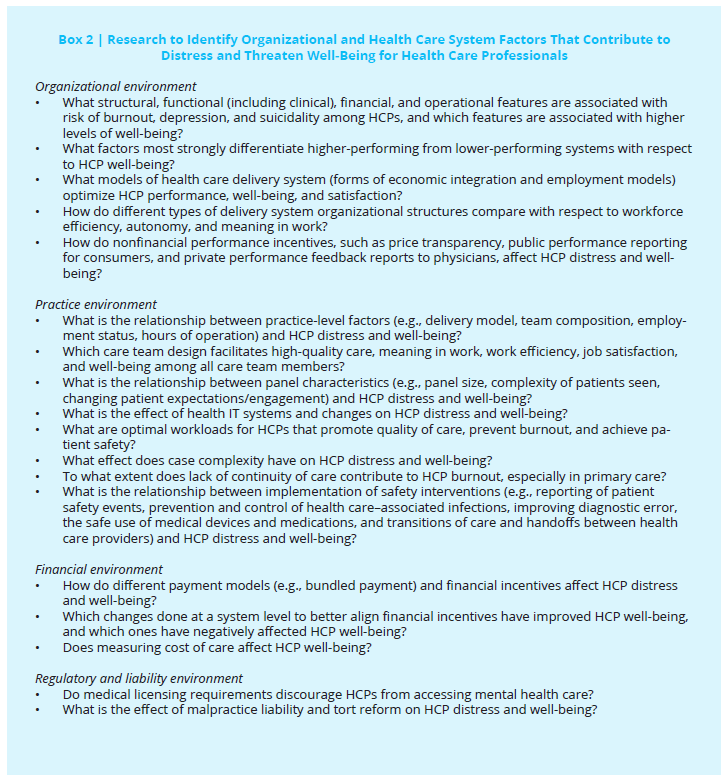
1) Research to identify organizational and health care system factors that increase risk of distress for health care professionals
Research is needed that creates new knowledge by identifying the organizational and health care system factors that are placing HCPs at increased risk for burnout. In particular, longitudinal studies are needed to better identify individual, work-unit, health care organization/employer, and health care system factors that contribute to poor well-being among HCPs. Research priorities within this domain are listed in Box 2. It is critical that researchers consider how factors may differentially affect different members of the health care team. For example, the incorporation of computer order entry may affect physicians, pharmacists, and nurses in different ways, increasing workload or stress for some while lessening it for others.
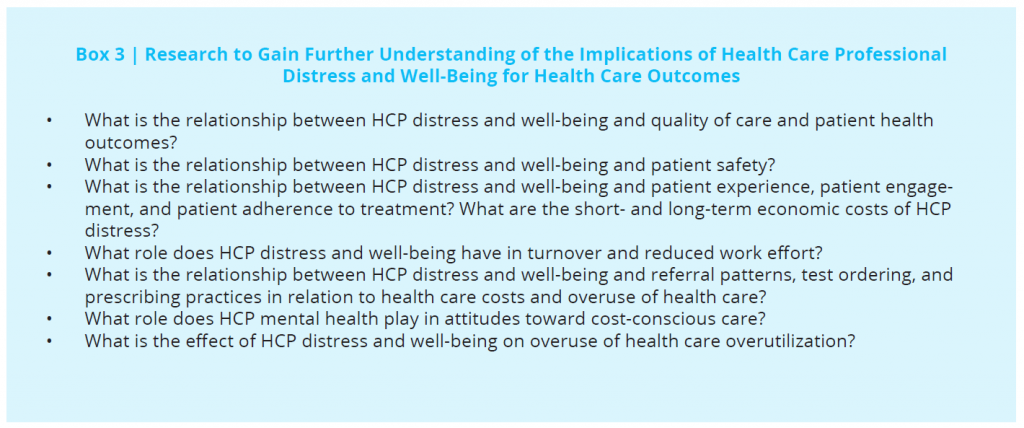
2) Research to gain further understanding of the implications of health care professional distress and well-being for health care outcomes
Longitudinal study designs and measured (rather than self-reported) health care outcomes are needed to advance our understanding of the professional consequences of HCP burnout and other forms of distress (Box 3). Given the effect of HCPs’ decisions on health care outcomes and costs, research should also focus on exploring relationships between HCPs’ distress, well-being, and referral patterns, test ordering, prescribing practices, and other decisions that affect health care quality, safety, and costs. Economic models that estimate the costs of poor HCP well-being are also needed. Efforts in this regard have begun, and additional studies are needed to maximize precision and generalizability [19, 94].
