A Model Framework That Integrates Community and Clinical Systems for the Prevention and Management of Obesity and Other Chronic Diseases
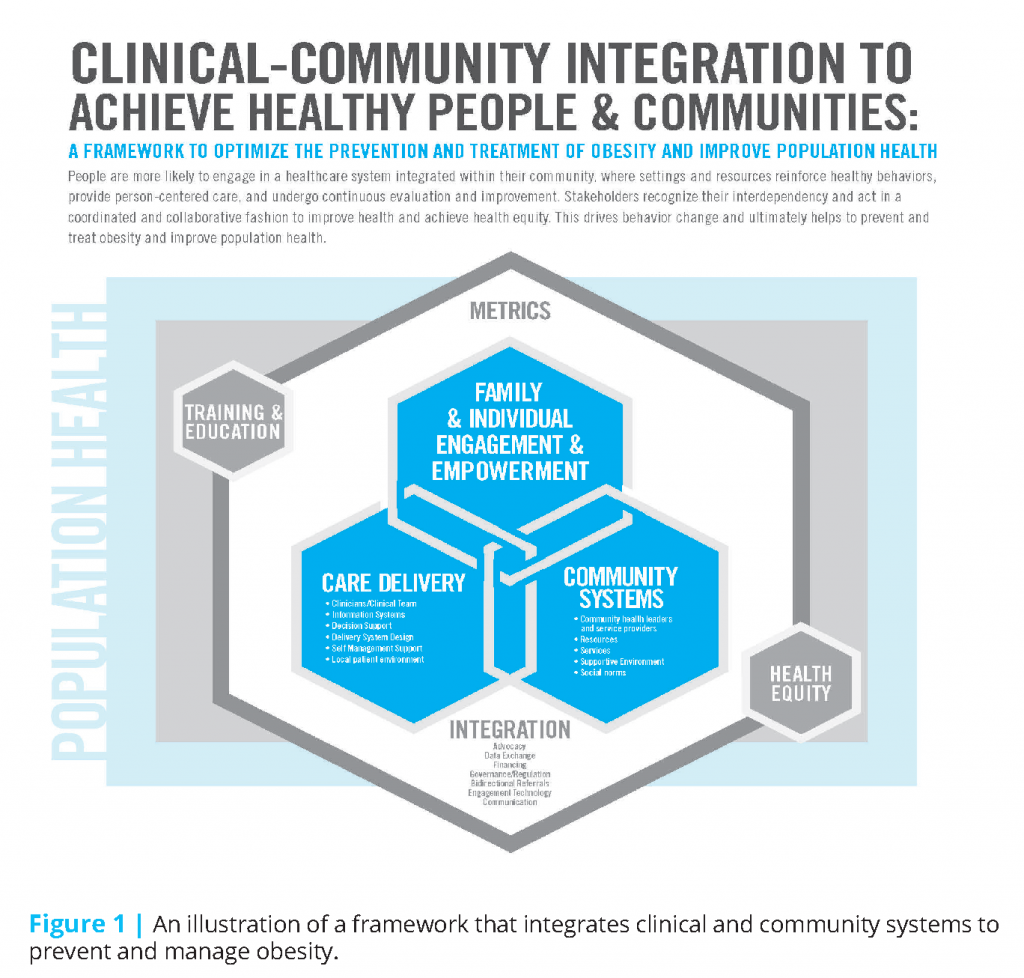
Obesity now affects 35 percent of men, 40 percent of women, and 17 percent of 2- to 19-year-old children and adolescents in the United States (Flegal et al., 2016; Ogden et al., 2016). Neither clinical nor environmental changes alone are sufficient to address a problem of this magnitude. We propose here a framework that integrates clinical and community systems to prevent and manage obesity (Figure 1) (Dietz et al., 2015).
The figure illustrates the tight linkages among family and individual engagement and empowerment, care delivery, and community systems. The tight linkages result from integrated clinical and community systems that serve to engage and empower patients and their families to optimize health outcomes. The interlocking systems influence and are influenced by the broader context of population health, where national, state, and local policies shape supportive environments and choices. Training and education are included in the outer ring because the knowledge and skill set of health care and community-based professionals determine the effectiveness of the integrated system. Health equity, also included in the outer ring, is a priority that influences all health outcomes, especially because obesity disproportionately affects ethnic minorities. Successful implementation of the model addresses health equity at every level of the framework. Success will be measured by metrics that are acceptable and agreed on by all the parties included in the model. Because integration requires partnerships and collaboration, measures should also determine the success of these interactions.
Engagement of patients and their active participation in clinical care and community systems are central to the success of this model. Engagement and activation can be prompted by individuals, their families, social networks, or providers. Changes in the design of the clinical delivery systems are required to develop a standard of care that responds with sensitivity to the bias and stigma that accompany obesity and the recognition by clinicians of the social and environmental context in which their patients’ obesity occurs. However, patients’ successful and sustained weight loss is unlikely to occur without supportive changes in the social and community systems that contributed to the development of obesity in the first place.
