Workforce Development to Enhance the Cognitive, Affective, and Behavioral Health of Children and Youth: Opportunities and Barriers in Child Health Care Training
Responsibility for cognitive, affective, and behavioral (CAB) health of children and adolescents (hereafter “youth”) has traditionally been shared among families, education systems, communities, and the health care delivery system. Within routine child health care, increasing but spotty attention is paid to early cognitive, emotional, and behavioral development. Those most intensively trained in emotional development and the clinical behavioral sciences (e.g., child and adolescent psychiatrists and psychologists, behavioral and developmental pediatricians, and social workers) have historically been segmented from routine child health care. Roles of behavioral clinicians have focused largely on treating those who have troublesome or disabling CAB disorders. Relatively less attention has been paid by any segment of the health care field to CAB health promotion and disorder prevention, starting early in life, or even to early detection and intervention for behavioral problems of youth who do not meet diagnostic criteria (NRC and IOM, 2009b). Much of the innovation in this area has been carried out by prevention scientists who have created evidence-based interventions, primarily targeting activities in community settings, and has not focused on opportunities within primary or subspecialty child health care settings. Preventive interventions adapted for child health care settings and training programs are nascent and will require a revision of training goals and curricula as well as a reorganization of practice for successful implementation.
Why Focus on Children’s Cognitive, Affective, and Behavioral Health?
Childhood mental health diagnoses are increasing in absolute numbers as well as in proportion to the total childhood population (IOM, 2015b). Estimates are that 13-20 percent of youth ages 3-17 in the United States experience a mental health disorder in any given year (NRC and IOM, 2009b); these estimates do not take into account youth with autism spectrum and cognitive disorders or sub-threshold CAB symptoms. An increased prevalence of diagnosed childhood CAB disorders is adding to the care and cost burden for children at an alarming rate (AHRQ, 2014). Mental health disorders negatively affect youth outcomes; research estimates that 50 percent of high school students with mental health disorders drop out of school (NAMI, n.d.). Particularly alarming are the increasing rates of psychotropic medication use and hospitalization among youth (Perou et al., 2013). A recent 2013 report by the Centers for Disease Control and Prevention (CDC) estimated the costs of behavioral disorders in youth to be approximately $247 billion per year when including health, educational, juvenile justice, and employee productivity costs (Perou et al., 2013). Medicaid data from the first decade of the 2000s documented a rate of increase that more than doubled reimbursed services for behavioral disorders of 3- through 17-year-old youth (IOM, 2015b).
Furthermore, CAB disorders in youth frequently become disabling disorders in adults; in fact, 50 percent of lifetime cases of mental health disorders begin by age 14, and 75 percent begin by age 24 (NRC and IOM, 2009b). It is also recognized that over their lifetime youth with CAB disorders are more vulnerable to risky or negligent health-related behaviors and consequent physical health disorders (Felitti et al., 1998; Kessler and Wang, 2008). The opportunity to mitigate risk for lifetime behavioral and related physical health conditions is likely to be greatest for young people, particularly in the first 3-5 years of life (Shonkoff and Garner, 2012; Shonkoff et al., 2009).
Risks for disadvantageous CAB outcomes include family disruption, child abuse and neglect, exposure to violence, food insecurity, unsafe housing, and many other adverse early childhood experiences (Bitsko et al., 2016; Shonkoff et al., 2009)—all of which lead to unmitigated stress. The adverse CAB and physical health outcomes of early childhood risks, especially the negative impact of multiple early adverse experiences, are now well documented (Bethell et al., 2014; Jimenez et al., 2016). In addition, such common childhood experiences as sleep deprivation, nutritional deficits (e.g., iron deficiency), and excessive screen time are generally recognized risk factors for disadvantageous CAB development (NRC and IOM, 2009b). Finally, chronic disease in childhood is a frequent and too often underappreciated risk factor for suboptimal development of CAB potential (Pless and Roghmann, 1971). All of these concerns can be addressed by the medical care system if properly organized to provide and promote family-focused, children’s CAB health and preventive interventions in the early years.
Why Should Health Care be a Preferred Venue for CAB Health Promotion and What Are Obstacles to Implementation?
Child health primary care provided in pediatric and family practice settings hold great promise for improving CAB outcomes. A majority of children, estimated at 90 percent, are seen with their parents in primary care settings on multiple occasions in the first several years of life, providing uniquely broad access and opportunity (CDC, 2016). Child health care and health care providers are trusted by most families (Graber, 2012). Anticipatory guidance, a standard component of child health care during the frequent primary care visits in the first years of life (Dosman et al., 2012), demonstrates that within this setting there is the ability to address parenting practices that could better support healthy CAB development. Several universal programs to mitigate risk —for instance, Reach Out and Read (ROR) and the Video Interaction Project (VIP), which targets cognitive development Mendelsohn et al., 2007; Needlman et al., 2005)—have been widely incorporated into primary care clinical and training programs. Other programs, such as Incredible Years, have improved CAB outcomes when studied in primary care settings (Perrin et al., 2014). Healthy Steps has also been incorporated into dozens of practices across the country (Briggs, 2016; IOM and NRC, 2014).
In addition, screening for autism spectrum disorders or adolescent depression is increasingly being incorporated into pediatric practices (Cheung et al., 2007; Committee on Children With Disabilities, 2001; Robins, 2008). Screening mothers for their adverse experiences as a proxy to address their parenting skills and providing parenting support through the Healthy Steps program have been shown in the Montefiore ambulatory health care system in the Bronx to improve social-emotional development in children (Briggs et al., 2014). Assessing mothers for depression, which is a risk for children’s CAB health (NRC and IOM, 2009a), has become a more common practice in primary child health care, and there is now an allowable charge by some state Medicaid programs.
A recent paper published by Stein et al., however, demonstrated little change in primary care pediatricians’ skill set and comfort level with common CAB concerns outside of attention-deficit/hyperactivity disorder (Stein et al., 2016). It is imperative to improve the skills and engagement of physicians who provide primary child health care through training focused on important CAB pediatric health outcomes.
Furthermore, the movement to accountable care, consequent to the Patient Protection and Affordable Care Act (ACA), has incentivized new models of health care that affect both measurement and delivery approaches, including the use of team-based approaches. The establishment of accountable care organizations (ACOs) is a key feature of the ACA and is designed to replace the fragmented and uncoordinated care system with one that integrates care with payment incentives targeting individual and population health outcomes (Fisher et al., 2007) and with team-based approaches that require the blended expertise of multiple providers (IOM, 2015c). Consequently, integrating other health professionals who can address CAB health at early ages into primary care settings for children where children are frequently evaluated is a critical new development that emphasizes the need to organize training to promote acceptance of team-based care.
Primary health care is not the only medical setting for enhancing children’s CAB health. Disabling chronic disorders, which occur in an estimated 4-8 percent of youth (NASEM, 2015; Newacheck and Halfon, 1998), are diagnosed and treated largely in subspecialty medical care settings but with variable attention to the crippling behavioral dimensions of their disease. These children are at risk for cognitive and behavioral issues related to their primary condition or stemming from treatments, including medical traumatic stress (Kazak et al., 2006). Disrupted school engagement, anxiety, depression, and substance use are frequent (Hadland and Walker, 2016). Behavioral consequences and traumatic stress also accrue to parents and other family members (Kazak et al., 2004; NASEM, 2016). For example, a recent international survey of parents of recently diagnosed patients with cystic fibrosis found a 30-40 percent prevalence of anxiety and /or depression (Quittner et al., 2015). In comprehensive chronic care programs, pediatric psychologists or behaviorally oriented social workers are embedded in the chronic care team, a practice that considerably antedates integrated primary health care. Nevertheless, programs may vary in the degree to which trainees from participating health care disciplines are required to work with these behavioral health professionals to provide proactive and preventive behavioral care across the physical and behavioral health spectrum (IOM, 2015a). Though family disturbance is a contributor to poor CAB outcomes, wellness of the families who provide care for children with chronic diseases is often unaddressed.
In the future, the ability of health care professionals to create effective integrated, interprofessional chronic care teams that promote children’s CAB health as well as advocate for diagnosis and treatment of behavioral disorders will be important for training. Yet, there is no requirement for either training in this mode or achievement of basic competency in CAB health promotion by trainees in health professions that contribute to subspecialty team care. An exception may be training in pediatric psychology, wherein trainees are expected to attend to the full continuum from healthy growth and development, procedural distress and medication adherence, family adjustment, and diagnosis and treatment of behavioral health conditions. Increasingly, primary care physicians and nurse practitioners as participants in patient-centered medical homes also contribute to the care of children with chronic diseases. Their training must also provide experience with children with such chronic diseases as asthma and their families (Kolko and Perrin, 2014).
Without immediate and sustained attention to developing a health care workforce ready to partner around CAB health promotion and prevention as well as treatment, the costs of mental health care will continue to adversely impact our nation. That workforce must include all health professionals who serve children and families and must promote interdisciplinary, family-centric, community-linked, team-based methods for service provision.
The Status of Health Care Workforce and Workforce Training that Addresses Improvement of CAB Outcomes
At a macro-level, there appears to be an adequate number of pediatricians, family medicine physicians, pediatric psychologists, nurse practitioners, and social workers who, if appropriately trained, can populate efforts in health care that advance children’s CAB outcomes. Numbers of child and adolescent psychiatrists and developmental and behavioral pediatricians, on the other hand, are insufficient to participate in broader efforts beyond their current focus on diagnosing and treating children with behavioral disorders (AACAP, 2016). Filling immediate needs for behavioral expertise appears to fall largely on the shoulders of nonphysician behaviorally trained health professionals. Estimates of mental health professionals in the United States determined that 96 percent of counties had an unmet need for prescribing professionals and 18 percent had an unmet need for non-prescribing mental health professionals (Konrad et al., 2009). The latter gap was attributed to uneven distribution. Rural and low-income populations are less well served by mental health professionals, even though they represent populations of high need (Ricketts, 2005). Filling this gap may require participation by a broader array of behavioral health care disciplines as well as the use of telemedicine to provide greater coverage. Greater
participation by primary care and subspecialty physicians (who, if adequately trained and supported by appropriate psychiatric consultation as needed, can be prescribing mental health professionals), nurse practitioners, and social workers is needed. Creating an ideal workforce is a threefold challenge: to train health professionals in sufficient numbers to fill current and future needs; to focus training on preventive and promotive (rather than only diagnostic and treatment) practices; and to set expectations for achievement of specific competencies in training that cross all disciplines in the interests of promoting CAB health (Skillman et al., 2016; Annapolis Coalition on the Behavioral Health Workforce, 2007).
