familyPower: A Referral-Based Pediatric Obesity Treatment Program that Connects Clinic to Family
Introduction
Overweight and obesity, and their negative sequelae, have become the focus of policy makers, business leaders, health care systems, and the general public in the United States and globally. Currently, one in three children and adolescents in the United States is either overweight or obese (Ogden et al., 2014). Children who are overweight or obese tend to remain as such into adulthood, increasing their risk of developing associated chronic conditions, such as type 2 diabetes, cardiovascular disease, nonalcoholic fatty liver disease, and other cardio-metabolic problems (Slomski, 2014). Further, more research is suggesting an important link between physical and mental health, with similar risk factors between obesity and chronic disease (e.g., unhealthy diet, physical inactivity, poor sleep) and many mental disorders, such as depression, anxiety, and attention deficit hyperactivity disorder (ADHD).
Obesity is a major driver of current health care expenditures. Current estimates range from $147 billion to nearly $210 billion per year (Cawley and Meyerhoefer, 2012). Medical costs are often higher for patients who are overweight or obese. For example, costs for providing emergency room care to a patient presenting with chest pains are 28 percent higher for obese patients and 22 percent higher for overweight patients compared to those of normal weight (Peitz et al., 2014).
During the past 2 decades, the prevalence of obesity among children steadily increased (Fryar et al., 2014). From 1976 to 1980, the prevalence of obesity was 5 percent among 2- to 5-year-olds, 6.5 percent among 6- to 11-year-olds, and 5 percent among 12- to 19-year-olds. A decade later, in 1999–2000, prevalence more than doubled for all age groups to 10.3 percent, 15.1 percent, and 14.8 percent, respectively. Another 10 years later, in 2009–2010, the prevalence of obesity continued to increase, albeit at a slower rate, to 12 percent for 2- to 5-year-olds, 18 percent for 6- to 11-year-olds, and 18.4 percent for 12- to 19-year-olds.
Recent national surveys, however, have indicated that obesity prevalence may be leveling off among certain age groups, in particular young children ages 2 to 5 years of age. Recently, the Centers for Disease Control and Prevention (CDC) reported that 18 states and 1 territory experienced statewide declines in the prevalence of obesity among low-income children ages 2–5 years between 2008 and 2011 (CDC, 2013). Less promising, this progress has come at the same time as an increased prevalence among both male and female adolescents ages 12 to 19.
However, despite the overwhelming recognition of obesity as a critical economic and public health issue, and the top child health concern of parents (C.S. Mott Children’s Hospital, 2015), researchers, policy makers, and public health and health care practitioners continue to search for the most effective and sustainable interventions to address the issue. A variety of sectors have a stake in solving the obesity epidemic. As such, solutions will require engagement from a wide range of actors, such as public health, health care, business and industry, education, agriculture and the food industry, transportation and urban planning, philanthropy, the nonprofit sector, and academia, as embodied by the Roundtable on Obesity Solutions (http://nationalacademies.org/hmd/Activities/Nutrition/ObesitySolutions.aspx (accessed April 26, 2016)) of the National Academies of Sciences, Engineering, and Medicine.
Childhood Obesity in Minnesota
In Minnesota, roughly 1 in every 5 students in the ninth grade, or 22 percent, is either overweight or obese (Minnesota Department of Education et al.,n.d.). This figure has remained stable since 2007. Among low-income children between 2 to 5 years old, obesity prevalence has declined since 2000 from 13.1 percent to 12.6 percent (Trust for America’s Health, 2015). However, this figure is still higher compared to the majority of other states. A considerable gender gap also exists among Minnesota children, with males continuing to be more than twice as likely to be overweight or obese compared to their female classmates. However, high school males often underestimate their perceived weight status compared to their actual weight status (Minnesota Student Survey Interagency Team, 2013b). In other words, many overweight or obese high school males often perceive themselves to be of normal weight. Among ninth grade boys in Anoka County, for example, there is an 11 percentage point difference between the prevalence of overweight and obesity and perceived overweight or obesity. Conversely, the trend is the opposite among females, who tend to overestimate their perceived weight status compared to their actual weight status.