The integration of clinical and community systems presents a challenge. Despite the significant role of the environment in the development of the obesity epidemic, medical systems have not generally engaged with community organizations to improve access to and consumption of healthful foods or to improve the conditions that foster physical activity. Individuals or groups that can bridge clinical and community systems are known as integrators. Integrators provide essential support by convening stakeholders from community and clinical systems, building trust and new relationships, and navigating and negotiating the many challenges that accompany efforts to integrate clinical and community systems.
In this perspective, we review many of the elements and challenges associated with the integration of clinical and community systems to prevent and manage obesity. Although the focus of this perspective is on obesity, our experience suggests that a model that integrates clinical and community services has much wider applicability to other chronic diseases, such as heart disease, asthma, adverse childhood experiences, and autism spectrum disorders.
Family and Individual Power and Engagement
Family and individual empowerment and engagement are central to the success of the integrated framework (Dietz et al., 2015). If care for obesity is to succeed, persons with obesity cannot be passive recipients of care. Behavior change occurs in the context of a motivated and confident patient with social supports in place—the most critical being the family support system—to help translate health information into actionable change and restructure the environment to promote health and prevent or reverse obesity. In the patient-centered clinical care system, patient engagement includes shared decision making, which improves outcomes and reduces costs (James, 2013).
Family and individual empowerment and engagement may be characterized by an activated person who has the knowledge, skill, ability, and desire to change and is supported by the family unit. In the clinical setting, patient engagement and empowerment occur through effective communication strategies, including sensitive non-judgmental language to initiate the conversation about weight, and a caring approach to addressing a stigmatized disease. Skilled implementation of behavioral change strategies, such as motivational interviewing, attention to adult learning principles, and health literacy levels, are essential. All these empowerment and engagement strategies should occur with an understanding of the context of the life and circumstances of the person with obesity.
In an integrated system, the activated and empowered patient and family connect to community resources that support ongoing change. Engagement includes strengthening social networks to support change and environmental measures and nudges that make the healthy nutrition and physical activity choices the easy choices. Patient engagement may also include the individuals’ active involvement in advocating for public health policy and health care initiatives related to obesity.
Clinical Systems
Our framework calls for changes in health care delivery through an informed and integrated mix of care providers and practitioners who can facilitate behavior change within and beyond medical treatment and throughout the life course. As described above, clinical health care delivery should extend beyond the walls of the clinic; it must incorporate relevant information, insights, and resources from patients’ communities, households, and social circumstances. Obesity is an ideal model because the disease affects every system, and its onset and persistence are influenced by multiple community systems.
Many aspects of care delivery require reorientation to support these goals. Training and education of all members of the clinical care team in obesity medicine are essential, as well as changes in the care delivery system, such as the development of a standard of care and the decision of who should deliver that care. Obesity prevention and treatment require multiple skill sets, an approach that empowers families and individuals and addresses the social, psychosocial, emotional, and contextual dimensions of care (Ogunleye et al., 2015). Comprehensive care may require access to additional skill sets and areas of expertise, operating at multiple levels and sectors throughout the spectrum of clinical and community care delivery. Such expertise may include combinations of physicians, nurse practitioners, nurses, registered dieticians, psychologists, health coaches, exercise specialists, social workers, community health workers, care managers, and others, and it should facilitate clinical-community interaction and coordination.
Because individuals and families constantly make food and physical activity choices, the clinician’s role is to provide them with the knowledge and tools to support their self-management. Counseling techniques such as motivational interviewing can help patients set concrete action steps and behavior goals as part of a self-management plan (Onubogu et al., 2014; Resnicow et al., 2015). Collectively, information systems, decision supports, and the delivery system design support self-management by providing clinical data, identifying behavior goals, and connecting individuals with community resources.
Stigmatization of people with severe obesity is widespread, and therefore stigmatization, as both a social justice priority and an intermediary in physiological stress pathways (Puhl and Suh, 2015; Kirk and Penney, 2013) must become a priority area for care delivery systems. The care delivery team must be sensitive to the concerns and perceptions of their patients and families by using nonjudgmental terminology when describing weight (Puhl et al., 2013) and people-first language (Kyle and Puhl, 2014). Accommodation of patients with severe obesity requires changes in physical facilities, such as chairs with arms that facilitate rising to a stand, and larger gowns, examining tables, stretchers, and blood pressure cuffs; changes also require that locations be scaled to preserve privacy (Lewis et al., 2011).
