An American Crisis: The Lack of Black Men in Medicine
This paper originally appeared in the Journal of Racial and Ethnic Health Disparities (2017) 4:317-321. Reprinted by permission.
The current state of diversity within the United States medical workforce does not reflect representative numbers of the Black male population. Research data continues to reveal continuing trends in the areas of discrimination, incarceration, health disparities and mortality with respect to Black males. The lack of increase in Black male medical school applications and matriculation contrasted by the continuing trends mentioned above illustrates that there is in fact an American crisis. We present here a call to arms, to address the need of African American men in medicine. The absence of Black males in medical school represents an American crisis that threatens efforts to effectively address health disparities and excellence in clinical care. This disturbing trend is in need of more empirical examination of medical school data specifically in the areas of: qualification barriers, race/ethnic classification and the impact of diversity on quality of health care in the U.S.
The number of Black males matriculating and graduating medical school is on a substantial decline. This decline has been caused in part we believe by barriers erected without empirical evidence of such barriers’ efficacy in predicting performance in medical school or practice. The decline has exacerbated health disparities. It is an American crisis because the declining diversity of doctors reduces the quality of health care in the U.S. as a whole—for all patient populations.
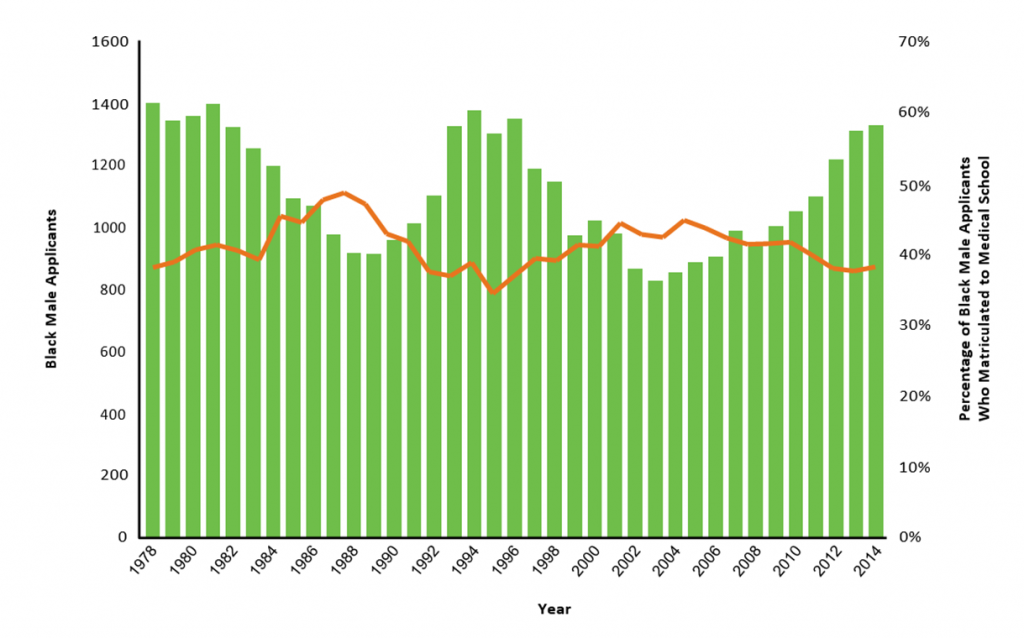
The number of Black males applying and matriculating to medical school has declined to very low levels [1]. In fact, matriculation numbers of Black males have failed to surpass the numbers from 35 years ago (Figure 1) while the number of positions in medical schools have increased during the same time frame. The reasons for this fact are manifold. Research data continue to reveal increasingly high rates of adverse life experiences with respect to Black males. While Black males matriculate to medical school at a low rate, they experience racial discrimination and pervasive health disparities with morbidity and mortality at a high rate. We believe the current state of society represents not just a crisis among Black men, but in fact an American crisis. To combat this crisis, it is necessary to ascertain the specific factors within society that support the growth and success of Black males in medicine in order to reverse the current trend.