Unhealthy behaviors linked to overweight and obesity are also common among Minnesota teens, such as limited fruit and vegetable intake, sugar-sweetened beverage (SSB) consumption, and insufficient physical activity (Minnesota Department of Education et al., n.d.). For example, less than 20 percent of Minnesota ninth graders report consuming five or more servings of fruit, fruit juice, or vegetables the previous day (Minnesota Department of Health and Healthy Minnesota Partnership, 2012). Similarly, only about half of ninth grade students report being physically active for 30 minutes or more in 5 of the previous 7 days (Minnesota Department of Health and Healthy Minnesota Partnership, 2012). This figure has remained relatively stable since 1998.
Treatment of pediatric obesity is unlikely to be successful when clinical approaches do not involve parents or consider the family situation (Sung‐Chan et al., 2013). However, the challenges associated with connecting the clinical interactions between the physician, child, and parents with the family context in addressing obesity are complex. Useful case examples of how clinical efforts can support family-based approaches to treat pediatric obesity are scarce. This discussion paper offers an example in this area and describes the experiences of a pediatric obesity treatment pilot program implemented as part of collaboration between two health care systems in Minnesota. We take a case study approach, analyzing the program using the PIPE Impact Metric, and discussing several strategic and implementation challenges to inform the need for new and innovative models of care and population health.
A Partnership Model to Address Community Needs
The Affordable Care Act (ACA) provided the impetus for health care organizations to reevaluate their care delivery models, particularly in how to elevate prevention and better manage chronic diseases. Much of this shift has stemmed from increased recognition of the limits of clinical interventions to promote health. A wide body of public health research supports the notion that the majority of factors influencing health are beyond the walls of the clinic. These nonclinical factors, known as the social determinants of health, also strongly influence the health and developmental trajectory of children and adolescents (Viner et al., 2012). As such, advancing health requires more than disease-oriented clinical interventions focused on treatment and management (Secretary’s Advisory Committee on National Health Promotion and Disease Prevention, 2010). Instead, health care organizations have the opportunity to improve their care delivery models through the deployment of a more integrated, collaborative team of health care professionals, such as dieticians, nurse practitioners, social workers, psychologists, and health coaches (Dietz et al., 2015). Further, partnership opportunities exist across health systems to improve population health outcomes.
One area ripe for collaboration is in the area of care delivery innovation. One such example is the Northwest Metro Alliance, a long-term collaboration between Bloomington, Minnesota-based HealthPartners and Minneapolis based Allina Health that is focused on achieving the Triple Aim of health care (high-quality care, exceptional patient experience, and affordability) for more than 300,000 people receiving care from these organizations in the northwestern suburbs of the Minneapolis-St. Paul metropolitan area. The Northwest Metro Alliance, which was launched in 2010, is a learning lab for an Accountable Care Organization (ACO), modeling many of the rules that are being promulgated by the U.S. Department of Health and Human Resources.
familyPower: Treating Pediatric Obesity Through Healthy Lifestyle Coaching
Recognizing pediatric obesity as a major public health risk and potential driver of future health care costs across both health care systems, Allina Health and HealthPartners launched familyPower in 2012 under the Northwest Metro Alliance. (Throughout this paper, “we” refers to the authors, as they represent their respective organizations as part of the Northwest Metro Alliance.) The familyPower program is a free, voluntary, family-based health coaching referral program to promote healthy behaviors and treat obesity among children 5 to 12 years old. At the time it was launched, providers saw a clear need for patient and family resources to help address this expanding health issue. As part of their regular assessment of patients for obesity (Barlow, 2007), an increasing number of children were presenting with a body mass index (BMI) in excess of the 85th percentile for age and gender in Anoka County, the primary service area for the Northwest Metro Alliance.
Recent data from Anoka County reinforce this observation and underscore the need for early intervention. Among eighth graders in Anoka County, 22 percent of males and 18 percent of females were overweight or obese in 2013 (Minnesota Student Survey Interagency Team, 2013a). Most concerning, however, is an increasing prevalence of overweight and obesity between grades 8 and 11. This trend is particularly clear among males, with prevalence increasing 5 percentage points during this time period from 22 percent to 27 percent (Minnesota Student Survey Interagency Team, 2013a). Many of these pediatric patients also had diagnosed comorbidities.