Symptom-focused training is still predominant in child health care settings. It will continue to be so because the expanding body of knowledge is challenging to master, and disease is far from eradicated. Even though there is increasing recognition of adverse effects of behavioral disorders on physical health, care settings are not organized to address behavioral health promotion and prevention needs. Medical and behavioral health care training have traditionally been provided in separate venues. In addition, child health care, whether in the primary care or the subspecialty setting, may focus on the child to the exclusion of parents, at a time when multigenerational, family-focused medical and preventive interventions are likely to be the most effective. Importantly, characteristics of current child health care are driven or reinforced by reimbursement systems—which at this time largely pay for discreet provider encounters to diagnose or treat specific conditions rather than for integrated, anticipatory care or consultations among professionals. In systems where insurance has been siloed for medical versus behavioral health claims, cost savings for promotion and prevention have not been recognizable. Other impediments include lack of standardized childhood outcome measures for behavioral health promotion and behavioral disorder prevention and for judging competence of trainees in these areas.
Obstacles to achieving a training experience that will prepare health care professionals to foster child CAB development and health are numerous and formidable. They include insufficient numbers of well-prepared educators; lack of integrated, interprofessional training opportunities; practice facilities and organization that do not easily accommodate team practice; and certification and accreditation expectations that do not address behavioral health in general or multigenerational, family-focused CAB health promotion or prevention. Other major obstacles include compensation of care models that do not support interprofessional preventive care training and a resulting lack of institutional (hospital) support for preventive care. These obstacles can be overcome if there is a mandate from standard-setting bodies (e.g., certifying boards or program accreditation bodies, professional societies, health care systems and organizations, and policy makers) to train health care providers in team-based care in order to promote CAB health—and to reimburse these providers appropriately for that work.
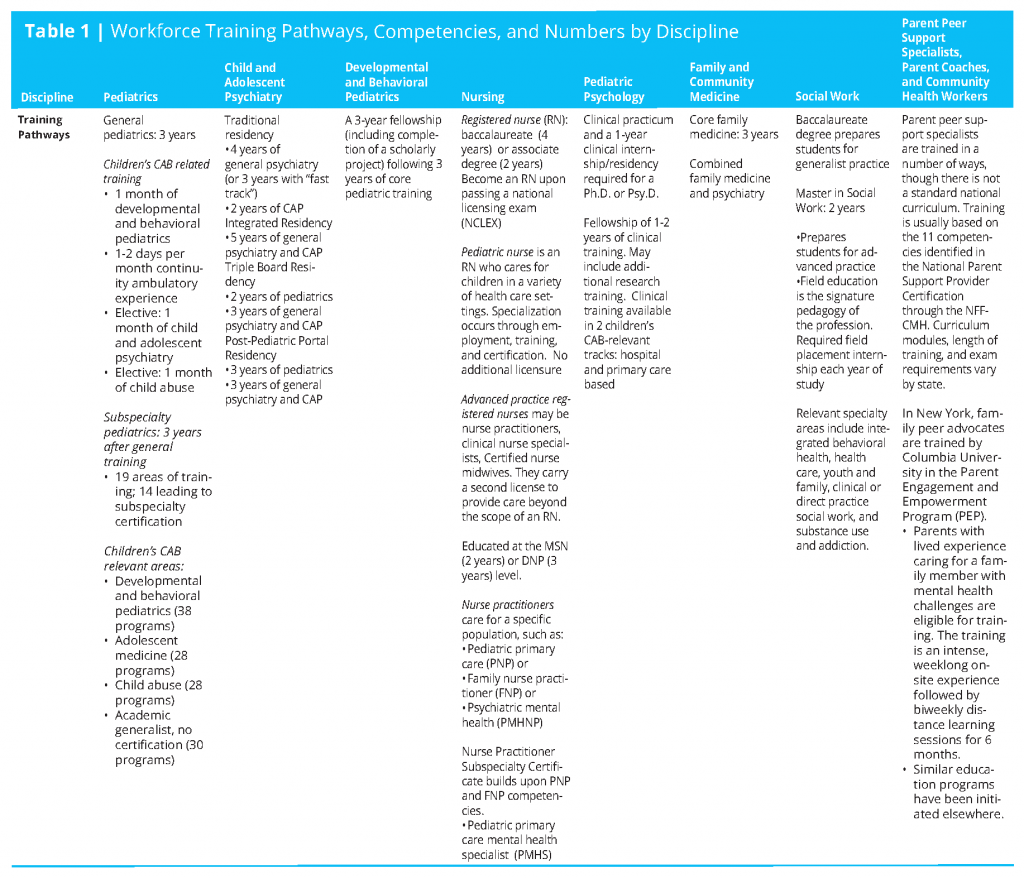
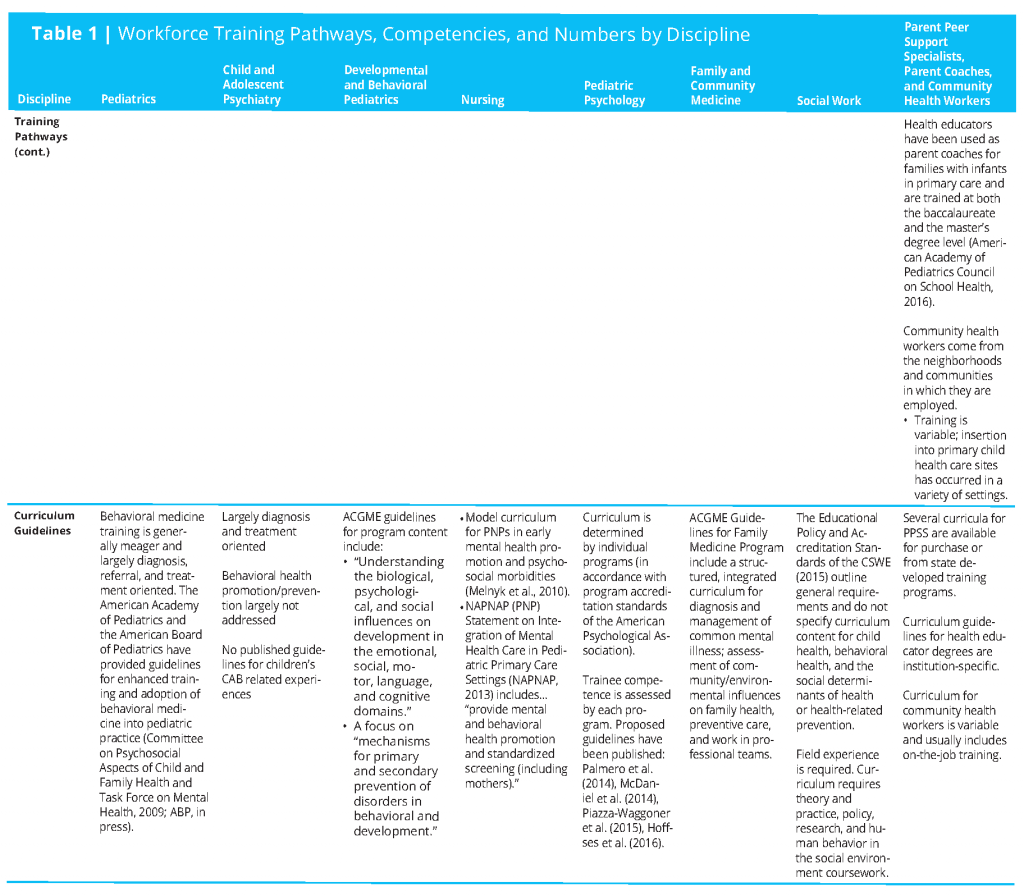
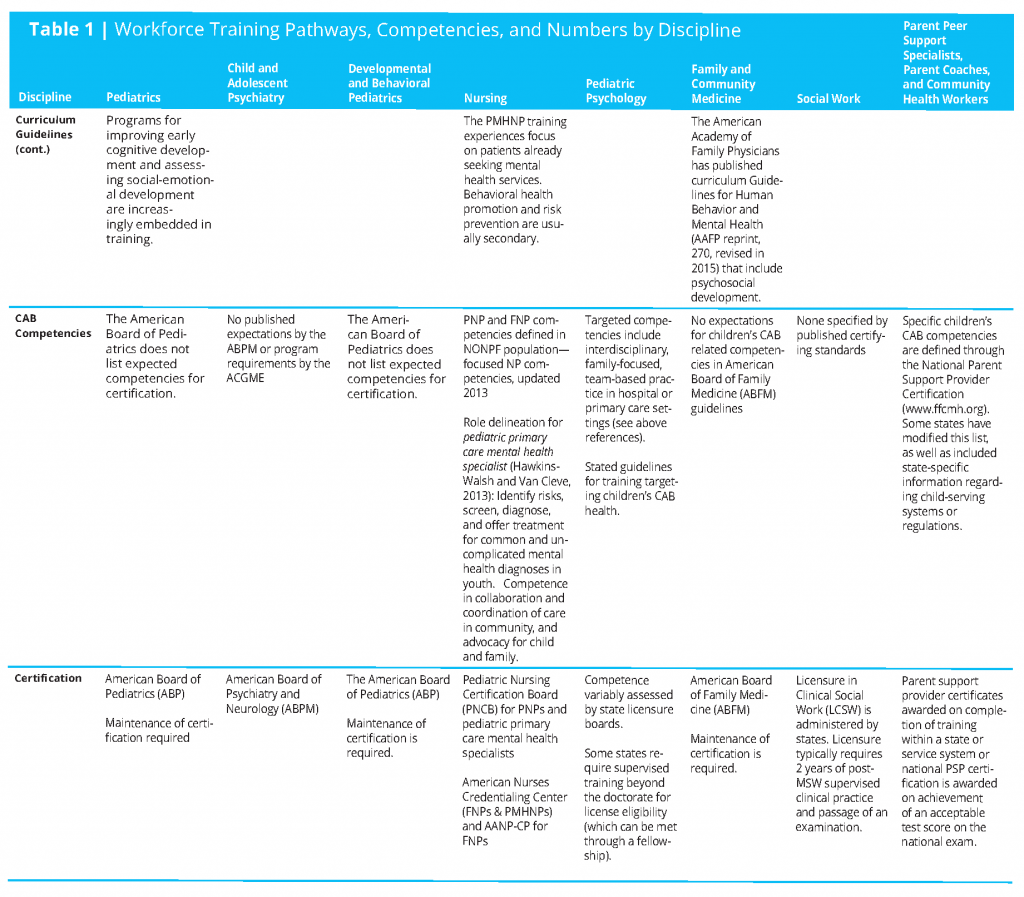
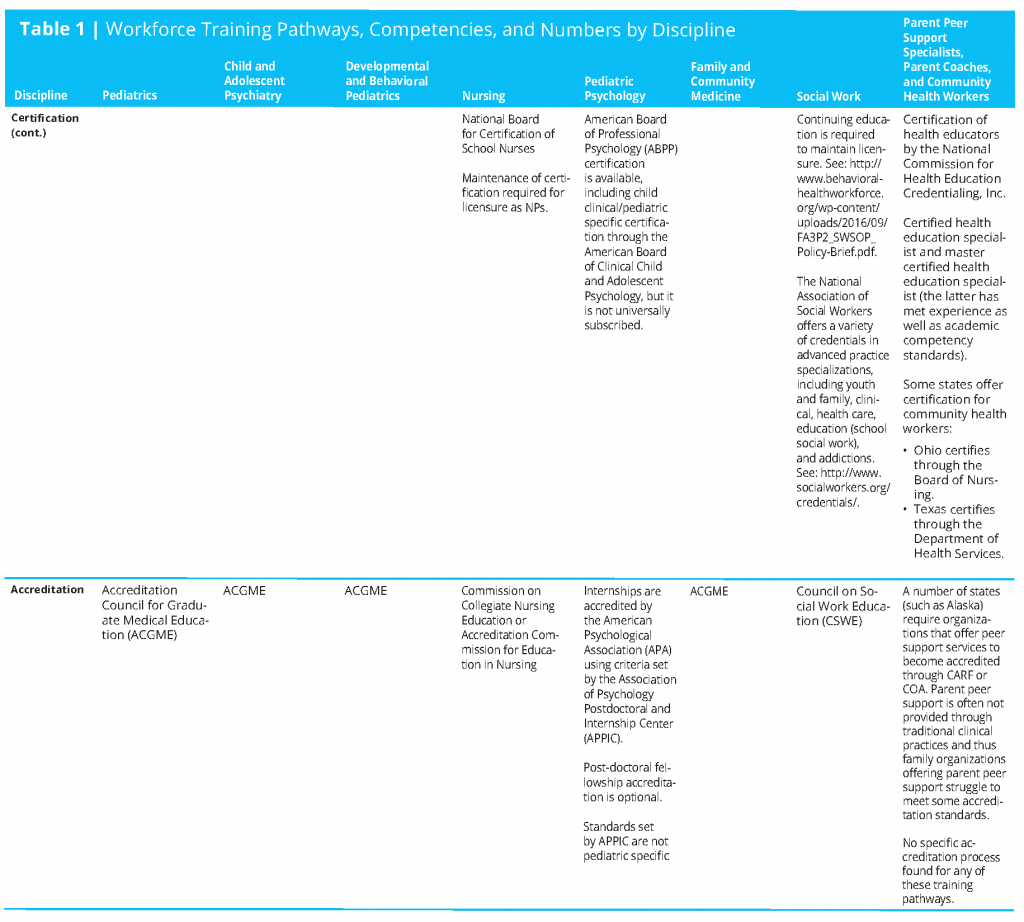
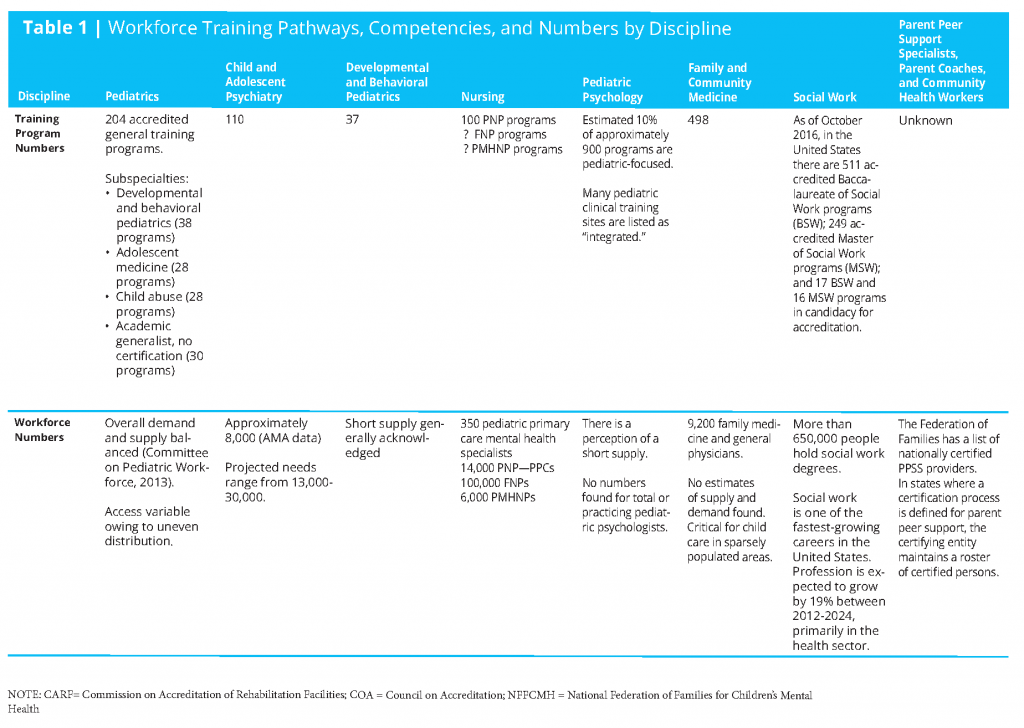