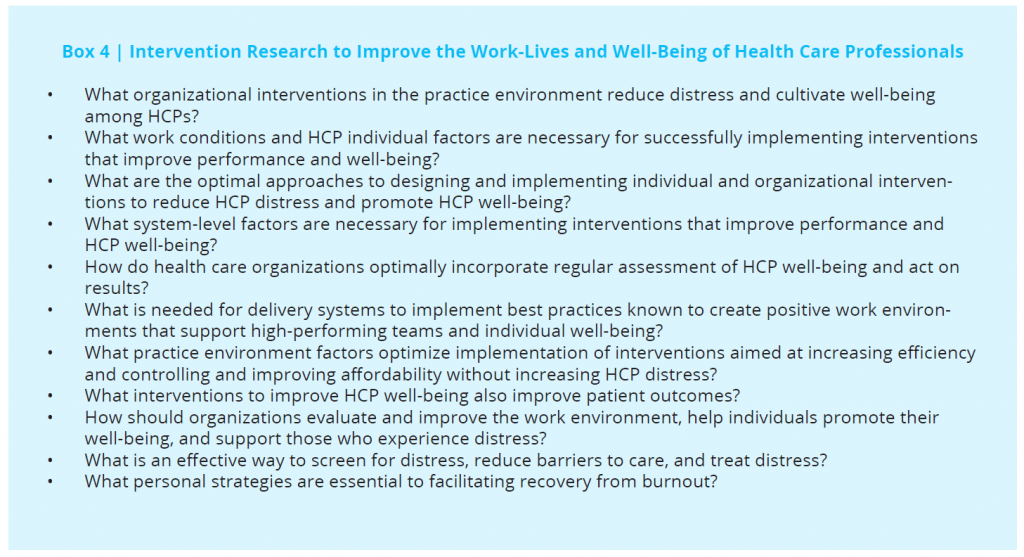
3) Intervention research to improve the work-lives and well-being of health care professionals
Relatively few methodologically robust intervention studies have been conducted [81, 95]. Intervention research should be a high priority. A recent systematic review and meta-analysis evaluating interventions to reduce physician burnout identified only 15 randomized controlled trials and 37 cohort studies [81]. The analysis concluded that a broad range of interventions are mildly to modestly effective in reducing physician burnout and that both organizational/structural- and individual-focused interventions are effective [81]. A second, subsequent meta-analysis resulted in similar findings [95]. Targets for intervention research are listed in Box 4 and will be further informed by the research proposed in area 1 above. Both interventions that include diverse groups of HCPs and others that target the unique needs of each type of HCP (e.g., physicians, nurses, nurse practitioners, physician assistants, pharmacists) are needed. It is also vital to determine the work conditions and HCP individual factors necessary for successfully implementing interventions that improve performance and well-being. Furthermore, studies assessing the degree to which interventions that improve HCP well-being also improve patient outcomes, access to care, and cost of care could have a transformative effect. Implementation-science principles should be used to promote the uptake of research findings into common health care environments.
Overcoming Barriers to Research
To date, research funding for studies designed to advance these three aims has been limited. Given the potentially serious ramifications of poor well-being and low job satisfaction among HCPs on the success of efforts to advance the patient experience of care, improve the health of populations, and reduce cost of health care, this should be remedied. Implementation of health care legislation and associated regulations should include appropriately scaled resources that can be allocated to study the effects of regulatory requirements associated with health care legislation on population health, patient satisfaction, cost, and HCP well-being and job satisfaction. Only with such effort will viable and sustainable solutions be realized.
Conclusion
The high prevalence of burnout among HCPs is cause for concern because it appears to be affecting quality, safety, and health care system performance. Efforts are needed to address this growing problem. Progress will require methodologically sound studies, adequate funding, and collaborative efforts. Formation of the National Academy of Medicine Action Collaborative (for a full list of participants, please see https://nam.edu/initiatives/clinician-resilience-and-well-being) is an important step. Many organizations have initiated steps to address aspects of the problem, but as indicated in this article, many important questions remain. The authors hope that research sponsors, institutions, clinician organizations, researchers, clinicians, and patients join in supporting enhanced research efforts focused on these topics.
If you are suicidal and need emergency help, call 911 immediately or 1-800-273-8255 if in the United States. If you are in another country, find a 24/7 hotline at www.iasp.info/resources/Crises_Centres.
Join the conversation!
![]() Tweet this! US clinicians are burnt out. What’s driving burn out & how can we fix it? Authors explore in @theNAMedicine paper: http://bit.ly/2shyYXc
Tweet this! US clinicians are burnt out. What’s driving burn out & how can we fix it? Authors explore in @theNAMedicine paper: http://bit.ly/2shyYXc
![]() Tweet this! New @theNAMedicine paper identifies high-priority research principles to further explore #ClinicianWellBeing: http://bit.ly/2shyYXc
Tweet this! New @theNAMedicine paper identifies high-priority research principles to further explore #ClinicianWellBeing: http://bit.ly/2shyYXc
![]() Tweet this! Clinician burnout affects, safety, productivity, patient satisfaction, & costs. How further research can help: http://bit.ly/2shyYXc
Tweet this! Clinician burnout affects, safety, productivity, patient satisfaction, & costs. How further research can help: http://bit.ly/2shyYXc
Download the graphic below and share it on social media!