A system design that builds in community engagement as a defining feature of its mission will promote the integration of medical systems with community systems (Dietz et al., 2015; Amed et al., 2015). The care provided within the health care system must incorporate knowledge of the community and complementary community systems. Awareness of the environments and contexts within which patients live, work, play, shop, pray, and commute affords opportunities to adjust clinical recommendations and link to supportive services as appropriate. For example, if increased fruit and vegetable intake for chronic disease prevention is a therapeutic target, providers and practitioners must know whether patients have access to and can afford these foods. Moreover, knowledge of community resources that may be available to the patient, such as grocery van services, accessible farmers’ markets, or meal delivery services, can proactively operationalize clinical guidance starting at the point of care. In this sense, an integrated clinical-community care delivery system would include a broader set of “vital signs” at the point of care. In addition to clinical vital signs, such as blood pressure, community vital signs, such as household food insecurity, healthful food access, and aspects of the built environment, should be readily
available to the care team to inform patient interactions and care planning. Asking about and documenting the policies and programs in patients’ workplaces or schools reinforce the systems approach to managing health.
Integration of clinical and community systems also requires open and continuous dialogue and coordination between clinical providers and community facilitators and systems. Such communication will require improvements in systematic identification and assessment of community resources and their capacity and a resolution of the barriers to dissemination and integration of relevant data within electronic health records and other point-of-care systems. Communication systems should provide for information and resource sharing and bidirectional referral systems between clinics and communities to engage and empower patients, families, and providers. Providers and health systems may need to take an active advocacy role to augment resources that strengthen and build the capacity of communities and community organizations to complement and reinforce clinical strategies. Likewise, community resources, services, and facilitators can refer individuals at high risk for adverse consequences or who require more intensive treatment to medical or other higher-level intervention settings.
Information systems should be bidirectional, provide real-time utility to the care team, and assure that data can easily flow between care delivery and community systems. Information systems must be able to retrieve and provide the most recent and pertinent information about a family or individual, as well as resources in the community, for a provider to offer the best possible interventions or guidance (Bronder et al., 2015). These systems should be able to relay this information to families, caregivers, and community partners. On the provider side, information systems must deliver high-quality, opportune, and timely decision supports—for example, messages, suggestions, and flags—so that the provider can offer both evidence-based strategies and individual- and family-centered guidance (Arsenault et al., 2014; Taveras et al., 2015).
Care delivery needs to link to community systems at the macro level, the systems level, and the individual level. For example, at the macro level, care delivery must have an overall policy and vision of community integration that drives connections with community supports and identifies a backbone for integration. At the systems level, care delivery information systems must be able to seamlessly share and receive data on health metrics, sociodemographic factors, and community resources. At the individual level, the care environment and providers can make use of mobile health technology that supports individuals and families with information to create and use health-promoting environments, goal setting, self-management strategies, and connections to community-based resources.
Community Systems
Most Americans spend only a few hours a year engaged with health care providers in care delivery settings. The rest of the time, people’s health is primarily influenced by the various community environments in which they live, work, study, play, and pray. In our framework, we use the term “community systems” to connote the various organizations and myriad economic, political, and social systems that operate at the neighborhood, municipal, statewide, and national levels to influence people’s health. This influence is brought to bear both through the services and resources available to individuals and families as well as through the environments and social norms that operate at the population level.
Our framework highlights the powerful influence these multiple community systems have on food and physical activity behaviors. Community systems can both reinforce anticipatory guidance delivered as part of primary prevention as well as support maintenance for patients who have recently received intensive behavioral counseling, weight loss surgery, or other treatments for obesity. The role of community systems to support health is often overlooked and underappreciated. Such systems could play a key role in preventing the weight regain that so commonly follows weight loss (Atkinson et al., 1994). Alternatively, community systems can work against people’s health by making healthy choices less available, affordable, and convenient and by creating social norms that reinforce unhealthy behaviors. For people being treated for obesity, gaps in community-based programs and
services or inadequate referral systems pose an additional set of barriers that limit the effectiveness and efficiency of the system overall.
Community-wide programs targeting key behaviors, such as Let’s Go! 5-2-1-0 (Rogers et al., 2013), illustrate the value of planned, intentional alignment and integration between health care providers and community systems to reinforce behaviors most strongly associated with achieving and maintaining a healthy weight. In this example, 5-2-1-0 refers to five or more fruits and vegetables a day, two hours or less of screen time, one hour or more of exercise, and zero consumption of sugary drinks. In Maine and other states that have implemented this program, health care providers, schools, and other youth-serving organizations develop and deliver consistent, mutually reinforcing messages, creating “surround sound” that can have a powerful impact on social norms. Evidence suggests that this program is associated with positive changes in food and physical activity behavior among targeted
children (Rogers et al., 2013).
In many 5-2-1-0 programs and other community-based obesity prevention efforts, health care providers have also played active roles as proponents of healthful food and physical environments (McPherson et al., 2012); for example, they advocate for safe routes to school, park and recreation programs, and school nutrition standards. This direct advocacy role played by health care providers, local health systems, and other health care organizations is a powerful, but often underutilized source of influence on community systems and an exemplar of an integrated clinic-community system of care. In policy realms often marked by controversy and divergent
and strongly held views and values, doctors, nurses, and other health care providers can be trusted and influential advocates for policy change, although only a small percentage of them report having been involved in these sorts of activities (Boyle et al., 2009).