Despite the clear demand, however, a program or resource did not exist to refer patients to, and providers themselves did not have either the time or the skill set required to help the children and their parents or guardians make meaningful and sustainable lifestyle changes. After constructing an advisory panel of representatives from both organizations, including pediatricians, clinic leadership, and behavior change experts, the group developed a pilot program that would meet the immediate need of pediatricians and the long-term need of children and their families. Program development began in January 2012, and familyPower became operational in August 2012. The initial pilot spanned 3 years (2012–2015), and following commitment from both Allina Health and HealthPartners, the program is planned to continue through 2017.
Key Programmatic Elements
Referral Based
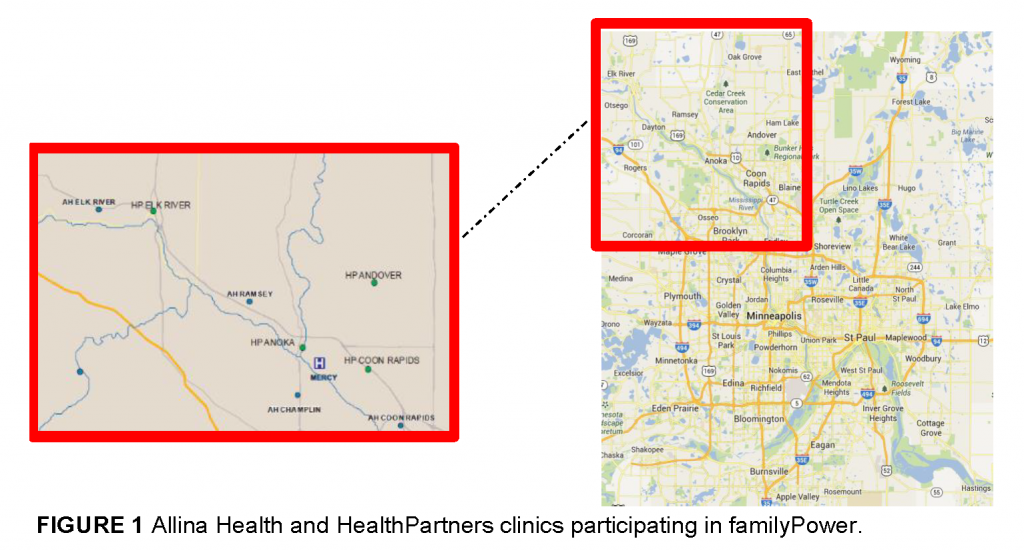
The familyPower program was designed to leverage the unique role of health care providers and apply known evidence-based behavior change concepts to support the adoption of several key healthy behaviors. The program was launched in cooperation with one Allina Health clinic (Coon Rapids, Minnesota) and one HealthPartners clinic (Andover, Minnesota). Since, the program has expanded to include three additional HealthPartners clinics and three additional Allina Health clinics in the northwest metro region outside of Minneapolis for a total of eight current referring clinics (Figure 1).
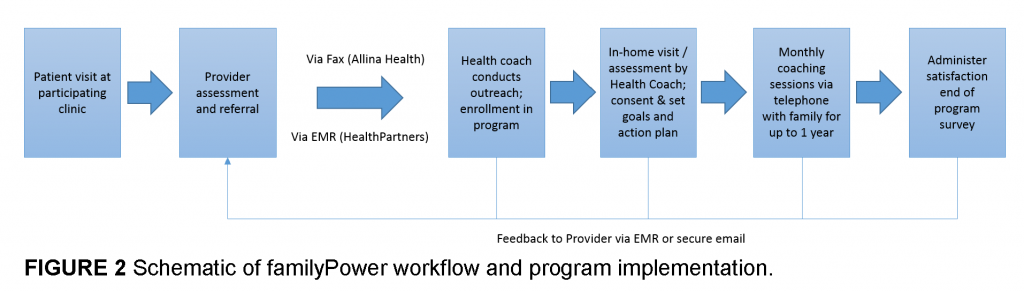
The program’s workflow initiates with a care provider referral. Because familyPower involves two separate health systems, referral mechanisms are unique to each health system to ensure privacy and protection of personal health information. For one system, referrals are made directly through the electronic medical record (EMR). The health coach subsequently receives the referral electronically via secure email within the organization’s firewall. The other health system uses a fax-based system, with the necessary patient and parent information being faxed directly to the health coach. The health coach subsequently provides feedback to the referring provider throughout the process, from outreach to program completion or termination, to inform future care to ensure patient satisfaction, quality of care, and health outcomes—the Triple Aim (Pronk et al., 2013). In essence, the health coach acts as an extension of the care team, with training in public health, psychology, and behavior change. With more patient interaction time than in a clinical setting, the health coach is better positioned to consider and address a patient’s lifestyle, environment, and other social determinants of health. Figure 2 depicts a schematic of the workflow.