References
- Shanafelt, T. D., S. Boone, L. Tan, L. N. Dyrbye, W. Sotile, D. Satele, C. P. West, J. Sloan, and M. R. Oreskovich. 2012. Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Archives of Internal Medicine 172:1377-85. https://doi.org/10.1001/archinternmed.2012.3199
- Shanafelt, T. D., O. Hasan, L. N. Dyrbye, C. Sinsky, D. Satele, J. Sloan, and C. P. West. 2015. Changes in burnout and satisfaction with work-life balance in physicians and the general US working population between 2011 and 2014. Mayo Clinic Proceedings 90:1600-13. https://doi.org/10.1016/j.mayocp.2015.08.023
- Mata, D. A., M. A. Ramos, N. Bansal, R. Khan, C. Guille, E. Di Angelantonio, and S. Sen. 2015. Prevalence of depression and depressive symptoms among resident physicians: A systematic review and meta-analysis. JAMA 314:2373-83. https://doi.org/10.1001/jama.2015.15845
- Rotenstein, L. S., M. A. Ramos, M. Torre, J. B. Segal, M. J. Peluso, C. Guille, S. Sen, and D. A. Mata. 2016. Prevalence of depression, depressive symptoms, and suicidal ideation among medical students. JAMA 316:2214-36. https://doi.org/10.1001/jama.2016.17324
- Dyrbye, L. N., F. S. Massie, A. Eacker, W. Harper, D. Power, S. J. Durning, M. R. Thomas, C. Moutier, D. Satele, J. Sloan, T. D. Shanafelt. 2010. Relationship between burnout and professional conduct and attitudes among US medical students. JAMA 304:1173-80. https://doi.org/10.1001/jama.2010.1318
- Dyrbye, L. N., and T. D. Shanafelt. 2016. A narrative review on burnout experienced by medical students and residents. Medical Education 50:132-49. https://doi.org/10.1111/medu.12927
- Dyrbye, L. N., M. R. Thomas, F. S. Massie, D. V. Power, A. Eacker, W. Harper, S. Durning, C. Moutier, D. W. Szydlo, P. J. Novotny, J. A. Sloan, and T. D. Shanafelt. 2008. Burnout and suicidal ideation among US medical students. Annals of Internal Medicine 149:334. https://doi.org/10.7326/0003-4819-149-5-200809020-00008
- Dyrbye, L. N., C. P. West, D. Satele, S. Boone, L. Tan, J. Sloan, and T. D. Shanafelt. 2014. Burnout among US medical students, residents, and early career physicians relative to the general US population. Academic Medicine 89:443-51. https://doi.org/10.1097/ACM.0000000000000134
- West, C. P., T. D. Shanafelt, and J. Kolars. 2011. Quality of life, burnout, educational debt, and medical knowledge among internal medicine residents. JAMA 306:952-60. https://doi.org/10.1001/jama.2011.1247
- Aiken, L. H., S. P. Clarke, D. M. Sloane, J. Sochalski, and J. H. Silber. 2002. Hospital nurse staffing and patient mortality, nurse burnout, and job dissatisfaction. JAMA 288:1987-93. https://doi.org/10.1001/jama.288.16.1987
- McHugh, M. D., A. Kutney-Lee, J. P. Cimiotti, D. M. Sloane, and L. H. Aiken. 2011. Nurses’ widespread job dissatisfaction, burnout, and frustration with health benefits signal problems for patient care. Health Affairs (Millwood) 30:202-10. https://doi.org/10.1377/hlthaff.2010.0100
- Letvak, S. A., C. J. Ruhm, and S. N. Gupta. 2012. Nurses’ presenteeism and its effects on self-reported quality of care and costs. The American Journal of Nursing 112:30-8; quiz 48, 39. https://doi.org/10.1097/01.NAJ.0000411176.15696.f9
- Benson, M. A., T. Peterson, L. Salazar, W. Morris, R. Hall, B. Howlett, and P. Phelps. 2016. Burnout in rural physician assistants: An initial study. Journal of Physician Assistant Education 27:81-3. https://doi.org/10.1097/JPA.0000000000000069
- Shanafelt, T. D., C. M. Balch, G. Bechamps, T. Russell, L. Dyrbye, D. Satele, P. Collicott, P. J. Novotny, J. Sloan, and J. Freischlag. 2010. Burnout and medical errors among American surgeons. Annals of Surgery 251:995-1000. https://doi.org/10.1097/SLA.0b013e3181bfdab3
- Balch, C. M., M. R. Oreskovich, L. N. Dyrbye, J. M. Colaiano, D. V. Satele, J. A. Sloan, and T. D. Shanafelt. 2011. Personal consequences of malpractice lawsuits on American surgeons. Journal of the American College of Surgeons 213:657-67. https://doi.org/10.1016/j.jamcollsurg.2011.08.005
- West, C. P., M. Huschka, P. Novotny, J. A. Sloan, J. C. Kolars, T. M. Haberman, and T. D. Shanafelt. 2006. Association of perceived medical errors with resident distress and empathy: A prospective longitudinal study. JAMA 296:1071-8. https://doi.org/10.1001/jama.296.9.1071