Workforce numbers are found in Table 1 (see page 18 for full table), though they are not particularly helpful in shaping a transformational plan to increase CAB health-related competencies of the child health care professional workforce. More specific and focused training opportunities and data from these opportunities will be needed.
Characteristics of a Health Care System That Will Promote Children’s CAB Health
Individuals participating in children’s CAB-promoting health care teams can come from a number of disciplines. A desired starting point would be providers who integrate medical and behavioral care. Health care providers in the domains of nurse practitioner, family medicine, obstetrics and gynecology, and pediatric practice, as well as behavioral health providers (whether physicians, psychologists, social workers, nurses and nurse practitioners) can be key contributors in promoting children’s CAB health. Family medicine providers have the advantage of being able to work with parents during the prenatal and postnatal care periods. Obstetricians and gynecologists are ideally situated to play an important role as providers of parent counseling for expectant parents around the impact of healthy fetal development on children’s CAB health. Nurse practitioners are increasingly providing primary care for children and families. Some pediatric practices provide a single prenatal visit for parents, which is an opportunity for positive parenting interventions before the birth of their child. Child psychiatrists do not provide primary care, but increasingly they are participating—either on-site or through telehealth—in primary care practices (AACAP, 2012) and could be in a position to provide consultation on the optimal preparation of parents to promote CAB wellness of their children.
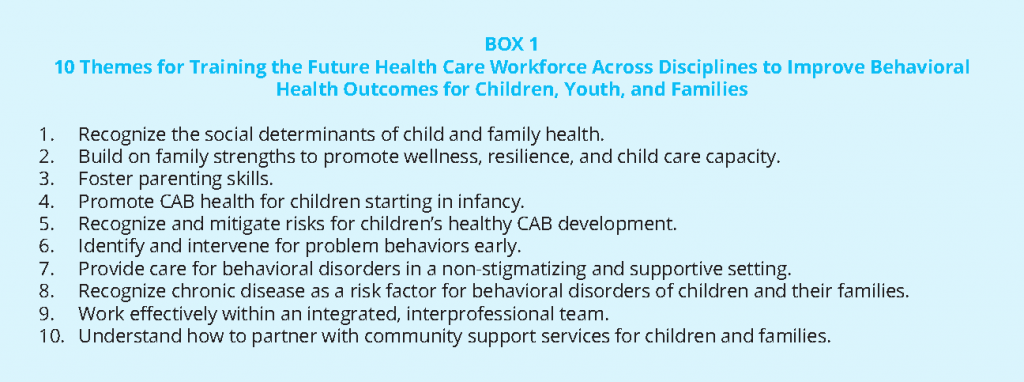
Not surprisingly, training of health care professionals who serve children and families varies considerably across disciplines. The expectations for training to create an integrated workforce need to be defined both within disciplines and between them. Interprofessional training needs greater primacy. Indeed, there are common themes that should be included in discipline-specific and interprofessional training programs. These themes promote understanding of the perspectives and capacities of all disciplines and professions entrusted with the physical and behavioral well-being of children and youth (Schmitt et al., 2013). Box 1 lists 10 themes that are applicable to training content across disciplines. Several of these themes will be the subject of further comment, but all of them are important considerations in the creation of integrated care training programs that more effectively promote CAB health for all children.