In addition to direct advocacy, health plans and provider organizations can play a variety of other roles in an integrated system of care that spans clinical and community-based settings—by, for instance, aligning and coordinating community-based resources and services for obesity prevention and treatment, supporting multisectoral efforts that target environmental changes, build capacity for effective advocacy (2), and reinforce health-promoting social norms. Examples abound. Nemours, a children’s health system based in Delaware, has led a national effort to improve nutrition and increase the amount of physical activity children receive in early care and education settings (Nemours Foundation, 2016). Kaiser Permanente, an integrated health care system with operations in seven states and the District of Columbia, sponsors multisectoral obesity prevention collaboratives focused on policy, systems, and environmental change in more than 50 communities across the country (Dietz et al., 2015).
Integration
Individuals in communities across the country take for granted that, when needed, medical care systems and the array of nonclinical organizations and programs will work for them and may assume that they work together. Our framework addresses the optimal characteristics of medical care and community systems necessary to achieve healthy weight and prevent and treat overweight and obesity. The framework explicitly addresses an integration function that is described, on the one hand, as coordinated action by all the members of the medical care team (the health team made up of physician and nonphysician providers in the clinical care setting) and, on the other hand, as the more formalized coordination and connection between the medical care system and the community system.
Our framework calls out the integration function as a necessary component to optimize the achievement of desired health outcomes—more healthful eating, more physical activity, and healthier weight. Our framework makes clear our bias that “connecting” medical care and community systems will produce better outcomes than a parallel systems approach that optimizes each separately.
The functions of the “integrator” have been described (Hester et al., 2015). A historic legacy of mistrust is associated with clinical systems that have conducted research within communities that has rarely been of direct benefit to these communities. Among the most desired characteristics of an integrator are being a trusted individual or organization that can convene affected and interested parties and facilitate efforts that lead to common goals. These efforts include agreement that coordinated efforts can accelerate progress toward achievement of goals, the development of policies and procedures that systematize coordination of services, and the use of a performance improvement framework, such as “plan, do, study, act” (Institute for Healthcare Improvement, 2016).
The care team that formulates a plan with a patient and family to address the patient’s weight issues and appreciates the patient’s community context—that is, the availability of sources of and resources for healthful food or physical activity—will deliver better care and achieve a better outcome. The “integrator” helps connect the pieces for individuals (such as medical care, scholarships for the neighborhood-based recreation center, or farmer’s market vouchers) and for providers.
HealthPartners and the Lakeview Health Foundation have played a significant role as integrators in the PowerUp program in the St. Croix River Valley in Minnesota and Wisconsin. In addition to convening more than 100 stakeholders representing multiple sectors beyond health, organizers developed a communications strategy and an evaluation framework. The effort was funded using community benefits dollars committed for a decade (IOM, 2015; Pronk et al., 2015).
“Charting the Course,” which was launched in Dallas, Texas, in October 2012, has evolved to become the Healthy Weight Management initiative, an example of an early stage “integrator.” Healthy Weight Management is a collective-impact initiative addressing childhood obesity. Six areas of focus are supported by the Health and Wellness Alliance for Children, the backbone organization for Healthy Weight Management (3) and reflect the integration of medical care and community systems. The six focus areas are healthy eating, a supportive health care system, physical activity, early childhood, healthy school settings, and breastfeeding. This effort was initially supported by the United Way of Dallas but has been largely underwritten by Children’s Health in Dallas.
Community-centered health homes (Cantor et al., 2011) and the recently described Accountable Health Communities (Alley et al., 2016) provide additional examples and opportunities to take from concept to practice at scale the integrator idea with a funding mechanism and a framework for the accountability of participants.
Training and Education
Successful implementation of the integrated framework will require many health professionals to assimilate emerging science and skills related to obesity, adopt a population-based care delivery approach, and learn to work together as an interprofessional team. Traditional health education has focused on care for the individual, characterized by isolated provider-patient interactions, with little attention given to the role of nutrition and physical activity. A recent report by the Alliance for a Healthier Generation, the American College of Sports Medicine, and the Bipartisan Policy Center (2014) documented the lack of physician training at all levels in nutrition and activity and reported that only 25 percent of physicians think they received adequate education in counseling on diet or physical activity. In addition, as scientific knowledge about the physiology, etiologies, and treatment of obesity continue to emerge, most health professionals remain relatively unaware of the relationship of obesity to social determinants of health, neurohormonal control of weight, epigenetics, the microbiome, social factors such as stigma and bias, and adverse childhood events (Bleich et al., 2012; Colbert and Jangi, 2013; Ochner et al., 2015).