- West, C. P., A. D. Tan, T. M. Habermann, J. A. Sloan, and T. D. Shanafelt. 2009. Association of resident fatigue and distress with perceived medical errors. JAMA 302:1294-300. https://doi.org/10.1001/jama.2009.1389
- Jones, J. W., B. N. Barge, B. D. Steffy, L. M. Fay, L. K. Kunz, and L. J. Wuebker. 1988. Stress and medical malpractice: Organizational risk assessment and intervention. Journal of Applied Psychology 73:727-35. https://doi.org/10.1037/0021-9010.73.4.727
- Cimiotti, J. P., L. H. Aiken, D. M. Sloane, and E. S. Wu. 2012. Nurse staffing, burnout, and health care-associated infection. American Journal of Infection Control 40:486. https://doi.org/10.1016/j.ajic.2012.02.029
- Welp, A., L. L. Meier, and T. Manser. 2015. Emotional exhaustion and workload predict clinician-rated and objective patient safety. Frontiers in Psychology 5:1-13. https://doi.org/10.3389/fpsyg.2014.01573
- Welp, A., L. L. Meier, and T. Manser. 2016. The interplay between teamwork, clinicians’ emotional exhaustion, and clinician-rated patient safety: A longitudinal study. Critical Care (London, England) 20:110. https://doi.org/10.1186/s13054-016-1282-9
- Halbesleben, J. R. B., and C. Rathert. 2008. Linking physician burnout and patient outcomes: Exploring the dyadic relationship between physicians and patients. Health Care Management Review 33:29-39. https://doi.org/10.1097/01.HMR.0000304493.87898.72
- Haas, J. S., E. F. Cook, A. L. Puopolo, H. R. Burstin, P. D. Cleary, and T. A. Brennan. 2000. Is the professional satisfaction of general internists associated with patient satisfaction? Journal of General Internal Medicine 15:122-8. https://doi.org/10.1046/j.1525-1497.2000.02219.x
- DiMatteo, M. R., C. D. Sherbourne, R. D. Hays, L. Ordway, R. L. Kravitz, E. A. McGlynn, S. Kaplan, and W. H. Rogers. 1993. Physicians’ characteristics influence patients’ adherence to medical treatment: Results from the Medical Outcomes Study. Health Psychology 12:93-102. https://doi.org/10.1037/0278-6133.12.2.93
- Leiter, M. P., P. Harvie, and C. Frizzell. 1998. The correspondence of patient satisfaction and nurse burnout. Social Science & Medicine 47:1611-7. https://doi.org/10.1016/s0277-9536(98)00207-x
- Vahey, D. C., L. H. Aiken, D. M. Sloane, S. P. Clarke, and D. Vargas. 2004. Nurse burnout and patient satisfaction. Medical Care 42:II57-66. https://doi.org/10.1097/01.mlr.0000109126.50398.5a
- Shanafelt, T. D., C. M. Balch, G. J. Bechamps, T. Russell, L. Dyrbye, D. Satele, P. Collicott, P. J. Novotny, J. Sloan, and J. A. Freischlag. 2009. Burnout and career satisfaction among American surgeons. Annals of Surgery 250:463-71. https://doi.org/10.1097/SLA.0b013e3181ac4dfd
- Shanafelt, T. D., J. Sloan, D. Satele, and C. Balch. 2010. Why do surgeons consider leaving practice? Journal of the American College of Surgeons 212:421-2. https://doi.org/10.1016/j.jamcollsurg.2010.11.006
- Shanafelt, T. D., M. Raymond, M. Kosty, D. Satele, L. Horn, J. Pippen, Q. Chu, H. Chew, W. B. Clark, A. E. Hanley, J. Sloan, and W. J. Gradishar. 2014. Satisfaction with work-life balance and the career and retirement plans of US oncologists. Journal of Clinical Oncology 32:1127-35. https://doi.org/10.1200/JCO.2013.53.4560
- Leiter, M. P., and C. Maslach. 2009. Nurse turnover: The mediating role of burnout. Journal of Nursing Management 17:331-9. https://doi.org/10.1111/j.1365-2834.2009.01004.x
- Spence Laschinger, H. K., M. Leiter, A. Day, and D. Gilin. 2009. Workplace empowerment, incivility, and burnout: Impact on staff nurse recruitment and retention outcomes. Journal of Nursing Management 17:302-11. https://doi.org/10.1111/j.1365-2834.2009.00999.x
- Hayes, L. J., L. O’Brien-Pallas, C. Duffield, J. Shamian, J. Buchan, F. Hughes, H. K. Spence Laschinger, and N. North. 2011. Nurse turnover: A literature review—an update. International Journal of Nursing Studies 49:887-905. https://doi.org/10.1016/j.ijnurstu.2011.10.001
- Shanafelt, T. D., M. Mungo, J. Schmitgen, K. A. Storz, D. Reeves, S. N. Hayes, J. A. Sloan, S. J. Swensen, and S. J. Buskirk. 2016. Longitudinal study evaluating the association between physician burnout and changes in professional work effort. Mayo Clinic Proceedings 91:422-31. https://doi.org/10.1016/j.mayocp.2016.02.001