At the same time, it is important to understand the systemic barriers to Black male success at all levels that result in their low participation rates in science, technology, engineering and math (STEM) [1]. Some of these conversations are uncomfortable. In his paper, Diversity 5.0, Laurencin states that diversity cannot truly be achieved until we recognize and attend to issues of past and pervasive present discrimination in charting our future course [7]. When examining the shrinking presence of the Black male in medical school, it is important to acknowledge and evaluate the inequitable balance that exists between Black men and individuals of other races. An American crisis exists when we fail to address the lack of opportunities for Black males in employment and educational opportunities.
Figure 1 | Number of black or African American male medical school applicants (bars) versus percentage of black or African American applicants who matriculated (line), 1978-2014. SOURCE: AAMC Data Warehouse: Applicant and Matriculant File, as of 5/11/2015.
The Decline in the Number of Black Male Medical Doctors
AAMC Report
We reviewed the 2015 AAMC report: Altering the Course: Black Males in Medicine to understand some of the factors contributing to 35 years of an overall declining trend of Black males in medicine. The report aimed to point out and help describe drivers of the decline of Black males applying and matriculating by delving into success factors, challenges and the role that academic medicine can play. Some successful influences are clear. For instance, a supportive network for a student serves as an essential component for academic success. Support sources help students navigate through challenges and aid in the development of resilience and extroverted personal attributes [1]. The accessibility of information within these social networks also can expose students to medical career options and ways to pursue them. Challenges influencing whether a Black male will apply or matriculate in a medical school program are multifaceted. For instance, financial cost, bias/stereotypes, imagery/career attractiveness and underperforming schools are factors within the trend of Black males in medicine. To appeal to young Black men, information on available resources and expansion of funding sources are needed to improve the application and matriculation rates. Financial costs of higher education can be a deterrent for those interested in medicine. Bias and stereotype perceptions also serve as barriers to study medicine. Negative media depictions of minorities can result in internalization of stereotypes and affect educational attainment and therefore achievement of career path goals. Another challenge involves underperforming schools impacting student educational eligibility. The high probability of Black males attending underperforming schools which lack pre-medical resources and experiencing teachers that lack cultural awareness influences the number of students in “the pipeline”. Similar to the supportive network mentioned above, Black males need Black physician role models within their communities and medical schools to increase career attractiveness [1]. In addition, academic leadership should be active and responsive to the absence of Black males in medical education in order to facilitate change and sustainability. With numbers of Black males matriculating to medical school not exceeding those from 1978—despite the prodigious expansion of medical schools in the US—the data and recommendations from the 2015 AAMC report demonstrate the ongoing need for broad efforts to support the development of a diverse and culturally competent physician workforce.
Qualified Selection