Family and Home Based
The familyPower program uses a one-on-one family- and home-based coaching approach to encourage healthy behavior change. After a referral, the health coach then conducts up to three outreach phone calls, the first of which occurs within 1 to 2 business days of the referral. During these outreach calls, the health coach explains the program to the parent or guardian, answers questions, determines if the family would like to enroll, and schedules an initial in-home coaching session and assessment.
Coaching is offered for up to 1 year, free of charge, and is conducted in-person for the first 1 to 3 sessions, followed by telephonic or virtual (e.g., Skype or email) encounters thereafter. In-person sessions are typically conducted in the family’s home, but families also have the option to meet at their clinic. The frequency of coaching encounters is variable and determined by each family’s preferences. Health coaching is offered for the entire family, recognizing the importance of familial support in modeling healthy behaviors and creating an enabling environment for sustainable behavior change (Bandura, 2001).
The home-based nature of the coaching allows the health coach to experience and consider a wider variety of factors that might otherwise go unnoticed through a telephonic or virtual consultation. The home visit provides the health coach the opportunity to observe the family’s physical home environment: is it a single-family home or an apartment, are there nearby recreation areas and grocery stores, and are sidewalks are available. The health coach also evaluates the family’s psychosocial environment and the family’s readiness to address different health behaviors. Such understanding is key to the health coach being able to contextualize the social determinants influencing the health of the child and tailor the coaching accordingly.
Combining Lifestyle Medicine and Coaching for Behavior Change
Health coaching is personalized, with a focus on identifying unique obstacles and challenges to healthy behavior adoption and using motivational interviewing techniques to promote intrinsic motivation and self-efficacy. After obtaining written consent from the parent or guardian during the first session, the health coach conducts an assessment of current obesity-related health behaviors and environmental factors to identify challenges and elucidate areas for specific behavior change goals. Subsequent sessions focus on incrementally identifying and assessing actionable steps to achieve individual goals. This type of tailored approach “meets individuals where they are.” Goals are incremental to allow families to build momentum in their self-confidence. The goal is to help steer families down a particular path while allowing them to determine the pace. In essence, “Successful coaching takes place when coaches apply clearly defined knowledge and skills so that clients mobilize internal strengths and external resources for sustainable change” (Jordan et al., 2015).
The familyPower program uses coaching to facilitate behavior change because of the strong evidence demonstrating intrinsic motivation and self-efficacy as key factors for behavior modification. This has been shown across a wide variety of social science disciplines (Ryan and Deci, 2000). Weight loss outcomes in particular have been found to be strongly linked to self-efficacy (Burke et al., 2015; Byrne et al., 2012; Linde et al., 2006). Further, research has also shown perceived self-efficacy among adolescents to predict adoption of healthy behaviors, such as physical activity (Park and Kim, 2008).
Health and wellness coaching has become increasingly common in primary care and community-oriented public health programming. Today’s major public health challenges—whether this refers to obesity prevention or chronic disease management—are complex in their etiology and interventions, often requiring environmental approaches complemented by individual-based behavior change. Health care organizations have embraced this notion, recognizing the need to link clinical care with community interventions to improve individual and population health. Health coaches are well versed in the science of major public health issues, but artfully apply counseling, motivational interviewing, and other psychological techniques to identify individual or environmental barriers to optimal health and well-being, and support clients in achieving self-determined goals.