- Shanafelt, T. D., L. N. Dyrbye, C. P. West, and C. Sinsky. 2016. Potential impact of burnout on the US physician workforce. Mayo Clinic Proceedings 91:1667-8. https://doi.org/10.1016/j.mayocp.2016.08.016
- Dyrbye, L. N., S. L. Boone, D. V. Satele, J. A. Sloan, and T. D. Shanafelt. 2013. Physician satisfaction and burnout at different career stages. Mayo Clinic Proceedings 88:1358-637. https://doi.org/10.1016/j.mayocp.2013.07.016
- Linn, L. S., R. H. Brook, V. A. Clark, A. R. Davies, A. Fink, and J. Kosecoff. 1985. Physician and patient satisfaction as factors related to the organization of internal medicine group practices. Medical Care 23:1171-8. https://doi.org/10.1097/00005650-198510000-00006
- Association of American Medical Colleges. 2008. The complexities of physician supply and demand: Projections through 2025. Available at: https://aamc-black.global.ssl.fastly.net/production/media/filer_public/31/13/3113ee5c-a038-4c16-89af-294a69826650/2019_update_-_the_complexities_of_physician_supply_and_demand_-_projections_from_2017-2032.pdf (accessed August 31, 2020).
- Jones, C. B. 2005. The costs of nurse turnover, part 2: Application of the Nursing Turnover Cost Calculation Methodology. Journal of Nursing Administration 35:41-9. https://doi.org/10.1097/00005110-200501000-00014
- Jones, C. B. 2008. Revisiting nurse turnover costs: Adjusting for inflation. Journal of Nursing Administration 38:11-8. https://doi.org/10.1097/01.NNA.0000295636.03216.6f
- Fibuch, E., and A. Ahmed. 2015. Physician turnover: A costly problem. Physician Leadership Journal 2:22-5. Available at: https://pubmed.ncbi.nlm.nih.gov/26214946/ (accessed August 31, 2020).
- Buchbinder, S. B., M. Wilson, C. F. Melick, and N. R. Powe. 1999. Estimates of costs of primary care physician turnover. American Journal of Managed Care 5:1431-8. Available at: https://pubmed.ncbi.nlm.nih.gov/10662416/ (accessed August 31, 2020).
- Kushnir, T., D. Greenberg, N. Madjar, I. Hadari, Y. Yermiahu, and Y. G. Bachner. 2014. Is burnout associated with referral rates among primary care physicians in community clinics? Family Practice 31:44-50. https://doi.org/10.1093/fampra/cmt060
- Bachman, K. H., and D. K. Freeborn. 1999. HMO physicians’ use of referrals. Social Science & Medicine 48:547-57. https://doi.org/10.1016/s0277-9536(98)00380-3
- Parker, P. A., and J. A. Kulik. 1995. Burnout, self- and supervisor-rated job performance, and absenteeism among nurses. Journal of Behavioral Medicine 18:581-99. https://doi.org/10.1007/BF01857897
- Stone, P. W., Y. Du, and R. R. M. Gershon. 2007. Organizational climate and occupational health outcomes in hospital nurses. Journal of Occupational and Environmental Medicine 49:50-8. https://doi.org/10.1097/01.jom.0000251622.05429.0c
- Toppinen-Tanner, S., A. Ojajarvi, A. Vaananen, R. Kalimo, and P. Jappinen. 2005. Burnout as a predictor of medically certified sick-leave absences and their diagnosed causes. Behavioral Medicine 31:18-27. https://doi.org/10.3200/BMED.31.1.18-32
- Hilton, M. F., P. A. Scuffham, J. Sheridan, C. M. Cleary, N. Vecchio, and H. A. Whiteford. 2009. The association between mental disorders and productivity in treated and untreated employees. Journal of Occupational and Environmental Medicine 51:996-1003. https://doi.org/10.1097/JOM.0b013e3181b2ea30
- Oreskovich, M. R., K. L. Kaups, C. M. Balch, J. B. Hanks, D. Satele, J. Sloan, C. Meredith, A. Buhl, L. N. Dyrbye, and T. D. Shanafelt. 2012. The prevalence of alcohol use disorders among American surgeons. Archives of Surgery 147:168-74. https://doi.org/10.1001/archsurg.2011.1481
- Shanafelt, T. D., C. M. Balch, L. N. Dyrbye, G. Bechamps, T. Russell, D. Satele, T. Rummans, K. Swartz, P. J. Novotny, J. Sloan, and M. R. Oreskovich. 2011. Suicidal ideation among American surgeons. Archives of Surgery 146:54-62. https://doi.org/10.1001/archsurg.2010.292
- Center, C., M. Davis, T. Detre, D. E. Ford, W. Hansbrough, H. Hendin, J. Laszlo, D. A. Litts, J. Mann, P. A. Mansky, R. Michels, S. H. Miles, R. Proujansky, C. F. Reynolds, and M. M. Silverman. 2003. Confronting depression and suicide in physicians: A consensus statement. JAMA 289:3161-6. https://doi.org/10.1001/jama.289.23.3161
- Maslach, C., S. E. Jackson, and M. P. Leiter. 1996. Maslach burnout inventory manual (3rd ed.). Palo Alto, CA: Consulting Psychologists Press.