“Talent is universal, but opportunity is not.” Marc Nivet, EdD, MBA, AAMC Chief Diversity Officer [1]
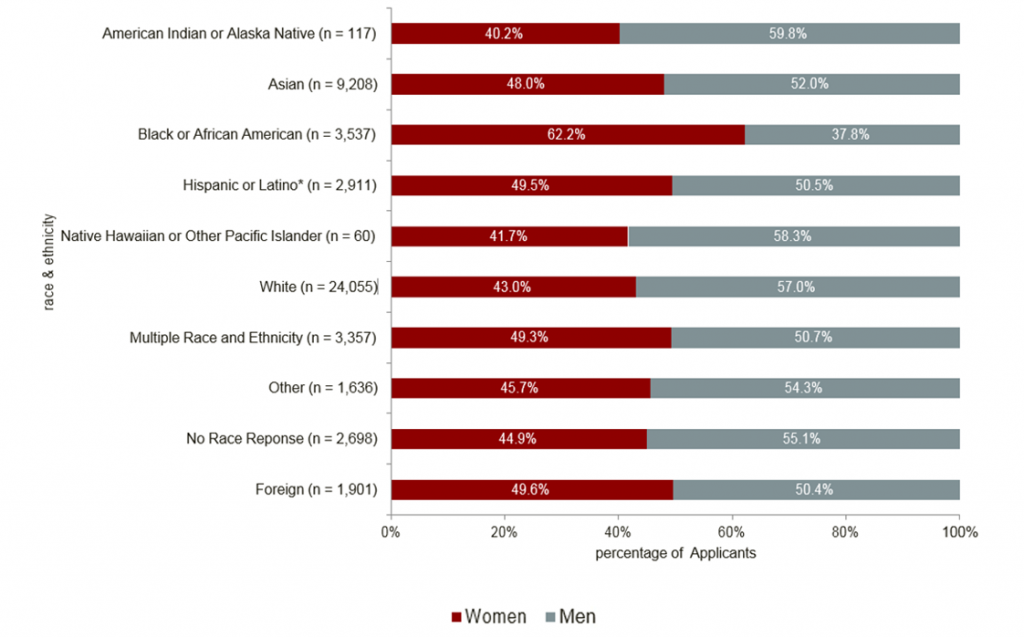
Data on the percentage of U.S. medical school applicants by gender and race/ethnicity in 2014 demonstrate the effects of the crisis seen in Black male applications to medical school. Only 37.8 percent of Blacks applying to medical school are men (Figure 2). The lack of Black men in medicine cannot be explained solely by what has been called “the pipeline”. For instance, despite being qualified, we suspect there are still implicit biases blocking opportunities for minorities entering medicine. We conducted an analysis of AAMC applicant and matriculation data. Our analysis compared the 1992-93 GPA scores of white males to the 2013-14 GPA scores of Black males [4]. The results indicated there that there were no significant differences in GPA scores of Black males in 2013-14 compared to white males GPA scores decades before. Thus the concept of qualified, and best qualified are perhaps through the lens of the majority, as grades (and scores) of Black males demonstrated levels that can be found in white counterparts now practicing as physicians. Despite overall increases in the number of Black male college graduates over the past two decades, the annual number of applications to medical school has not exceeded 1,410 since 1978 [1]. Are schools selecting a well-rounded set of qualified individuals through a holistic approach or are they selecting individuals that fit profiles created for the majority? True holistic approaches for admissions must be created and engaged that better define the notion of qualified and best qualified [5].
Additionally, if Black males achieved success rates in their applications to medical school commensurate to White male success rates, we believe that substantial increases in numbers of Black males matriculating in and graduating from medicine would occur. Black males who are unsuccessful in their first application have lower rates of reapplication then their white counterparts. This may be due to systemic discouragement for Black males in entering medicine. We advocate for medical schools to create opportunities to counsel formerly unsuccessful applicants on career guidance and reapplication to address this disparity.
Figure 2 | Percentage of U.S. medical school applicants by gender, race, and ethnicity, 2014. SOURCE: AAMC Data Warehouse: Applicant and Matriculant File, as of 3/26/2015.
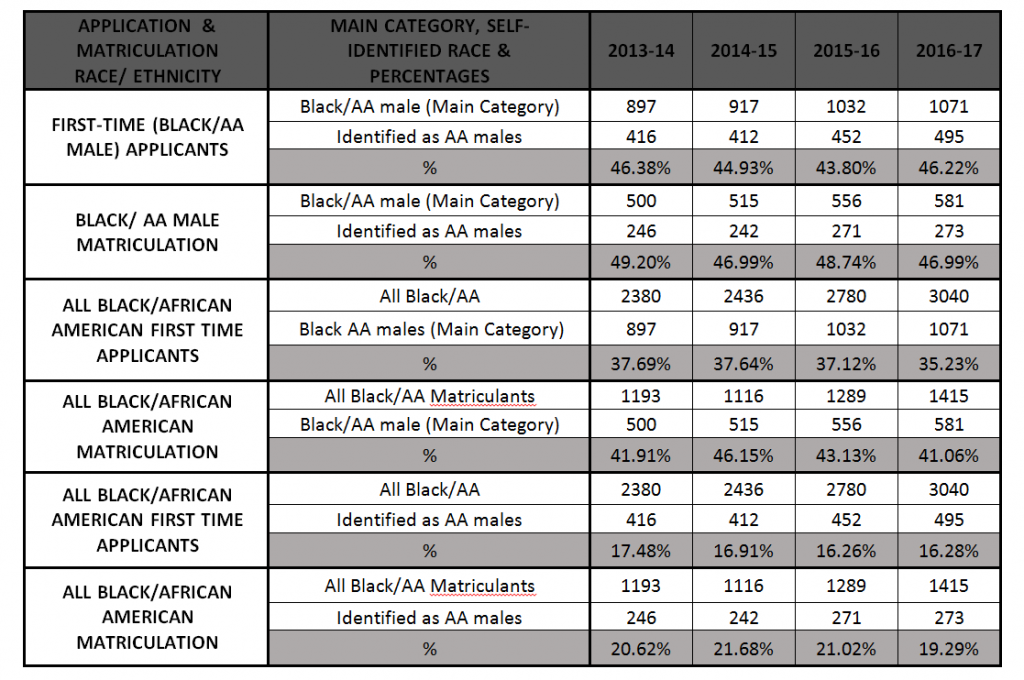
Examining the Crisis
Examination of the crisis reveals a more disturbing discovery for native-born Black/African American applicants and matriculants. Reported declining data may mask the existing crisis regarding U.S. born Black Males (identifying as African American). According to the AAMC data facts, the method for collecting race and ethnicity data were changed in 2013, resulting in the combining of Hispanic origin and race questions; allowing respondents to select sub categories options (i.e., African, African American, Afro Caribbean, Other Black or African American) [3]. Delving deeper into the new classifying methodology of Black Male medical school data uncovers stagnant application and matriculation trends specifically for those identifying as U.S. born Blacks/African American males despite recent incremental increases. The sub-racial/ethnic category African American male has not surpassed 46% application and 49% matriculation from 2013-14 – 2016-17 [3]. Data concerning the total number of Black/African American medical school students indicate the percentage of U.S. born African American males has not exceeded 17% first-time applications and 22% matriculations during the same timeframe (Figure 3). Consequently, a larger disparity may exist regarding African American males born in the U.S. applying to and matriculating in medical schools [1].