Interprofessional Care
Integrated care has gained considerable popularity in the health care field and provides an ideal framework for child health care trainees to experience and develop competency in the area of child behavioral health promotion and disorder prevention. In practice, it is unlikely that, alone, a physician, a psychologist, a social worker, an advanced nurse practitioner, a trained parent peer support provider, or any other practitioner will be able to devote the time and provide all of the expertise needed to work optimally with each family around these issues. Behavioral health promotion and prevention efforts will require an integrated team effort, and trainees must have an opportunity to develop comfort and confidence in interactive, coordinated, and collaborative health care delivery. Understanding the strengths and limitations in the expertise of other disciplines is fundamental to effective collaboration. Ideally, interprofessional care extends beyond colocation of various disciplines to team contributions that include joint care planning as well as coordinated, efficient care delivery. Opportunities for each discipline to work up to the high end of their competency will allow for the highest levels of professional satisfaction and value as participants in interdisciplinary care delivery.
Family-Centered Care
Perhaps most important is the acknowledgment of parents as providers of health care for their children and as important members of the health care team. Adolescents themselves are also important consumers and members of health teams. The concept of coproduction of health care (Batalden et al., 2015) involving both health care professionals and patients or family members encapsulates a fundamental tenant of family-focused care: it is especially critical when dealing with children and adolescents given their dependency on their families.
Understanding and acknowledging the importance of shared decision making that opens the door to expression of patient/family needs and preferences is an important competency for health care professionals. Ideally, parents will be fully accepting of those roles and eager to promote optimal CAB development for their child. As is the case for all team members, parents and other family members benefit from education and training to contribute to the full extent of their abilities. In a number of settings, parenting groups are a main source of information, problem solving, and encouragement for all participants (Breitenstein et al., 2012). Health professionals should be trained at the earliest opportunity to work with parents as partners in care decisions and implementation of care plans for their children. An important characteristic of health care professionals’ increasingly effective work with children will be their ability to understand the context for care in the home and to tailor considerations for CAB promotion of children to the resources in the family setting.
Multigenerational Care
Historically, pediatric health care has targeted the well-being of the child. Increasingly, it is recognized that care at home that leads to satisfactory or optimal children’s CAB health and development depends on the health and well-being of the parents and other family members. Pediatric practices have begun to consider how to contribute to multigenerational health by assessing the health of the parents: for example, by screening for exposure to adverse experiences and behavioral disorders such as depression (Briggs et al., 2014; Dubowitz, 2014), and by embedding help with economic, social, and behavioral issues in the practice. Family medicine practices have the opportunity to coordinate multigenerational care. Training within the context of addressing the health needs of all members of the family will provide a workforce across disciplines that is better prepared to promote CAB health and development.
Community-Linked Care
Many supportive services for children and families that address CAB issues are community-based, among them home visitation programs, preschools and schools, community health programs, and community agencies. Just as it is essential for health care professionals working with children to understand the context for care in the home, it is equally important for those professionals to understand the context for social engagement in other environments in which children spend a significant part of their lives (e.g., school). Trainees in the health care system should be familiar with community-based resources and gain facility with linking families to them as seamlessly as possible. Trainees should be exposed to and participate in educational sessions concerning the social determinants of health. In addition, they should have firsthand experience with community-based support programs. Organizing effective bridges for health care providers to community partners can be an important step in creating training experiences that lead to lifelong comfort and competence in extending CAB health promotion beyond the walls of health care settings.
Current Training Across Participating Disciplines
This section addresses a number of disciplines that should be prepared to participate in family-focused CAB health promotion and prevention activities within primary and subspecialty health care. Within the description of each discipline, it addresses current training pathways and outlines the relevant certification processes, program accreditation bodies, and discipline-specific expectations for behavioral health training in general and training for CAB health promotion in particular.
Training Physicians
Clinical experiences in medical school provide opportunities to introduce the topic of children’s CAB health; however, the topic at this time is not considered a fundamental component of medical knowledge, and exposure to it is inconsistent. Topics such as the social determinants of health, interprofessional training, and team-based care are finding their way into student clinical exposures and provide hope that children’s CAB health will one day be a part of every student’s clinical experience.
The usual pathway in the United States for residency training in general pediatrics, family medicine, psychiatry, or obstetrics and gynecology is a three- or four-year curriculum in an accredited program. Training in most subspecialty areas of pediatrics and other specialties requires an additional 1 to 3 years, including in pediatrics 1 to 2 years that are devoted to scholarly activity. American Board of Medical Specialties (ABMS) core competencies for all medical specialties are organized into six categories: Patient Care and Procedural Skills; Medical Knowledge; Practice-based Learning and Improvement; Interpersonal and Communication Skills; Professionalism; and Systems-based Practice (ABMS, 2016). These competencies are outlined at a high level and do not address specific training goals such as the ability to identify and treat/refer behavioral disorders or participate in efforts to promote CAB health and prevent behavioral disorders. The Accreditation Council for Graduate Medical Education (ACGME), through its program review committees, does not mandate training experiences that address family-focused behavioral prevention and care interventions.
Pediatrics
For general pediatrics training, the Residency Review Committee of the ACGME requires that one unit (usually 4 weeks) must be in developmental-behavioral pediatrics. Residents can opt for additional behavioral pediatrics by participating in one unit of Child Abuse and/or Child and Adolescent Psychiatry (ACGME, 2016f). Thus, resident formal experience with the behavioral dimensions of child health is limited, particularly if the Developmental-Behavioral rotation is heavily oriented to developmental disabilities or if the resident takes vacation time during this rotation. A continuity ambulatory pediatrics experience includes focus on anticipatory guidance of the parents and older children. Promotion of children’s CAB health is not a major component of this activity in most programs. The American Board of Pediatrics (ABP) mentions promotion of health as a target competency, but nearly all dimensions of competence relate to diagnosis and treatment of disorders (ABP, 2016). A number of reports in the literature describe models for assessing behavioral risk and intervening for disorders in primary care practice (Dubowitz, 2014). The application of these models to training experiences and training outcomes has not been systematically addressed, however. Neither training program accreditation nor certification requirements and expectations speak to CAB health promotion and risk prevention and mitigation; multigenerational health needs; promotion of parenting skills; early screening; and interventions for behavioral risk or concerns.
The American Academy of Pediatrics (AAP) has addressed the behavioral health needs of children and adolescents and recommended pertinent training experiences and competencies (Committee on Psychosocial Aspects of Child and Family Health and Task Force on Mental Health, 2009). Additionally, at this time, the ABP is publishing a statement of the need for behavioral health training in pediatrics in the form of a “Call to Action” paper (McMillan et al., in press), but as yet the ABP has not addressed behavioral health promotion and risk prevention. A detailed statement by the ABP that addresses training of subspecialists (Freed et al., 2014) does not include expected competency of trainees for participation in CAB health promotion or behavioral care of their patients.
Serious gaps are noted when pediatric residents are surveyed about their perceived competency as a result of their training experiences (Fox et al., 2010; Horwitz et al., 2010). In most training programs there is little if any coordination among the several potential exposures to behavioral health, and therefore there is no thoughtful or integrated curriculum for this vital area of child health. Furthermore, because neophyte pediatricians are focused on acquiring the basic skills and identity of pediatrics they are often less interested in learning the subtleties of mental health prevention. It is later, when they have completed training and entered practice, that surveys of pediatricians about training deficiencies usually find behavioral health as the most frequently cited deficiency. Likewise, even though expected pediatric competencies include relating to other health professionals, there is no mention in program requirements or trainee competency expectations of an ability to function effectively within the context of interdisciplinary team care.
Some academic training programs are using social-emotional as well as developmental screening tools as a routine part of health surveillance. Pediatric residents have been successfully inserted into adverse experience screening of families as part of the SEEK program (Dubowitz, 2014) or parenting training using the Triple P program (McCormick et al., 2014), both showing that residents’ knowledge and skills were improved. These are isolated examples of activities that increasingly should be considered for pediatric training.
Most pediatric subspecialty training programs are academically based. Program accreditation and trainee certification are separate processes for each subspecialty area. Because behavioral and emotional problems are common in children with disabling and life-threatening chronic disease, the opportunity to prospectively address patient and family wellness as well as behavioral problems and disorders should be acknowledged and increasingly addressed as a joint responsibility of the entire team. At this time, pediatric subspecialty training for the most part does not prepare learners to participate effectively in family-focused, multigenerational CAB support and care. Neither the pediatric subspecialty training accreditation nor the subspecialist certification processes have communicated expectations for preparation of trainees to address CAB health.
One exception may be the training of developmental and behavioral pediatric subspecialists. Their behavioral training orientation is largely diagnosis and treatment. The ACGME program requirements for this subspecialty area include “understanding the biological, psychological and social influences on development in the emotional, social, motor, language and cognitive domains” and focus on “mechanisms for primary and secondary prevention of disorders in behavior and development” (ACGME, 2016d). There are only 38 training programs in developmental and behavioral pediatrics and relatively few subspecialists in this field (ACGME, 2016h). Interdisciplinary team experiences during training are most advanced for developmental and behavioral pediatrics.
Although accreditation requirements for training in adolescent medicine largely ignore the CAB dimensions of adolescent health, trainees in this subspecialty (who can come from core training in pediatrics, internal medicine, or family medicine) are exposed to areas such as eating disorders, depression and screening for this disorder, suicide prevention, LGBTQ health concerns, and substance use (ACGME, 2016b). The extent to which health promotion and preventive approaches to CAB health are incorporated into trainee experiences is at best uneven.
General Psychiatry
General psychiatry training includes exposure to child mental health, and individuals trained at this basic level may be involved with youth. ACGME requirements for general psychiatry training programs mention prevention but almost exclusively target diagnosis and treatment of behavioral disorders. There is no mention of behavioral health promotion, identification of risks and their mitigation, family-focused care, or engagement with community programs that embrace these topics. There is a single mention of resident participation on interprofessional teams, but there is no language defining an interprofessional practice or site, and no language outlining what preparation for interdisciplinary or integrated practice might entail. A single statement notes that on completion of training residents should understand sociocultural issues. The most frequent and successful integration efforts involving psychiatrists have been directed at adult care and are diagnosis and treatment oriented (ACGME, 2016g).