- Williams, E. S., T. R. Konrad, M. Linzer, J. McMurray, D. E. Pathman, M. Gerrity, M. D. Schwartz, W. E. Scheckler, and J. Douglas. 2002. Physician, practice, and patient characteristics related to primary care physician physical and mental health: Results from the Physician Worklife Study. Health Services Research 2;37:119-41. https://doi.org/10.1111/1475-6773.00007
- Williams, E. S., L. B. Manwell, T. R. Konrad, and M. Linzer. 2007. The relationship of organizational culture, stress, satisfaction, and burnout with physician-reported error and suboptimal patient care: Results from the MEMO study. Health Care Management Review 32:203-12. https://doi.org/10.1097/01.HMR.0000281626.28363.59
- Balch, C. M., T. D. Shanafelt, L. N. Dyrbye, T. R. Russell, G. J. Bechamps, and J. A. Freischlag. 2010. Surgeon distress as calibrated by hours worked and nights on call. Journal of the American College of Surgeons 211:609-19. https://doi.org/10.1016/j.jamcollsurg.2010.06.393
- Dyrbye, L. N., T. D. Shanafelt, C. Balch, D. Satele, and J. Freischlag. 2011. Relationship between work-home conflicts and burnout among American surgeons: A comparison by sex. Archives of Surgery 146:211-7. https://doi.org/10.1001/archsurg.2010.310
- Dyrbye, L. N., C. P. West, D. Satele, J. A. Sloan, and T. D. Shanafelt. 2011. Work-home conflict and burnout among academic internal medicine physicians. Archives of Internal Medicine 171:1207-9. https://doi.org/10.1001/archinternmed.2011.289
- Shanafelt, T. D., C. P. West, J. A. Sloan, P. J. Novotny, G. A. Poland, R. Menaker, T. A. Rummans, and L. N. Dyrbye. 2009. Career fit and burnout among academic faculty. Archives of Internal Medicine 169:990-5. https://doi.org/10.1001/archinternmed.2009.70
- Shanafelt, T. D., L. N. Dyrbye, C. Sinsky, O. Hasan, D. Satele, J. Sloan, and C. P. West. 2016. Relationship between clerical burden and characteristics of the electronic environment with physician burnout and professional satisfaction. Mayo Clinic Proceedings 91:836-48. https://doi.org/10.1016/j.mayocp.2016.05.007
- Campbell, D. A., Jr., S. S. Sonnad, F. E. Eckhauser, K. K. Campbell, and L. J. Greenfield. 2001. Burnout among American surgeons. Surgery 130:696-702; discussion 702-5. https://doi.org/10.1067/msy.2001.116676
- Bertges Yost, W., A. Eshelman, M. Raoufi, and M. S. Abouljoud. 2005. A national study of burnout among American transplant surgeons. Transplant Proceedings 37:1399-401. https://doi.org/10.1016/j.transproceed.2005.01.055
- Leiter, M. P., and H. K. Spence Laschinger. 2006. Relationships of work and practice environment to professional burnout: Testing a causal model. Nursing Research 55:137-46. https://doi.org/10.1097/00006199-200603000-00009
- Spence Laschinger, H. K., and M. P. Leiter. 2006. The impact of nursing work environments on patient safety outcomes: The mediating role of burnout/engagement. Journal of Nursing Administration 36:259-67. https://doi.org/10.1097/00005110-200605000-00019
- Laschinger Spence, H. K., C. A. Wong, and P. Greco. 2006. The impact of staff nurse empowerment on person-job fit and work engagement/burnout. Nursing Administration Quarterly 30:358-67. https://doi.org/10.1097/00006216-200610000-00008
- Woodhead, E. L., L. Northrop, and B. Edelstein. 2016. Stress, social support, and burnout among long-term care nursing staff. Journal of Applied Gerontology 35:84-105. https://doi.org/10.1177/0733464814542465
- Rushton, C. H., J. Batcheller, K. Schroeder, and P. Donohue. 2015. Burnout and resilience among nurses practicing in high-intensity settings. American Journal of Critical Care 24:412-20. https://doi.org/10.4037/ajcc2015291