Beyond the lack of current knowledge, most health professions have been trained to focus on individual patients within the confines of the clinical setting. However, health care itself accounts for 10–20 percent of health or the prevention of premature death (Schroeder, 2007). The integrated framework will require a health workforce that understands and can impact the social and behavioral determinants of health. Federal agencies, including the Centers for Disease Control and Prevention and the Health Resources and Services Administration, have recognized the need for health professionals accomplished in these competencies, as have both governmental and private payers. Value-based payment models, such as accountable care organizations and accountable health communities, are incentivizing a rapid increase in community-clinical integration health competencies (4, 5, 6, 7).
Finally, to operationalize an integrated framework, health professionals will need to work as an interprofessional team that recognizes and utilizes the skills unique to each provider sector, shares a common set of competencies for obesity and its related conditions, and learns and practices interprofessional collaboration skills (Barr, 1998). The clinical-community care team will need to include community-based stakeholders (e.g., community health workers) who share the common and interprofessional collaboration competencies.
While we recognize the need and value of our current health care system, in the integrated framework we recommend a training and education paradigm shift from an individual, clinically focused model limited to a health care setting to a patient- and family-centered model that is community-focused and that addresses the social, behavioral, and environmental determinants of health.
Population Health
As indicated by its location, the framework is embedded within a population health context. Factors related to population health include legislative or regulatory policies at the federal and state level. These policies include such initiatives as the Healthy, Hunger-Free Kids Act, which substantially improved the foods served in schools. Such policies may not originate within communities, but they do directly affect community ecosystems.
Federal and state policies also affect care delivery. For example, the Patient Protection and Affordable Care Act offers the option to expand Medicaid to more low-income adults, making preventive obesity screening for children and adults available at no additional out-of-pocket cost to patients or parents. Because obesity screening meets U.S. Preventive Services Task Force recommendations, obesity counseling and behavioral management, including referrals, are covered services. Furthermore, as Medicaid and Medicare shift from volume-based to value-based care, clinical systems will be incentivized to identify nonclinical, evidence-based, community interventions that improve nutrition and physical activity and prevent or stabilize obesity and other chronic conditions for patients and their families. The Affordable Care Act includes provisions related to community health needs assessments and community benefits, which mandate that nonprofit hospitals invest in community health improvement activities (Rosenbaum et al., 2015). Community benefit initiatives provide another potential source of funding to integrate care delivery and community organizations.
Equity
As we indicated in our Health Affairs article titled “An Integrated Framework for the Prevention and Treatment of Obesity and Its Related Chronic Diseases,” we define health equity as “the assurance of the conditions for optimal health for all people” (Dietz et al., 2015). We intentionally located health equity in the ring that surrounds the model to give health equity an explicit overarching priority. Inequities characterize obesity. The prevalence of obesity and severe obesity is greater among African American women than other population groups (Flegal et al., 2016). Children of color have higher obesity and overweight rates than their white counterparts (Ogden et al., 2016). In addition, individuals with obesity are highly stigmatized, and their medical care is adversely affected. For example, providers spend less time with patients with obesity (Bertakis and Azari, 2005; Hebl and Xu, 2001), and almost 70 percent of women with severe obesity report that negative experiences with providers have led them to defer or avoid medical visits.
Health equity must be a priority in clinical delivery and community systems. We indicate the importance of health equity in training and education by locating both in the outer ring of the model because improved training and cultural competency on the part of providers will begin to address the inequities in care. Training and education should begin with a sensitivity to bias and stigma among patients with obesity, including appropriate terms to use during clinical encounters (Wadden and Didie, 2003). Furthermore, recognition of the environmental conditions that promote obesity or limit the patient’s ability to increase physical activity or improve dietary choices must become an essential element of the clinical encounter.
Inequities also characterize many communities of color. The absence of supermarkets may limit the availability of healthful foods. Communities that lack sidewalks or are characterized by the lack of connections of sidewalks to places where people want to go, in addition to the absence of parks and recreational facilities, may limit opportunities for physical activity. Unless the provider considers the environmental context of obesity, counseling efforts are likely to lead to frustration for both the provider and patient.
Employers and Health Plans
Although they are not explicitly included in the model, employers and health plans can play a major role in the integration of community and clinical systems. Employers can specify the types of services for their employees that they require of their employee health plans and can advocate and support community systems that contribute to the health of their workforce. Health plans can also effect changes in the care delivery system and increasingly recognize that investments in community systems may reduce the prevalence and improve outcomes of chronic disease management.
Metrics
Measuring the implementation and impact of the integrated framework will be a challenge, in part because so many metrics are being used by diverse stakeholders. Nonetheless, collaborating partners need to agree on a limited set of timely, accurate, credible, and reproducible measures that reflect progress toward stakeholder goals, whether to assess process, infrastructure development, or health outcomes.