Child and Adolescent Psychiatry
Numbers of child psychiatrists are estimated to be as low as 20 percent of the workforce need (AACAP, 2016) and have limited their ability to move beyond traditional care of children and adolescents who are seriously compromised by behavioral disorders. Nevertheless, all child psychiatry residents are required to train in school-based settings, allowing for exposure to an alternative system and a broader spectrum of youth. The integration of psychiatric care into primary care pediatric settings is beginning to receive attention. The most successful integration efforts have been directed at adult care and are diagnosis and treatment oriented. Discussions about integration of child psychiatry practice into pediatric primary care are active at the professional society level (Fritz, 2016), but applications are scattered and largely carried out as pilot programs.
The ACGME training program requirements for the child psychiatry fellowship, which follows a general psychiatry residency, are much the same as for general psychiatry resident training (ACGME, 2016c). Child and adolescent psychiatry training is defined to include prevention, diagnosis, and treatment of behavioral disorders. The extensive outline of requirements for training programs and trainee experiences has always included the expectation that child psychiatry trainees understand the stages of normal development from infancy through adolescence. The ACGME child and adolescent psychiatry milestones project has for the first time added requirements relating to the identification of factors contributing to wellness and resilience. Experience of at least a month in a community psychiatry setting is required, with the content of the experience being determined by the local community resources. Although child and adolescent fellows are expected to have training experiences as participants on interprofessional teams, no mention is made of experience in clinical settings, either ambulatory or hospital, where behavioral and physical medicine are systematically integrated. Consultation experiences within primary and/or specialty pediatric care are a required part of psychiatric training; they usually occur on inpatient units with youth who are acutely or chronically ill enough to require hospitalization (ACGME, 2016c).
Combined Training Programs
Combined training programs in pediatrics, adult psychiatry and child and adolescent psychiatry (Triple Board, 2016) and combined training in family medicine and psychiatry are approved by the individual boards and lead to trainee certification in each of these specialties. Both programs would seem to provide excellent training venues for individuals who have an interest in integrated behavioral and traditional medical practice; indeed, a number of trainees from these programs are now providing leadership for integrated care pilot programs using a variety of models. Training program accreditation guidelines for combined training largely mirror training guidelines for the individual specialties and are diagnosis and treatment focused. As with the parent specialty training program guidelines, no training program guidelines or requirements for goals or experiences relating to children’s CAB development and health are specified. Behavioral health promotion and prevention of risks for problem behaviors may be addressed at some level within individual training programs, but there is little available evidence of specific expectations related to these competencies at the specialty board or ACGME levels (ACGME, 2016a).
Family Medicine
Family Medicine physicians have the advantage of providing multigenerational care and have traditionally been trained, more so than pediatricians, to diagnose and treat behavioral health issues. As is the case for all specialty areas of the ABMS, competencies to be acquired by a family medicine physician are outlined only in broad topical areas that have been adopted by all specialty boards. ACGME program requirements for GME in family medicine are more detailed and include several statements about competencies in behavioral health. These include “[D]iagnose, manage and coordinate care for common mental illness and behavioral issues in patients of all ages.”; “The curriculum must be structured so behavioral health is integrated into the residents’ total education experience.”; and “There must be a structured curriculum in which residents are trained in the diagnosis and management of common mental illnesses” (ACGME, 2016e.). Further, the competency requirements include an ability to “assess community, environmental, and family influences on the health of patients,” to “provide preventive care,” and to “address population health, including the health of the community” (ACGME, 2016e). The requirements also specify that residents must work in interprofessional teams to enhance patient safety and care quality. There is no language in the training program requirements for exposure to or competence in areas of behavioral health promotion or prevention of risks for problematic behaviors. While some family medicine physicians are in a position to work with families around conception, pregnancy, and birthing, there is no training requirement that addresses prenatal and postnatal family-focused behavioral wellness or parenting promotion competencies.
The American Academy of Family Physicians (AAFP) has published its recommended curriculum guidelines for residents, entitled Human Behavior and Mental Health, first in 1986 and most recently in 2015 (AAFP, 2015). These guidelines comprehensively address acquisition of competencies, attitudes, knowledge, and skills related to behavioral health. Family medicine residents are expected both to assess risk of patients for abuse, neglect, and other disruptive family-related factors and to screen for traumatic experiences. They are likewise expected to recognize the impact of complex family and social factors on individual health and the psychosocial dynamics that influence human behavior. Understanding the importance of multidisciplinary approaches to health care is emphasized. Knowledge acquisition addresses not only mental health disorders but also basic human behaviors, including psychosocial growth and development as well as interrelationships among biologic, psychologic, and social factors. While emphasizing family context and relationships, little attention is paid in these guidelines either to child behavioral and cognitive development and health or to the critical role of nurturing parental roles in behavioral health promotion.
There are a limited number of combined family medicine and psychiatry residency training programs (Association of Medicine and Psychiatry, 2015). These trainees should be advantageously positioned to take on a lead role for child and family behavioral health promotion and risk prevention.
Obstetrics and Gynecology
Obstetricians and gynecologists (OB/GYNs) provide primary care for many women and are positioned to influence outcomes of family planning and the arrival of children. OB/GYN practices frequently offer classes for expectant couples, but the content of these classes more often addresses physical care of children and breast-feeding than positive parenting. OB/GYN physicians have an ideal opportunity to influence CAB outcomes before and in the early stages of parenting. No mention is made, however, of board or residency program review expectations for resident participation in learning about relevant prenatal counseling. There is also no mention in the ACGME program requirements about stress and other adverse exposures leading to epigenetic modifications of gene expression that can be harmful to the child. A statement of relevance to CAB health mentions that residents must have an opportunity to work as a member of effective interdisciplinary teams and must be able to demonstrate a personal role in the provision of family-centered care (ACGME, 2016i).
Training Nonphysicians
Pediatric Psychology (1)
Psychology providers are increasingly participating as key members of child health care sites and systems, whether targeting child and family needs owing to chronic disease and disability or the process of well-child care and acute care.
The training pathway for pediatric psychologists includes the following training experiences:
- Graduate training leading to a Ph.D. or Psy.D. that includes clinical practicum training and a 1-year clinical internship/residency.
- One-year internships in accredited pediatric psychology programs provide clinical experiences and scholarship (possibly including research), leading to a specified level of clinical competence. Hospital-based internships may provide experience in primary care settings. Satisfactory completion of this experience, usually off-site from the graduate program, is a requisite for the award of a doctoral degree.
- Postdoctoral fellowships in pediatric psychology are common and consist of 1 to 2 years of pediatric clinical training and, in some cases, intensive research experiences. Fellowships can be differentiated based on program clinical focus. While many are hospital-based and concentrate clinical experiences on children with serious acute and chronic disorders, a growing number of fellowships target the fellow’s clinical experiences and competence goals to the primary care area.
Pediatric psychologists are licensed by states in which they practice. Some states require an additional year (or even 2) of supervised experience beyond the doctoral degree (which may be a fellowship) for license eligibility, while other states will grant license eligibility if the completion of a Ph.D. or Psy.D. has provided the requisite number of years of supervised clinical experience.
Evaluation of trainee competence as a clinician is largely the task of each sequential training program. Palermo et al. (2014) defined core competencies for pediatric psychology across training levels that are being used by many programs as a framework for evaluation of candidates. This set of recommendations was created by a task force that was assembled by the Society of Pediatric Psychology (Division 54 of the American Psychological Association). These recommendations include themes that are highly relevant to family-focused prevention, such as having knowledge of the effects of families and socioeconomic factors on CAB development and health and the roles of other disciplines in achieving behavioral health promotion. Hoffses et al. (2016) have adapted these recommendations for pediatric psychology training specific to the primary care setting. Other recent publications
have also addressed core competencies. McDaniel et al. published detailed competency recommendations for psychology practice in primary care in six broad domains (McDaniel et al., 2014). Piazza-Waggoner et al. (2015) built on the Palermo et al. (2014) recommendations by suggesting a training developmental trajectory assessment and the need to map professional competencies to health outcomes of children and youth.
Accreditation of psychology internships and fellowships is done generically—that is, for all programs, both adult and pediatric—by the American Psychological Association (APA), and accredited programs are recognized as meeting criteria set forth by the Association of Psychology Postdoctoral and Internship Centers (APPIC). APPIC also conducts an internship match and is considering a postdoctoral fellowship match process in the future. There are no stated criteria for provision of specific training experiences. Criteria largely deal with program structure, processes, and goals. Flexibility across and within programs regarding specific training experiences is supported by the current accreditation process and various program content recommendations. It has been estimated that less than 10 percent of the approximately 900 psychology training programs are focused on preparation for careers addressing the needs of children and adolescents. Numbers of practicing pediatric psychologists are difficult to ascertain, as licensure is granted generically to all applied psychologists by state boards. Geographic distribution is uneven, and a 2007 report, An Action Plan for Behavioral Health Workforce Development (Annapolis Coalition on the Behavioral Health Workforce, 2007), prepared for the Substance Abuse and Mental Health Services Administration (SAMHSA) stated that the behavioral health workforce in general is uninformed about and unengaged in health promotion and prevention activities (APA, 2014).
Clinical competence is assessed as a step in the licensure process in many states. Candidates for licensure must pass an examination that is generic, nationally administered, and agnostic regarding training or practice focus, but some states require an additional oral examination that may be clinically based. Similarly, maintenance of competence is assessed by state licensing boards, largely through verification of participation in approved continuing education programs. There is a certification process that is conducted by the American Board of Professional Psychology. This independent board certifies individuals with training in 15 different specialty areas within psychology, one of which is “Clinical Child and Adolescent Psychology.” Board certification is optional for psychologists, and it appears that many pediatric psychologists are not certified.