- Hamric, A. B., and L. J. Blackhall. 2007. Nurse-physician perspectives on the care of dying patients in intensive care units: Collaboration, moral distress, and ethical climate. Critical Care Medicine 35:422-9. https://doi.org/10.1097/01.CCM.0000254722.50608.2D
- Shanafelt, T. D., M. R. Oreskovich, L. N. Dyrbye, D. V. Satele, J. B. Hanks, J. A. Sloan, and C. M. Balch. 2012. Avoiding burnout: The personal health habits and wellness practices of US surgeons. Annals of Surgery 255:625-33. https://doi.org/10.1097/SLA.0b013e31824b2fa0
- Sinsky, C., L. Colligan, L. Ling, M. Progmet, S. Reynolds, L. Goeders, J. Westbrook, M. Tutty, and G. Bilke. 2016. Allocation of physician time in ambulatory practice: A time and motion study in 4 specialties. Annals of Internal Medicine 165(11): 753-760. https://doi.org/10.7326/M16-0961
- Dyrbye, L. N., C. P. West, T. C. Burriss, and T. D. Shanafelt. 2012. Providing primary care in the United States: The work no one sees. Archives of Internal Medicine 172:1420-1. https://doi.org/10.1001/archinternmed.2012.3166
- Shanafelt, T. D., G. Gorringe, R. Menaker, K. A. Storz, D. Reeves, S. J. Buskirk, J. A. Sloan, and S. J. Swensen. 2015. Impact of organizational leadership on physician burnout and satisfaction. Mayo Clinic Proceedings 90:432-40. https://doi.org/10.1016/j.mayocp.2015.01.012
- Dyrbye, L. N., T. D. Shanafelt, C. Balch, D. Satele, and J. Freischlag. 2010. Physicians married/partnered to physicians: A comparative study in the American College of Surgeons. Journal of the American College of Surgeons 211:663-71. https://doi.org/10.1016/j.jamcollsurg.2010.03.032
- Dyrbye, L. N., M. R. Thomas, A. Eacker, W. Harper, F. S. Massie, Jr., D. V. Power, M. Huschka, P. J. Novotny, J. A. Sloan, and T. D. Shanafelt. 2007. Race, ethnicity, and medical student well-being in the United States. Archives of Internal Medicine 167:2103-9. https://doi.org/10.1001/archinte.167.19.2103
- Maslach, C. 1982. Burnout: The Cost of Caring. Englewood Cliffs, NJ: Prentice-Hall.
- McManus, I. C., A. Keeling, and E. Paice. 2004. Stress, burnout and doctors’ attitudes to work are determined by personality and learning style: A twelve year longitudinal study of UK medical graduates. BMC Medicine 2:29. https://doi.org/10.1186/1741-7015-2-29
- Tyssen, R., E. Hem, P. Vaglum, N. T. Gronvold, and O. Ekeberg. 2004. The process of suicidal planning among medical doctors: Predictors in a longitudinal Norwegian sample. Journal of Affective Disorders 80:191-8. https://doi.org/10.1016/S0165-0327(03)00091-0
- Tyssen, R., P. Vaglum, N. T. Gronvold, and O. Ekeberg. 2001. Factors in medical school that predict postgraduate mental health problems in need of treatment. A nationwide and longitudinal study. Medical Education 35:110-20. https://doi.org/10.1046/j.1365-2923.2001.00770.x
- Dyrbye, L. N., M. R. Thomas, J. L. Huntington, K. L. Lawson, P. J. Novotny, J. A. Sloan, and T. D. Shanafelt. 2006. Personal life events and medical student well-being: A multicenter study. Academic Medicine 81:374-84. https://doi.org/10.1097/00001888-200604000-00010
- Brazeau, C. M., T. D. Shanafelt, D. Satele, J. A. Sloan, and L. N. Dyrbye. 2012. Distress among matriculating medical students relative to the general population. Academic Medicine 89:1520-5. Available at: https://docksci.com/distress-among-matriculating-medical-students-relative-to-the-general-population_5a8f4766d64ab2321b692e54.html (accessed August 31, 2020).