Healthy Behavior Focus
Though weight is the primary health outcome of interest, familyPower’s focus is to promote adoption or strengthening of weight-related health behaviors. The program uses the 5-2-1-0 framework as an overarching model for goal setting and behavior change, simultaneously targeting multiple weight-related behaviors. A recent review by Seburg et al. (2015) found this type of a multipronged approach to be a key element of primary-care-based childhood obesity prevention and treatment interventions. The 5-2-1-0 framework encourages the adoption of healthy behaviors related to healthy eating, physical activity, and screen time. It encourages five or more servings of vegetables and fruit per day; 2 hours or less of screen time per day, including television, computer, smartphones, and video games; 1 of more hours of active play per day; and zero sugary drinks. Families also receive a tracker, a tool used both to monitor progress and for accountability, another important element of successful obesity prevention and treatment interventions. Coaching is then tailored within the 5-2-1-0 framework, identifying unique challenges, goals, and action steps.
Framework to Guide Program Design and Evaluation
Considering the practice-based context in which the familyPower program is being implemented, we applied a framework created in the practice setting at our organizations to the logic of program design and evaluation (Pronk, 2003). We used the four S’s of program design—size, scope, scalability, and sustainability—to design the program. We use the Penetration, Implementation, Participation, and Effectiveness (PIPE) Impact Metric to evaluate the program. The two represent a framework organized around a few, critical features of program design and evaluation variables that are linked so as to provide opportunities for improvement based on feedback.
Using the four S’s and the PIPE Impact Metric framework, we analyzed familyPower’s program design and implementation phases to assess its strengths, limitations, and its potential effect upon the community.
The four S’s of program design are defined as follows:
- (Effect) size—The magnitude, extent, relative aggregate amount, or dose of the intervention that affects the user, thereby creating the desired outcome
- Scope—The range of program operations and activities
- Scalability—The ability of a program to grow or expand to accommodate increasing reach or demand of that program
- Sustainability—The long-term, ongoing support for a program that generates revenue or benefits through a predictable supply of requisite inputs: time, money, and human resources
The elements of the PIPE Impact Metric—penetration, implementation, participation, and effectiveness—each represent an equally important aspect of program activation. These four elements can be further divided into two groupings. Penetration and implementation focus on the investment required to bring a program to a user; whereas, participation and effectiveness reflect the extent to which the program meaningfully engages users to achieve the desired outcome. Combined, these elements shed light on potential program impact. The four elements are defined as follows:
- Penetration—The proportion of the target population reached with invitations to engage in the program or intervention
- Implementation—The degree to which the program has been implemented according to its design specifications and work plan
- Participation—The proportion of individuals who enroll in the program according to the program protocol
- Effectiveness—The rate of successful participations, with success defined in the original design phase of the intervention and linked to an anticipated health benefit
The Four S’s Applied to familyPower: Program Design and Analysis
(Effect) Size
Effect size is considered in the context of the goals and objectives of the familyPower program: (1) the promotion of health behaviors and (2) the treatment of excess weight. As such, effect size is applied to data that reflects the impact on behavioral outcomes considered by the program, such as physical activity, healthy eating, screen time, and self-efficacy. In addition, we were interested in changes in weight status as measured by BMI.
Scope
The scope of familyPower includes a set of tools and services for creating benchmark, goalsetting, education, action, and accountability.
- Benchmarking —A standardized assessment is completed at four time intervals: during the home visit (i.e., enrollment), 6 months into the program, 12 months into the program, and again at 6 months after program completion (18 months from enrollment). Constructs include self-reported biometric information; previous weight loss intention and success; behavior patterns related to nutrition, physical activity, and screen time; and self-efficacy. The assessment was designed to evaluate how the family is doing with meeting the 5-2-1-0 behaviors and how the health coaching is affecting their ability to meet these goals over the course of their time in the program.