While a number of internship and fellowship programs are heavily focused on behavioral dimensions of childhood chronic disease—and a growing number of other programs focus on behavioral health in primary care settings—a common feature of child psychology training programs is preparation for interdisciplinary, family-focused, team-based child behavioral health care practice that includes a health promotion and prevention orientation. Thus, unlike the training for a number of other health care specialty careers, there may be less urgency in psychology to expand current program content and trainee experience to achieve a workforce that can advance the CAB health of children through promotion, prevention, and early intervention activities in health care settings. The extent to which promotion and prevention components are implemented today in training and their impact on
post-training practice are unclear, however.
Research training and competence is expected of all Ph.D. pediatric psychology programs. A thesis is also an expected product for the Psy.D., and many trainees have publications in the peer-reviewed literature by the time they graduate. Fellowship programs, especially those of 2 year’s duration, also provide postdoctoral research experiences. Thus, many pediatric psychologists are engaged in rigorous research after training, and they should be positioned to make important contributions to outcomes and program improvement research related to improving children’s CAB health.
Psychologists in the medical setting are currently reimbursed for diagnosis, psychological assessment, treatment, and behavioral health consultations (“health and behavior” Current Procedural Terminology codes) with medical patients. Compensation models that reimburse efforts to promote and prevent risks for children’s CAB health represent an important challenge for public and private payers, and not all reimburse health and behavior codes.
Nurses
Licensed registered nurses graduate from a school of nursing within a college or university that is accredited by one of two national accreditation agencies (Commission on Collegiate Nursing Education [CCNE] or Accreditation Commission for Education in Nursing [ACEN]). Upon graduation they must sit for a national licensing exam (NCLEX). Nurses do not specialize in a specific population while becoming RNs. Nurses at all levels of training do participate in child health care, specifically the behavioral dimensions of child health. Health promotion and risk reduction are cornerstones of a nursing curriculum. Nurses also take coursework in community health and are placed in field experiences with community agencies. Pediatric nursing courses focus on the “protection, promotion, and optimization of the health and abilities for children from newborn age through young adulthood” (NAPNAP, 2015). During their nursing programs students take formal classes in growth and development and pediatric health and illnesses and have a clinical rotation in pediatrics. Upon completion and licensure and after gaining experience working with children, a registered nurse (RN) may choose to sit for an additional elective certification exam (e.g., as a pediatric nurse or school nurse).
School nurses have an expanding role in health promotion, surveillance, and the care of school-age children, including preschool children in some settings. Some have the opportunity to work in a school-based clinic, which serves as the child’s medical home through which care is coordinated with local child health practices (AAP Council on School Health, 2016). Certificates in school nursing (NCSN) are available to licensed RNs who have had 1,000 hours of school nursing experience and successfully pass a voluntary certification exam administered by the National Board for Certification of School Nurses (NBCSN). Recertification occurs every 5 years and can be accomplished by testing or continued education credits. There are more than 3,500 school nurses with the NCSN certificate.
As pediatric practices embrace the role of the medical home, roles for nurses within these settings are likely to grow. Nurses bring specific training in the role of health educator and counselor as well as a conceptual framework of caring that positions them well to contribute to CAB health promotion.
Nurse Practitioners
Nurses who choose to become an Advanced Practice Registered Nurse (APRN) return to an accredited university program at the level of a master’s or doctoral degree. They select one of four APRN roles: the nurse practitioner, the clinical nurse specialist, the certified nurse anesthetist, or the certified nurse midwife. APRNs in all of these roles will hold a second license, which provides them with an expanded scope of practice. Nurse practitioner programs prepare the student for an expanded role with a specific population: that is, pediatric nurse practitioner – primary care; family nurse practitioner; or psychiatric mental health nurse practitioner. These programs typically involve 2-4 years of didactic coursework, simulation experiences, standardized patients, and clinical rotations.
- Pediatric nurse practitioner–primary care: Students typically spend 1 or 2 days a week seeing patients in pediatric primary care settings under the supervision of a pediatrician or pediatric nurse practitioner. Additionally, they often elect rotations in the hospital, the community, and in school-based health clinics. Electives in developmental-behavioral settings have limited availability.
- Family nurse practitioner: Students focus on the health and illnesses of patients of all ages from birth through old age. Therefore, the pediatric focus within an FNP program may be limited to a semester.
- Psychiatric mental health nurse practitioner: Students focus on individuals across the life span, families, and populations at risk for developing or having a diagnosis of psychiatric disorders or mental health problems. The PMHNP provides continuity care to patients seeking mental health services in a wide range of settings. Upon successful completion of an NP program, the graduate is eligible to sit for a national certifying examination (Pediatric Nursing Certification Board [PNCB], American Nurses Credentialing Center [ANCC], or American Academy of Nurse Practitioners Certification Program [AANPCP]) that matches their area of study. These examinations are based upon the competencies identified through role delineation studies conducted every 3-5 years and endorsed by all major nurse practitioner educational bodies (National Organization of Nurse Practitioner Faculties [NONPF]). Recognized competencies have been expanded to include interprofessional teamwork and greater attention to behavioral health.
There has been an outgrowth of new courses that are co-taught by faculty from two or more programs (nursing, social work, and psychology). A pediatric health assessment course provides students with the skills to assess behavioral and mental health risks as well as physical health. In 2004 the Association of Faculties of Pediatric Nurse Practitioners (AFPNP) was awarded a grant by the Commonwealth Fund to implement and evaluate a national curriculum for students in 20 PNP programs that promoted the use of validated screening tools and evidence-based interventions for mental health concerns in primary care (Hawkins-Walsh et al., 2011; Melnyk et al., 2010). Licensure as a nurse practitioner is dependent upon continued maintenance of certification.
Specialty training beyond the NP
PNPs and FNPs who are employed in primary care pediatric settings and have interest in primary mental health care can acquire additional expertise through continuing education programs, conferences, formal coursework, and on-the-job training. (Examples include the Keep Yourself Safe and Secure [KYSS] and Research, Education, Advocacy, and Child Health Care [REACH] programs). A subspecialty certification is available to these NPs through an additional examination, the Primary Care Mental Health Specialist (PMHS), administered by the PNCB (2016). A survey of 270 nurses working in this role listed the five highest-ranking tasks. At the top of the list was “promoting positive parenting” (Hawkins-Walsh and Van Cleve, 2013). More than 350 NPs have been certified for the PMHS certification, and in addition to pediatric practices, a small number of those with the PMHS certification are working in developmental-behavioral pediatrics, in their own independent practice, in school-based health care, or in group child psychiatric, neurology, or psychology practices. In its recent statement on Integration of Mental Health Care in Pediatric Primary Care Settings, NAPNAP (2013) recommends that its more than 8,500 members consider certification in primary mental health care. Certification is granted for 3 years, at which time recertification is required.
There is considerable opportunity for specialized nurse practitioners to bolster the workforce that is prepared to promote children’s CAB health.
Nurse Midwives
The certification examination for certified nurse midwives (CNMs) and certified midwives (CMs) falls under the American Midwifery Certification Board (see: www.amcbmidwife.org) and is taken every 5 years. The accrediting agency requires that the certification exam be based upon those tasks being done by recently employed CNMs. There are approximately 11,200 currently practicing CNMs and fewer than 100 CMs (ACNM, 2016). In recent years, close to 500 new CNMs enter practice each year. They contribute significantly to the prenatal and postnatal care of women. In the most recent task analysis, certified CNMs and CMs reported the education of new mothers and preparation for infant care as significant tasks as well as screening for perinatal depression. CNMs have gained attention in some locales for their role in sponsoring and conducting group prenatal visits that address parenting skills. It appears that CNMs are able to play an important role in the CAB health of young families.
Licensed Professional Counselors and School Counselors
While not common, there are primary health care practices that employ counselors for behavioral-health-related expertise and contributions to interdisciplinary care. Numerous counseling degrees are being offered; two common ones are school counselors and licensed professional counselors (LPCs). School counselors provide evaluations and, in some cases, therapeutic interventions. School counselors participate in school-based health clinics and can be an important source of information related to a child’s health surveillance and maintenance through the medical setting. LPCs, numbering more than 120,000 in the United States, are recognized in all 50 states (American Counseling Association, 2011). Licensure requires a combination of a master’s or doctoral degree and counseling experience with supervision, in addition to a passing grade on a national examination. Academic course work features normal growth and development as well as social determinants of health, but it does not specify exposure or competency in the area of children’s CAB health and development. Certification for LPCs is optional and can be obtained from the National Board for Certified Counselors (see: www.nbcc.org). Certification can also be obtained for such children’s CAB relevant specialty areas as mental health counseling and school counseling. No information concerning standards for graduate school curricula has been identified. The number of required hours of supervised clinical experience is variable and is designated by each state licensure board.
Social Workers
Social workers are often important participants in child health care delivery, in primary care settings where the social determinants of health are major factors, and for youth who have disabling or life-threatening chronic diseases that require compliance with complex treatment plans in home and community settings. The functions of social workers in pediatric primary care follow two alternative and complementary models. Under the Chronic Care Model, social workers serve as care managers—often in collaboration with nurses—for families with children who have sustained medical and psychosocial needs that require multiple caretaker involvement. Second, following the long-standing involvement of social work in the provision of mental health services, some social workers serve as behavioral health specialists who conduct standardized assessments and provide discrete, evidence-based behavioral health interventions for children, adolescents, and families. Social workers are the largest group of clinically trained mental health providers in the country (SAMHSA, 2013).
Social workers can focus their baccalaureate training so as to be qualified as children, youth, and families social workers. Master of Social Work (MSW) trainees are viewed as advanced practitioners in this area. Certification in this social work specialty area is available. Another specialty option relevant to children’s CAB health is school social work. Many social workers are employed by social service agencies or schools. Many MSW social workers go on to qualify for a license in clinical social work (LCSW). Schools of social work and professional organizations offer a variety of certificate programs for advanced training (NASW, 2016).
Furthermore, psychiatric social workers must earn an MSW degree and be licensed to practice in their state. In general, they are part of psychiatric treatment teams, often hospital based. Their participation in primary or subspecialty child health care is infrequent and their focus is not often on children’s CAB health and development.