- Shanafelt, T. D., K. A. Bradley, J. E. Wipf, and A. L. Back. 2002. Burnout and self-reported patient care in an internal medicine residency program. Annals of Internal Medicine 136:358-67. https://doi.org/10.7326/0003-4819-136-5-200203050-00008
- Shanafelt, T. D., J. A. Sloan, and T. M. Habermann. 2003. The well-being of physicians. American Journal of Medicine 114:513-9. https://doi.org/10.1016/s0002-9343(03)00117-7
- West, C. P., L. N. Dyrbye, P. J. Erwin, and T. D. Shanafelt. 2016. Interventions to prevent and reduce physician burnout: A systematic review and meta-analysis. The Lancet 388(10057):2272-2281. https://doi.org/10.1016/S0140-6736(16)31279-X
- Dyrbye, L. N., and T. D. Shanafelt. 2011. Physician burnout. A potential threat to successful health care reform. JAMA 305:2009-10. https://doi.org/10.1001/jama.2011.652
- West, C. P., and T. D. Shanafelt. 2007. The influence of personal and environment factors on professionalism in medical education. BMC Medical Education 7;7. https://doi.org/10.1186/1472-6920-7-29
- West, C. P., and T. D. Shanafelt. 2007. Physician well-being and professionalism. Minnesota Medicine 90:44-6. Available at: https://pubmed.ncbi.nlm.nih.gov/17899849/ (accessed August 31, 2020).
- Dunn, L. B., A. Iglewicz, and C. Moutier. 2008. A conceptual model of medical student well-being: Promoting resilience and preventing burnout. Academic Psychiatry 32:44-53. https://doi.org/10.1176/appi.ap.32.1.44
- Dyrbye, L. N., M. R. Thomas, and T. D. Shanafelt. 2005. Medical student distress: Causes, consequences, and proposed solutions. Mayo Clinic Proceedings 80:1615-22. https://doi.org/10.4065/80.12.1613
- Shanafelt, T. D., and J. H. Noseworthy. 2016. Executive leadership and physician well-being: Nine organizational strategies to promote engagement and reduce burnout. Mayo Clinic Proceedings 92:129-46. Available at: https://www.mayoclinicproceedings.org/article/S0025-6196(16)30625-5/pdf (accessed August 31, 2020).
- Dyrbye, L. N., D. Satele, and T. D. Shanafelt. 2016. Ability of a 9-item well-being index to identify distress and stratify quality of life in US workers. Journal of Occupational Environmental Medicine 58:810-7. https://doi.org/10.1097/JOM.0000000000000798
- Dyrbye, L. N., D. Satele, J. A. Sloan, and T. D. Shanafelt. 2013. Utility of a brief screening tool to identify physicians in distress. Journal of General Internal Medicine 28:421-7. https://doi.org/10.1007/s11606-012-2252-9
- Dyrbye, L. N., A. Schwartz, S. M. Downing, D. W. Szydlo, J. A. Sloan, and T. D. Shanafelt. 2011. Efficacy of a brief screening tool to identify medical students in distress. Academic Medicine 86:907-14. https://doi.org/10.1097/ACM.0b013e31821da615
- Dyrbye, L. N., D. Satele, J. A. Sloan, and T. D. Shanafelt. 2014. Ability of the Physician Well-Being Index to identify residents in distress. Journal of Graduate Medical Education 6:78-84. https://doi.org/10.4300/JGME-D-13-00117.1
- Linzer, M., S. Poplau, S. Babbott, T. Collins, L. Guzman-Corrales, J. Menk, M. L. Murphy, and K. Ovington. 2016. Worklife and wellness in academic general internal medicine: Results from a national survey. Journal of General Internal Medicine 31(9): 1004-1010. https://doi.org/10.1007/s11606-016-3720-4
- Shanafelt, T. D., K. L. Kaups, H. Nelson, D. V. Satele, J. A. Sloan, M. R. Oreskovich, and L. N. Dyrbye. 2014. An interactive individualized intervention to promote behavioral change to increase personal well-being in US surgeons. Annals of Surgery 259:82-8. https://doi.org/10.1097/SLA.0b013e3182a58fa4
- Dewa, C. S., P. Jacobs, N. X. Thanh, and D. Loong. 2014. An estimate of the cost of burnout on early retirement and reduction in clinical hours of practicing physicians in Canada. BMC Health Services Research 14:254. https://doi.org/10.1186/1472-6963-14-254
- Panagioti, M., E. Panagopoulou, P. Bower, G. Lewith, E. Kontopantelis, C. Chew-Graham, S. Dawson, H. van Marwijk, K. Geraghty, and A. Esmail. 2017. Controlled interventions to reduce burnout in physicians: A systematic review and meta-analysis. JAMA Internal Medicine 177(2):195-205. https://doi.org/10.1001/jamainternmed.2016.7674