At the population level, the Institute of Medicine’s consensus report titled Vital Signs: Core Metrics for Health and Health Care Progress (IOM, 2015) recommended using overweight/obesity priority measures—such as activity levels and healthy eating behaviors—as well as a range of other measures relevant to the health of a community to track the impact of obesity prevention and treatment efforts. At a more granular level, another Institute of Medicine report (IOM, 2013) identified outcome (e.g., age and pregnancy-specific body mass index goals) as well as process (e.g., physical activity/day guidelines), policy, and structural (e.g., enhanced physical and built environment) metrics for each of the five goals identified in Accelerating Progress in Obesity Prevention (IOM, 2012). Those five goals included: Integrating physical activity every day in every way; making healthy foods available everywhere; marketing what matters for a healthy life; activating employers and health care professionals; and strengthening schools as the heart of health. The integrated framework also calls for metrics to measure the integration and collaboration among clinical and community stakeholders. A number of metrics exist (8), although at present no consensus exists on the measures that correlate best with the relevant process or outcome goals, nor are there generally resources available to regularly collect local level data around these goals.
Summary
We have developed a new model for integrating clinical and community services for the prevention and treatment of obesity that offers clinicians, public health practitioners, and community organizations a new conceptualization of how care for obesity and other chronic diseases can be managed or the conditions prevented. The model calls for a variety of changes in how various care providers will need to interact with each other and community systems to prevent and treat obesity. Success will depend on the ability of providers to work with and strengthen clinical systems, new metrics to access the initial success of collaborations and ultimately improved outcomes, and new payment models that recognize and return the cost savings attributable to community systems to community organizations. The high prevalence of obesity and the current limited reach of clinical interventions emphasize the urgency to implement this model.
Notes
- The authors are members of the activities of the Innovation Collaborative for the Integration of Clinical and Social Systems for the Prevention and Management of Obesity, an ad hoc activity associated with the Roundtable on Obesity Solutions of the National Academies of Sciences, Engineering, and Medicine.
- See www.voicesforhealthykids.org (accessed August 19, 2016).
- See www.healthandwellnessalliance.com (accessed August 22, 2016).
- See Public Health 3.0, https://www.healthypeople.gov/sites/default/files/Public-Health-3.0-White-Paper.pdf (accessed August 22, 2016).
- See Accountable Health Communities Model, https://innovation.cms.gov/initiatives/AHCM, https://www.cms.gov/Newsroom/MediaReleaseDatabase/Fact-sheets/2016-Fact-sheetsitems/2016-01-05.html
(accessed August 22, 2016). - See What’s the Quality Payment Program? https://www.cms.gov/Medicare/Quality-Initiatives-PatientAssessment-Instruments/Value-Based-Programs/MACRA-MIPS-and-APMs/MACRA-MIPS-and-APMs.html (accessed August 22, 2016).
- See Medicare Payment Reform: Aligning Incentives for Better Care, http://www.commonwealthfund.org/publications/issue-briefs/2015/jun/medicarepayment-reform-aligning-incentives (accessed August
22, 2016). - See Tools for Measuring Collaboration, http://broadleafconsulting.ca/uploads/3/4/0/8/3408103/tools_for_measuring_collaboration.pdf (accessed August 5, 2016).
References
- Alley, D. E., C. N. Asomugha, P. H. Conway, and D. M. Sanghavi. 2016. Accountable health communities: Addressing social needs through Medicare and Medicaid. New England Journal of Medicine 374(1):8–11. https://doi.org/10.1056/NEJMp1512532
- Alliance for a Healthier Generation, American College of Sports Medicine, and Bipartisan Policy Center. 2014. Teaching nutrition and physical activity in medical school: Training doctors for prevention-oriented care. Available at: http://cdn.bipartisanpolicy.org/wp-content/uploads/sites/default/files/Med_Ed_Report.PDF (accessed July 24, 2016).
- Amed, S., P. J. Naylor, S. Pinkney, S. Shea, L. C. Mâsse, S. Berg, J. P. Collet, and J. Wharf Higgins. 2015. Creating a collective impact on childhood obesity: Lessons from the SCOPE initiative. Canadian Journal of Public Health 106(6):e426–433. https://doi.org/10.17269/cjph.106.5114
- Arsenault, L. N., K. Xu, E. M. Taveras, and K. A. Hacker. 2014. Parents’ obesity-related behavior and confidence to support behavioral change in their obese child: Data from the STAR study. Academic Pediatrics 14(5):456–462. https://doi.org/10.1016/j.acap.2014.03.001
- Atkinson, R. L., W. H. Dietz, J. P. Foreyt, N. J. Goodwin, J. O. Hill, J. Hirsch, X. Pi-Sunyer, R. L. Weinsier, R. Wing, J. H. Hoofnagle, J. Everhart, V. S. Hubbard, and S. Zelitch. 1994. Weight cycling. JAMA 272(15):1196–1202. Available at: https://pubmed.ncbi.nlm.nih.gov/7741844/ (accessed August 10, 2020).