Figure 3 | AAMC Data Table A-12: Applicants, First-Time Applicants, Acceptees, and Matriculants to U.S. Medical Schools by Race/Ethnicity, 2013-2014 through 2016-2017.
The Impact of Diversity in Medicine: Disparities and the Quality of Care
African American men have the lowest life expectancy and highest death rate compared to men and women in other racial, ethnic and gender groups in the United States [12]. Why is this? U.S. health disparities for African American men are rooted in the history of slavery. Although those days are over, the legacy of segregation, the relatively recent Civil Rights Movement, and their interconnectedness with Health Disparities lives on today [11]. Increased physician diversity is often associated with greater access to care for patients with low incomes, racial and ethnic minorities, non-English speaking patients, and individuals with Medicaid [1, 2]. Given the significant inequalities in health, education, employment opportunities, and the effects of an unjust criminal justice system, the Black male is at a particular disadvantage. Despite some gains over the last few decades, African Americans, Latinos, and Native Americans remain underrepresented in the health profession relative to their proportion of the U.S. population [8]. Black men continue to be a minority of minorities in medicine [8]. Thus, the crisis we see in Black males entering medicine has prompted us to declare a call to action to understand these trends and to focus efforts toward solutions.
The creation of a diverse medical workforce is crucial to quality health care. Diversity can positively assist underserved populations with health care access, expand the number of stakeholders embedded in establishing quality care policy and provide more innovative studies on the contributors to health disparities. Minority medical students are more likely to work in underserved communities and therefore influence these community’s access to health care [9]. Diversity provides a bridge for those working in healthcare, policy and community leaders to collaborate specifically in areas directly and indirectly affecting public health interest. Innovation through the lens of different perspectives is needed in health disparity research. Research shows racial and ethnic diversity in medical education improves the learning and cross-cultural competencies of all doctors [5]. Exposure to a racially/ethnically diverse set of peers allows students to experience different cultural perspectives on a patient’s illness, and the results of treatments. Medical innovation and progressive policy initiatives in medicine are dependent upon diversity efforts.
Our call to action is to address not just a Black male crisis, but what is in fact an American crisis. The lack of increase in Black male medical school applications and matriculation contrasted by the continuing trends mentioned above creates a perfect storm for health disparities. The trends demonstrate our inability to attract and sustain a diverse physician workforce. The trends also suggest an inattention to the importance of this crisis, and particularly how the crisis may affect the health of underserved American communities. Overall we hope this perspective paper ignites more interest in examining race/ethnicity medical school and workforce data closely in respect to its possible connection to minority health. The decline of Black males in medical school we believe runs counter to efforts to eliminate health disparities and promote health equity and excellence in clinical care. Thus, the problem represents a crisis for American health care.