Large academic primary care practices and Federally Qualified Health Centers employ social workers to support family needs around issues raised by adverse health-related social determinants. Social workers also provide parent training programs in many settings, including primary care, schools, and child welfare agencies. For example, in a randomized controlled trial in pediatric primary care, Perrin et al. (2014) demonstrated the benefits of an adapted version of the Incredible Years program with parents of children with oppositional behavior; the intervention was provided by social workers and psychologists.
Accredited by the Council on Social Work Education (CSWE), training programs in social work emphasize both academic and applied practice preparation. The CSWE Educational Policy and Accreditation Standards (CSWE, 2016a) outline general educational requirements and, in part because social workers are employed in so many service systems, do not explicitly address child health, behavioral health, the social determinants of health, or prevention. Many social work programs, however, do offer “concentrations” or specializations that focus on behavioral health and clinical practice. Field education is considered a core pedagogy of the profession. Graduate students spend up to half of their time in internships. If students are in a health concentration, their internships are likely to be in integrated or hospital-based settings. Course work in social work helps students understand how social contexts influence health through a person-in-environment perspective. Curriculum content in health concentrations considers the full array of biopsychosocial determinants of behavioral and physical health. In 2012, CSWE launched a special curriculum development initiative focused on the expansion of integrated behavioral health curricula (CSWE, 2016c). Further, in 2014 the Health Resources and Services Administration (HRSA) awarded 62 MSW social work programs in excess of $26 million to expand training in behavioral health for integrated care settings (CSWE, 2016b).
MSW social workers are viewed as advanced practitioners, and demand for them is increasing in health care. The Bureau of Labor Statistics projects that 30,900 additional health care social workers—a 19 percent increase over 2014—and 22,300 additional behavioral health social workers—a 19 percent increase over 2014—will be needed in the United States by 2024 (BLS, 2015).
Family Peer Advocates, Parent Coaches, Health Educators, and Community Health Workers
Parent peer support specialists (PPSSs; also known as family peer advocates and family support specialists) have gained acceptance as important contributors to support of families of children and adolescents with mental health issues. The professionalization of the role of parent partners has grown from the early acknowledgment of the importance of family-centered care (Stroul and Friedman, 1994). Parents and community members with special skills represent a growing workforce with training programs and national and state credentialing bodies.
PPSSs are parents or relatives of children/adolescents with mental health needs and who increasingly are trained and credentialed to work as members of teams providing mental health support to families (Hoagwood, 2005; Koroloff et al., 1994, 1996; Osher et al., 2008). They work in a variety of settings, largely community-based but also in primary health care and schools.
In about 25% of states, family support services delivered by parent peers are now billable through public funding mechanisms (CHCS, 2012). PPSSs model, coach, and empower parents to cope with, advocate for, and better utilize health and mental health systems. PPSSs can help families connect through formal and informal support networks, and promote advocacy at the local systems as well as policy levels. Social support promotes parents’ own behavioral health and ability to cope with family needs. It also improves access to resources that can promote adjustment of their children (Ireys et al., 2001a,b).
The evidence for efficacy of parent-delivered family support should be strengthened (Blau et al., 2010; Hoagwood et al., 2010; Kutash et al., 2011). In an effort to promote standards and competency needed for this growing workforce related to children’s CAB health, the National Federation of Families for Children’s Mental Health (NFFCMH) created a Certification Commission for Family Support (http://certification.ffcmh.org/) and competencies to be considered for certification have been identified. There is broad consensus about tasks to be performed by PPSSs (Obrochta et al., 2011; NFFCMH, 2011) but little guidance for individual program evaluation and improvement.
A training program to support skill acquisition by PPSSs, funded by the National Institute of Mental Health (NIMH), was developed in New York State and has trained and credentialed more than 550 parent peer partners. Called the Parent Engagement and Empowerment Program (PEP), the original training program included a 1-week on-site training session followed by distance learning sessions on a biweekly basis for the next 6 months. The current training model involves both online modular curriculum completion and case consultation (see: http://www.ftnys.org/peptraining/).
Related supportive professional roles include trained health educators as parent coaches for families of infants in primary care practice. These coaches work with parents around issues of preventive care measures (anticipatory guidance), and parents reported enhanced behavioral/developmental awareness as well as enhanced satisfaction with the primary care experience (Beck et al., 2016). Bachelor’s degrees in health education are available and the U.S. Bureau of Statistics listed nearly 57,000 health educators in 2013. The National Commission for Health Education Credentialing gives an examination that, if passed, certifies each graduate as a health education specialist.
To bridge primary care practices to communities and cultures from which their patient population is derived, some practices have employed community health workers. Originally created in underserved countries to provide health information and support in the absence of sufficient numbers of health professionals, the concept is now applied to bring value to practices where adverse social determinants of neighborhood health are particularly prominent. Education of individuals to play this role is variable and differs from location to location. Some states offer certificates for community health workers. For example, Ohio certifies these individuals through the Ohio Board of Nursing. Texas provides certificates through the Texas Department of State Health Services. The American Public Health Association (APHA) has a section for community health workers. The value of these individuals in health care team approaches to family-centered, culturally appropriate CAB health promotion and prevention would be important to document.
Interdisciplinary, Family-Centered Models
The federal Leadership Education in Neurodevelopmental and Related Disabilities (LEND) training programs (AUCD, 2011) for children with developmental disabilities are highly interdisciplinary. LEND programs are focused on providing services for children with a range of disabilities, including those in the behavioral health realm. Since the primary focus of these programs is diagnosis, treatment, and functional rehabilitation, the content of these training programs may not provide an inclusive framework for interdisciplinary training in promotion-/prevention-focused health care experiences. It is likely that training program redesign will be an important component of preparation of the health care workforce to promote children’s CAB health. Model development, sharing of best interprofessional training practices, and testing of training outcomes will be important activities to foster and fund.
A Research Agenda to Support Integrative Workforce Training
Training health professionals to carry out effective research as well as clinical programs will be essential to the development of a strong evidence base for children’s CAB health promotion in the medical setting. Physicians who opt for pediatric subspecialty training are expected to conduct research or a scholarly project that can be focused on documenting program or educational outcomes. Health professionals who complete a Ph.D. or the equivalent have an intensive research experience that may prepare them to contribute substantially to the documentation of intervention and training outcomes. Effective multidisciplinary research with these goals will require attention to workforce development.
Research on effective training models has focused largely on single disciplines and, at times, on supervision models that support training in and delivery of evidence-based practices (Bridge et al., 2008; Goodfriend et al., 2006; Henggeler and Brondino, 1997; Hogue et al., 2013; Horwitz et al., 2015; Leaf et al., 2004; Manuel et al., 2009; Regehr et al., 2007; Schoenwald et al., 2000a,b; Schoenwald et al., 2009; Stein et al., 2008, 2009). The new workforce challenges described in this paper highlight the need for more integrative training that takes advantage of different expertise drawn from multiple disciplines, with the goal of enhancing collaboration and promoting quality of care in children’s health. Designing a research agenda to support this integrative training paradigm is likely to require attention to five areas: (a) comparative effectiveness studies that contrast training and supervision modalities (online, in person, etc.) and that target collaborative teamwork; (b) studies of the implications of alternative fiscal models (value-based purchasing; pay for performance) on training effectiveness; (c) comparative studies of different structural configurations of the interface of child medical care and behavioral health support (colocation, networked, discrete) on integrative services and training; (d) development of quality indicators that assess competencies for integrative team training and that lead to improved health outcomes for children; and (e) study of new, integrated training models for children with chronic, disabling disorders as well as for children in primary care.
Improving the feasibility and reach of training via alternative modalities (e.g., distance learning, online modules, and long distance consultation) is a focus of research in some health professions (e.g., psychology, social work). But these studies and the models upon which they are based do not typically include attention to integrative work with other professions. Integrative training models require clear differentiation of roles, establishment of different competencies and indicators of competence, joint contributions to configuring and assessing the care model, and attention to quality monitoring. Research in these areas is needed.
A range of new fiscal incentives, driven in large measure by Centers for Medicare and Medicaid Services (CMS) and the Medicaid reforms that are under way in more than two dozen states, affects delivery of service and places new demands on the workforce to collaborate across disciplines, to share expertise, and to bill for both integrative services as well as discrete specialty care. Promotion and prevention will be difficult to sustain in this setting unless payers reimburse for more than diagnosable disorders. Center for Medicare and Medicaid Innovation (CMMI) has opened the door for studies of team-based delivery models that are effective and provide value. The impact of different fiscal models on training approaches has not been a focus of research yet, but it is needed.
The health care changes in this country are also affecting where services are being delivered and how connections among different providers are structured. These structural configurations can include colocation of behavioral health providers within primary care offices, networked connections among health care providers under one entity, contracted referral services to improve access, and assumption of responsibility of health care institutions such as children’s hospitals for neighborhood or community health, etc. The impact of these different structural connections on the delivery of integrative health services has not been examined. Finally, health care services are increasingly held to new accountability standards that, among other requirements, necessitate documentation of workforce competencies and indicators that quality care is being delivered. These include competencies and indicators for “alternative” workforce staff, including parent peer support specialists (Olin et al., 2014). These accountability standards and workforce competencies or skills exist for some professions, but they are uneven across the range of disciplines that are needed to create integrative services. Development of these standards would benefit from research on the differential skill sets and competencies that lead to improved pediatric outcomes. Ultimate goals include the documentation of effectiveness and costs of fully integrated care and training that allow broad or universal consideration of this model of care by training program leadership, professional societies, credentialing and accreditation bodies, and both public and private payers.
Conclusion
Health professionals should be and are entrusted to promote the behavioral health and well-being of children, youth, and families. Training processes and required competencies, however, vary across disciplines. The expectations for training to create an integrated workforce need to be defined relative to each discipline, but there are common themes—promoting CAB health and resilience in children and families—that should be included in training programs for all of those caring for children.
Notes
- Child clinical psychologists are not fully distinguishable from pediatric psychologists (and some are both). Training requirements are similar for both specialties. Child clinical psychologists typically focus on children and youth with behavioral health conditions; pediatric psychologists commonly work with children and youth with medical conditions or in primary care.