- Barr, H. 1998. Competent to collaborate: Towards a competency-based model for interprofessional education. Journal of Interprofessional Care 12(2):181–187. https://doi.org/10.3109/13561829809014104
- Bertakis, K. D., and R. Azari. 2005. The impact of obesity on primary care visits. Obesity Research 13(9):1615–1622. https://doi.org/10.1038/oby.2005.198
- Bleich, S. N., W. L. Bennett, K. A. Gudzune, and L. A. Cooper. 2012. National survey of US primary care physicians’ perspectives about causes of obesity and solutions to improve care. BMJ Open 2(6):e001871. Available at: https://bmjopen.bmj.com/content/bmjopen/2/6/e001871.full.pdf (accessed August 10, 2020).
- Boyle, M., S. Lawrence, L. Schwarte, S. Samuels, and W. J. McCarthy. 2009. Health care providers’ perceived role in changing environments to promote healthy eating and physical activity: Baseline findings from health care providers participating in the healthy eating, active communities program. Pediatrics 123(suppl 5):S293–300. https://doi.org/10.1542/peds.2008-2780H
- Bronder, K. L., C. A. Dooyema, S. J. Onufrak, and J. L. Foltz. 2015. Electronic health records to support obesity-related patient care: Results from a survey of United States physicians. Preventive Medicine 77:41–47. https://doi.org/ 10.1016/j.ypmed.2015.04.018
- Cantor, J., L. Cohen, L. Mikkelsen, R. Panares, J. Srikantharajah, and E. Valdovinos. 2011. Community-centered health homes: Bridging the gap between health services and community prevention. Oakland, CA: Prevention Institute. Available at: https://www.preventioninstitute.org/publications/community-centered-health-homes-bridging-the-gap-between-health-services-and-community-prevention (accessed August 10, 2020).
- Colbert, J. A. and S. Jangi. 2013. Training physicians to manage obesity—back to the drawing board. New England Journal of Medicine 369(15):1389-1391. https://doi.org/10.1056/NEJMp1306460
- Dietz, W. H., L. S. Solomon, N. Pronk, S. K. Ziegenhorn, M. Standish, M. M. Longjohn, D. D. Fukuzawa, I. U. Eneli, L. Loy, N. D. Muth, E. J. Sanchez, J. Bogard, and D. W. Bradley. 2015. An integrated framework for the prevention and treatment of obesity and its related chronic diseases. Health Affairs (Millwood) 34(9):1456–1463. https://doi.org/10.1377/hlthaff.2015.0371
- Flegal, K. M., D. Kruszon-Moran, M. D. Carroll, C. D. Fryar, and C. L. Ogden. 2016. Trends in obesity among adults in the United States, 2005–2014. JAMA 315(21):2284–2291. https://doi.org/10.1001/jama.2016.6458
- Hebl, M. R., and J. Xu. 2001. Weighing the care: Physicians’ reactions to the size of a patient. International Journal of Obesity 25:1246–1252. https://doi.org/10.1038/sj.ijo.0801681
- Hester, J. A., P. V. Stange, L. C. Seeff, J. B. Davis, and C. A. Craft 2015. Toward sustainable improvements in population health: Overview of community integration structures and emerging innovations in financing. CDC Health Policy Series, No. 2. Atlanta, GA: CDC. Available at: https://stacks.cdc.gov/view/cdc/27844 (accessed August 10, 2020).
- Institute for Healthcare Improvement. 2016. How to improve. Available at: http://www.ihi.org/resources/Pages/HowtoImprove/default.aspx (accessed July 29, 2016).
- Institute of Medicine. 2012. Accelerating Progress in Obesity Prevention: Solving the Weight of the Nation. Washington, DC: The National Academies Press. https://doi.org/10.17226/13275
- Institute of Medicine. 2015. Cross-Sector Responses to Obesity: Models for Change: Workshop Summary. Washington, DC: The National Academies Press. https://doi.org/10.17226/21706
- Institute of Medicine. 2013. Evaluating Obesity Prevention Efforts: A Plan for Measuring Progress. Washington, DC: The National Academies Press. https://doi.org/10.17226/18334
- Institute of Medicine. 2015. Vital Signs: Core Metrics for Health and Health Care Progress. Washington, DC: The National Academies Press. https://doi.org/10.17226/19402
- James, J. 2013. Health policy brief: Patient engagement. Available at: http://www.healthaffairs.org/healthpolicybriefs/brief.php?brief_id=86 (accessed June 5, 2016).