Download this graphic and share it on social media!
References
- Association of American Medical Colleges. 2015. Altering the Course, Black Males in Medicine. Washington, DC: Association of American Medical Colleges. Available at: https://store.aamc.org/altering-the-course-black-males-in-medicine.html (accessed August 25, 2020).
- Association of American Medical Colleges. 2015. 2015 State Physician Workforce Data Book. Available at: https://www.aamc.org/data-reports/workforce/report/state-physician-workforce-data-report (accessed August 25, 2020).
- Association of American Medical Colleges. 2017. Data Table A-12: Applicants, First-Time Applicants, Acceptees, and Matriculants to U.S. Medical Schools by Race/Ethnicity, 2013-2014 through 2016-2017. Available at: https://www.aamc.org/system/files/2019-10/2019_FACTS_Table_A-12.pdf (accessed August 25, 2020).
- Association of American Medical Colleges. 1992-2014 MCAT & GPA Data.
- Feroe, A. and S. Loebs. 2015. Reducing Health Disparities through the 2015 MCAT: A Bold Goal Requiring On-going Assessment, Journal of Health Disparities Research and Practice 8(1). Available at: https://digitalscholarship.unlv.edu/jhdrp/vol8/iss1/6/ (accessed August 25, 2020).
- Garces, L. M. and D. Mickey-Pabello. 2015. Racial Diversity in the Medical Profession: The Impact of Affirmative Action Bans on Underrepresented Student of Color Matriculation in Medical Schools. The Journal of Higher Education, 86(2), 264–294. https://doi.org/10.1353/jhe.2015.0009
- Laurencin, C. 2014. Diversity 5.0: A Way Forward. Journal of Racial and Ethnic Health Disparities 1(2), pp 67-68. https://doi.org/10.1007/s40615-014-0023-5
- Martin, S. A., K. Harris, and B. W. Jack. 2015. The Health of Young African American Men. JAMA 313 (14):1415-1416. https://doi.org/10.1001/jama.2015.2258
- Smedley, B. D., A. Y. Stith, L. Colburn, and C. H. Evans. 2001. The Right Thing to Do, The Smart Thing to Do: Enhancing Diversity in the Health Professions: Summary of the Symposium on Diversity in Health Professions in Honor of Herbert W. Nickens, M.D. Available at: https://www.ncbi.nlm.nih.gov/books/NBK223623/ (accessed August 25, 2020).
- Kington, R., D. Tisnado, and D. M. Carlisle. 2001. Increasing Racial and Ethnic Diversity Among Physicians: An Intervention to Address Health Disparities? In The Right Thing to Do, The Smart Thing to Do: Enhancing Diversity in the Health Professions: Summary of the Symposium on Diversity in Health Professions in Honor of Herbert W. Nickens, M.D.. Available at: https://www.ncbi.nlm.nih.gov/books/NBK223632/ (accessed August 25, 2020).
- Thomas, B., E. G. Manusov, A. Wang, and H. Livingston. 2011. Contributors of black men’s success in admission to and graduation from medical school. Academic Medicine 86(7):892–900. https://doi.org/10.1097/ACM.0b013e31821d6f3d
- Washington, H. A., R. B. Baker, O. Olakanmi, T. L. Savitt, E. A. Jacobs, E. Hoover, M. K. Wynia, and the Writing Group on the History of African Americans and the Medical Profession. 2016. Segregation, Civil Rights, and Health Disparities: The Legacy of African American Physicians and Organized Medicine, 1910-1968. Journal of the National Medical Association 101(6): 513-527. https://doi.org/10.1016/S0027-9684(15)30936-6
- Xanthos, C., H. M. Treadwell, and K. B. Holden. 2010. Social determinants of health among African–American men. JMH 7(1). Available at: http://thescholasticeditor.com/wp-content/uploads/2014/12/Xanthos-et-al-2010-1.pdf (accessed August 25, 2020).