References
- Accreditation Council for Graduate Medical Education (ACGME). 2016a. Accreditation Council for Graduate Medical Education. Available at: https://www.acgme.org/ (accessed November 18, 2016).
- ACGME. 2016b. ACGME program requirements for graduate medical education in adolescent medicine. Available at: http://www.acgme.org/Portals/0/PFAssets/2013-PR-FAQ-PIF/321_adolescent_med_peds_07012013.pdf (accessed November 6, 2016).
- ACGME. 2016c. ACGME program requirements for graduate medical education in child and adolescent psychiatry. Available at: https://www.acgme.org/Portals/0/PFAssets/ProgramRequirements/405_child_and_adolescent_psych_2016.pdf (accessed November 6, 2016).
- ACGME. 2016d. ACGME program requirements for graduate medical education in developmental-behavioral pediatrics. Available at: http://www.acgme.org/Portals/0/PFAssets/2013-PR-FAQ-PIF/336_developmental_behavioral_peds_07012013.pdf (accessed November 6, 2016).
- ACGME. 2016e. ACGME program requirements for graduate medical education in family medicine. Available at: http://www.acgme.org/portals/0/pfassets/programrequirements/120_family_medicine_2016.pdf (accessed November 6, 2016).
- ACGME. 2016f. ACGME program requirements for graduate medical education in pediatrics. Available at: https://www.acgme.org/Portals/0/PFAssets/ProgramRequirements/320_pediatrics_2016.pdf (accessed November 6, 2016).
- ACGME. 2016g. ACGME program requirements for graduate medical education in psychiatry. Available at: https://www.acgme.org/Portals/0/PFAssets/ProgramRequirements/400_psychiatry_2016.pdf (accessed November 6, 2016).
- ACGME. 2016h. Number of accredited programs academic year 2016-2017, United States. Available at: https://apps.acgme.org/ads/Public/Reports/ReportRun?ReportId=3&CurrentYear=2016&AcademicYearId=2016 (accessed November 6, 2016).
- ACGME. 2016i. Obstetrics and gynecology. Available at: https://www.acgme.org/Specialties/Overview/pfcatid/12 (accessed November 18, 2016).
- Agency for Healthcare Research and Quality (AHRQ). 2014. Medical expenditure panel survey: Statistical brief #434: The five most costly children’s conditions, 2011: Estimates for U.S. civilian noninstitutionalized children, ages 0-17. Available at: https://meps.ahrq.gov/data_files/publications/st434/stat434.shtml (accessed November 5, 2016).
- American Academy of Child and Adolescent Psychiatry (AACAP). 2012. Best principles for integration of child psychiatry into the pediatric health home. Available at: https://www.aacap.org/App_Themes/AACAP/docs/clinical_practice_center/systems_of_care/best_principles_for_integration_of_child_psychiatry_into_the_pediatric_health_home_2012.pdf (accessed November 5, 2016).
- AACAP. 2016. Workforce issues. Available at: http://www.aacap.org/aacap/resources_for_primary_care/Workforce_Issues.aspx (accessed November 6, 2016).
- American Academy of Family Physicians (AAFP). 2016. Human behavior and mental health. Available at: http://www.aafp.org/dam/AAFP/documents/medical_education_residency/program_directors/Reprint270_Mental.pdf. (accessed November 18, 2016).
- American Academy of Pediatrics (AAP). 2016. Bright futures/American Academy of Pediatrics: Recommendations for preventive pediatric health care. Available at: https://www.aap.org/en-us/Documents/periodicity_schedule.pdf (accessed October 31, 2016).
- AAP Council on School Health. 2016. Role of the school nurse in providing school health services: Policy statement. Pediatrics 137(6): 34-39. https://doi.org/10.1542/peds.2016-0852
- American Board of Medical Specialties (ABMS). 2016. Based on core competencies. Available at: http://www.abms.org/boardcertification/a-trusted-credential/based-on-corecompetencies/ (accessed November 6, 2016).
- American Board of Pediatrics (ABP). 2016. Physician competencies. Available at: https://www.abp.org/content/physician-competencies (accessed November 6, 2016).
- American College of Nurse-Midwives (ACNM). 2016. Essential facts about midwives. Available at: http://www.midwife.org/acnm/files/ccLibraryFiles/Filename/000000005948/EssentialFactsAboutMidwives-021116FINAL.pdf (accessed November 18, 2016).
- American Counseling Association. 2011. Who are licensed professional counselors? Available at: https://www.counseling.org/PublicPolicy/WhoAreLPCs.pdf (accessed November 20, 2016).
- American Psychological Association (APA). 2014. Guidelines for prevention in psychology. American Psychologist 69(3), 285-296. Available at: https://www.apa.org/pubs/journals/features/amp-a0034569.pdf (accessed August 4, 2020).
- Annapolis Coalition on the Behavioral Health Workforce. 2007. An action plan for behavioral health workforce development—a framework for discussion. Available at: http://attcnetwork.org/find/respubs/docs/WorkforceActionPlan.pdf (accessed November 5, 2016).
- Association of Medicine and Psychiatry. 2015. Residency programs: Family medicine/psychiatry. Available at: https://assocmedpsych.org/studentstrainees/residency-programs/ (accessed November 20, 2016).
- Association of University Centers on Disabilities (AUCD). 2011. About LEND. Available at: https://www.aucd.org/template/page.cfm?id=473 (accessed November 6, 2016).
- Batalden, M., P. Batalden, P. Margolis, M. Seid, G. Armstrong, L. Opipari-Arrigan, and H. Hartung. 2015. Coproduction of healthcare service. BMJ Quality & Safety. https://doi.org/10.1136/bmjqs-2015-004315
- Beck, A. F., M. M. Tschudy, T. R. Coker, K. M. Mistry, J. E. Cox, B. A. Gitterman, L. J. Chamberlain, A. M. Grace, M. K. Hole, P. E. Klass, K. S. Lobach, C. T. Ma, D. Navsaria, K. D. Northrip, M. D. Sadof, A. N. Shah, and A. H. Fierman. 2013. Determinants of Health and Pediatric Primary Care Practices. Pediatrics 137(3). Available at: https://pediatrics.aappublications.org/content/pediatrics/137/3/e20153673.full.pdf (accessed August 4, 2020).
- Bethell, C. D., P. Newacheck, E. Hawes, and N. Halfon. 2014. Adverse childhood experiences: Assessing the impact on health and school engagement and the mitigating role of resilience. Health Affairs, 33(12),
2106-2115. https://doi.org/10.1377/hlthaff.2014.0914 - Bitsko, R. H., J. R. Holbrook, L. R. Robinson, J. W. Kaminski, G. Peacock, R. Ghandour, and C. Smith. 2016. Health care, family, and community factors associated with mental, behavioral, and developmental
disorders in early childhood United States, 2011-2012. Morbidity and Mortality Weekly Report, 65(9), 221-226. http://dx.doi.org/10.15585/mmwr.mm6509a1 - Blau, G. B., B. Caldwell, S. Fisher, A. Kuppinger, J. Levinson-Johnson, and R. Lieberman. 2010.The Building Bridges Initiative: Residential and community-based providers, families, and youth coming together to
improve outcomes. Child Welfare, 89(2), 21-38. Available at: http://buildingbridges4youth.org/sites/default/files/Blau%20et%20al_BuildingBridges.pdf (accessed August 4, 2020.) - Breitenstein, S. M., D. Gross, L. Fogg, A. Ridge, C. Garvey, W. Julion, and S. Tucker. 2012. The Chicago parent program: Comparing 1-year outcomes for African American and Latino parents of young children.
Research in Nursing & Health, 35(5), 475-489. https://doi.org/10.1002/nur.21489 - Bridge, T. J., E. G. Massie, and C. S. Mills. 2008. Prioritizing cultural competence in the implementation of an evidence-based practice model. Children and Youth Services Review, 30(10), 1111-1118. https://doi.org/10.1016/j.childyouth.2008.02.005
- Briggs, R. D. 2016. Integrated early childhood behavioral health in primary care: A guide to implementation and evaluation. Switzerland: Springer International Publishing.
- Briggs, R. D., E. J, Silver, L. M. Krug, Z. S. Mason, R. D. A. Schrag, S. Chinitz, and A. D. Racine. 2014. Healthy steps as a moderator: The impact of maternal trauma on child social-emotional development. Clinical
Practice in Pediatric Psychology 2(2), 166-175. https://doi.org/10.1037/cpp0000060 - Bureau of Labor Statistics (BLS). U.S. Department of Labor. 2015. Occupational outlook handbook. Available at: http://www.bls.gov/ooh/Community-and-Social-Service/Social-workers.htm#tab-6 (accessed October 26, 2016).
- Centers for Disease Control and Prevention (CDC). 2016. Ambulatory care use and physician office visits. Available at: http://www.cdc.gov/nchs/fastats/physician-visits.htm (accessed November 18, 2016).
- Center for Health Care Strategies, Inc. (CHCS). 2012. Medicaid financing for family and youth peer support: A scan of state programs. Available at: http://www.chcs.org/resource/medicaid-financing-for-family-and-youth-peer-support-ascan-of-state-programs-3/ (accessed November 18, 2016).
- Cheung, A. H., R. A. Zuckerbrot, P. S. Jensen, K. Ghalib, D. Laraque, and R. E. Stein. 2007. Guidelines for adolescent depression in primary care (GLAD-PC): Treatment and ongoing management. Pediatrics, 120(5),
1313-26. https://doi.org/10.1542/peds.2006-1395 - Committee on Children With Disabilities. 2001. Technical report: The pediatrician’s role in the diagnosis and management of autistic spectrum disorder in children. Pediatrics, 107(5). https://doi.org/10.1542/peds.107.5.1221
- Committee on Pediatric Workforce. 2013. Pediatrician workforce policy statement. Pediatrics, 132(2), 390-397. https://doi.org/10.1542/peds.2013-1517