- Kirk, S. F., and T. L. Penney. 2013. The role of health systems in obesity management and prevention: Problems and paradigm shifts. Current Obesity Reports 2:315–319. https://doi.org/10.1007/s13679-013-0074-7
- Kyle, T. K., and R. M. Puhl. 2014. Putting people first in obesity. Obesity (Silver Spring) 22(5):1211. https://doi.org/10.1002/oby.20727
- Lewis, S., S. L. Thomas, R. W. Blood, D. J. Castle, J. Hyde, and P. A. Komesaroff. 2011. How do obese individuals perceive and respond to the different types of obesity stigma that they encounter in their daily lives? A qualitative study. Social Sciences and Medicine 73(9):1349–1356. https://doi.org/10.1016/j.socscimed.2011.08.021
- McPherson, M. E., R. Mirkin, P. N. Heatherley, and C. J. Homer. 2012. Educating health care professionals in advocacy for childhood obesity prevention in their communities: Integrating public health and primary
care in the Be Our Voice project. American Journal of Public Health 102(8):e37–43. https://doi.org/10.2105/AJPH.2012.300833 - Nemours Foundation. Collaboration and the ECELC project. 2016. Available at: https://healthykidshealthyfuture.org/about-ecelc/ (accessed June 17, 2016).
- Ochner, C. N., A. G. Tsai, R. F. Kushner, and T. A. Wadden. 2015. Treating obesity seriously: when recommendations for lifestyle change confront biological adaptations. Lancet Diabetes and Endocrinology 3(4):232-234. https://doi.org/10.1016/S2213-8587(15)00009-1
- Ogden, C. L., M. D. Carroll, H. G. Lawman, C. D. Fryar, D. Kruszon-Moran, B. K. Kit, and K. M. Flegal. 2016. Trends in obesity prevalence among children and adolescents in the United States, 1988–1994 through 2013–2014. JAMA 315 (21):2292–2299. https://doi.org/10.1001/jama.2016.6361
- Ogunleye, A., A. Osunlana, J. Asselin, A. Cave, A. M. Sharma, and D. L. Campbell-Scherer. 2015. The 5As team intervention: Bridging the knowledge gap in obesity management among primary care practitioners. BMC Research Notes 8:810. https://doi.org/10.1186/s13104-015-1685-8
- Onubogu, U., M. E. Graham, and T. O. Robinson. 2014. Pilot study of an action plan intervention for self-management in overweight/obese adults in a medically underserved minority population: Phase 1. ABNF Journal 25(3):64–71. Available at: https://europepmc.org/article/med/25181784 (accessed August 10, 2020).
- Pronk, N. P., M. Canterbury, T. E. Kottke, and D. Zimmerman. 2015. Case study: The power of community in population health: PowerUp for Kids. In Population health: Creating a culture of wellness, 2nd ed., edited by D. B. Nash, R. J. Fabius, A. Skoufalos, J. L. Clarke, and M. R. Horowitz. Burlington, MA: Jones and Bartlett Learning. Pp. 427-436.
- Puhl, R., J. L. Peterson, and J. Luedicke. 2013. Motivating or stigmatizing? Public perceptions of weight-related language used by health providers. International Journal of Obesity (London) 37(4):612–619. https://doi.org/10.1038/ijo.2012.110
- Puhl, R., and Y. Suh. 2015. Health consequences of weight stigma: Implications for obesity prevention and treatment. Current Obesity Reports 4(2):182–190. https://doi.org/10.1007/s13679-015-0153-z
- Resnicow, K., F. McMaster, A. Bocian, D. Harris, Y. Zhou, L. Snetselaar, R. Schwartz, E. Myers, J. Gotlieb, J. Foster, D. Hollinger, K. Smith, S. Woolford, D. Mueller, and R. C. Wasserman. 2015. Motivational interviewing and dietary counseling for obesity in primary care: An RCT. Pediatrics 135(4):649–657. https://doi.org/10.1542/peds.2014-1880
- Rogers, V. W., P. H. Hart, E. Motyka, E. N. Rines, J. Vine, and D. A. Deatrick. 2013. Impact of Let’s Go! 5-2-1-0: A community-based, multisetting childhood obesity prevention program. Journal of Pediatric Psychology
38(9):1010–1020. https://doi.org/10.1093/jpepsy/jst057 - Rosenbaum, S., D. A. Kindig, J. Bao, M. K. Byrnes, and C. O’Laughlin. 2015. The value of the nonprofit hospital tax exemption was $24.6 billion in 2011. Health Affairs (Millwood) 34(7):1225–1233. https://doi.org/10.1377/hlthaff.2014.1424
- Schroeder, S. A. 2007. We can do better: Improving the health of the American people. New England Journal of Medicine 357(12):1221–1228. https://doi.org/10.1056/NEJMsa073350
- Taveras, E. M., R. Marshall, K. P. Kleinman, M. W. Gillman, K. Hacker, C. M. Horan, R. L. Smith, S. Price, M. Sharifi, S. L. Rifas-Shiman, and S. R. Simon. 2015. Comparative effectiveness of childhood obesity interventions in pediatric primary care: A cluster-randomized clinical trial. JAMA Pediatrics 169(6):535–542. https://doi.org/10.1001/jamapediatrics.2015.0182
- Wadden, T. A., and E. Didie. 2003. What’s in a name? Patients’ preferred terms for describing obesity. Obesity Research 11(9):1140–1146. https://doi.org/10.1038/oby.2003.155