- Goal-Setting, education, and action planning—The program’s health coach is integral to its success and effectiveness. This individual is responsible for program management, education with families on obesity-related topics, and conducting in-person and telephonic or virtual coaching to set goals and develop individualized action plans in partnership with families. Where appropriate, the coach also serves as a connector to other community resources. Coaching sessions usually occur monthly, though the intervals are based on the preference of the family, and are 15–90 minutes in duration. Typically, the first few sessions are more in-depth because of the importance of establishing trust between the health coach and family and establishing achievable goals from the outset. Subsequent sessions are by phone or email and often decline in duration once an action plan has been established. Goal setting is iterative, identifying positive, attainable steps throughout the program based on the families’ unique circumstances, challenges, and readiness, and building on each other as the family develops confidence and progresses through the program. Sessions are conducted with one or both parents and the child. Families also receive weekly health tips via email on healthy eating, physical activity, and screen time.
- Tracking and accountability—During the initial in-home session, each family receives a weekly tracker, a tool designed to assess progress and achievement of the 5-2-1-0 behaviors on a daily, weekly, and annual basis. Families can also customize the tracker by adding their own unique goals within the overarching 5-2-1-0 framework. The tracker provides accountability for families in their efforts to modify behaviors, as well as a feedback mechanism for both the health coach and family. For the coach, feedback informs future coaching and goal-setting activities. For the family, the tracker provides a mechanism to prioritize behavior changes and build self-efficacy through successful achievement of goals.
- Care coordination—Through the time a family is enrolled in familyPower, the health coach provides regular feedback to their provider through EMR or email to help inform future care.
- Training—familyPower also aims to build the knowledge base among pediatricians in public health and lifestyle factors that influence clinical chronic disease and obesity treatment, management, and care.
Scalability
The scale of the project was defined up front based on resources available. The familyPower program was intentionally integrated into clinical care delivery to bring public health resources as close to the provider as possible. As such, scalability within existing referral clinics is influenced by successful screening and marketing to enroll eligible patients into the program.
The future scalability of familyPower is dependent upon a number of factors. First, its expansion or modifications will be linked to the learnings from this case study, alongside the continuous feedback and input from providers, community partners, and the program’s advisory committee. Second, scalability is also constrained by availability of dedicated financial and human resources for the project, especially, but not limited to, the area of health coaching. Third, the formal collaboration between HealthPartners and Allina Health is only for the Twin Cities northwest metropolitan area, rather than the entire service areas of both health systems. However, both health systems present considerable opportunities to replicate the program in other locations. At present, only four of Allina Health’s 90 clinics and four of HealthPartners’ 55 primary care clinics refer patients to the familyPower program. Lastly, familyPower relies on a home-based, one-on-one coaching model as its primary intervention. Though effective in some cases, such an approach is resource intensive on the part of the health coach compared to other technology-based behavior change strategies, such as text messaging or mass media. Hence, scalability issues and concerns need to consider creative use of human resources and the optimal deployment of technology.
Sustainability
The referral-based design of familyPower offers a sustainable delivery model that leverages the unique role of health care institutions and pediatricians. First, families and individuals still recognize health care providers as trusted community institutions and important sources of health information. This remains true despite the proliferation of Internet health information sources (Hesse et al., 2005). Second, children and parents often develop a long-term relationship with their pediatrician or health care provider. As stated in recent American Academy of Pediatric guidelines, this unique relationship allows providers to follow children over a long period of time, sometimes from fetal life through college, giving them a unique long-term perspective in preventing chronic conditions such as obesity (Daniels et al., 2015). Allina Health and HealthPartners have also incorporated routine clinical screening measures, such as height, weight, and BMI, to inform this longitudinal perspective. Based on data collected over time, pediatricians can then assess obesity risk in accordance with the U.S. Preventive Services Task Force (2010) guidelines that recommend clinicians screen children aged 6 years and older for obesity. Third, by providing regular feedback to providers regarding the progress of clients, the familyPower health coach can inform future clinical intervention and care (Yun et al., 2015). However, a key contingency for sustaining familyPower is the institutional commitment by Allina Health and HealthPartners to continue its formal collaboration and to financially support the administration of the program. This also relates to the future of ACOs and the potential of newly introduced ideas such as the Accountable Health Communities.
Program Impact Analysis Using the PIPE Impact Metric
Penetration
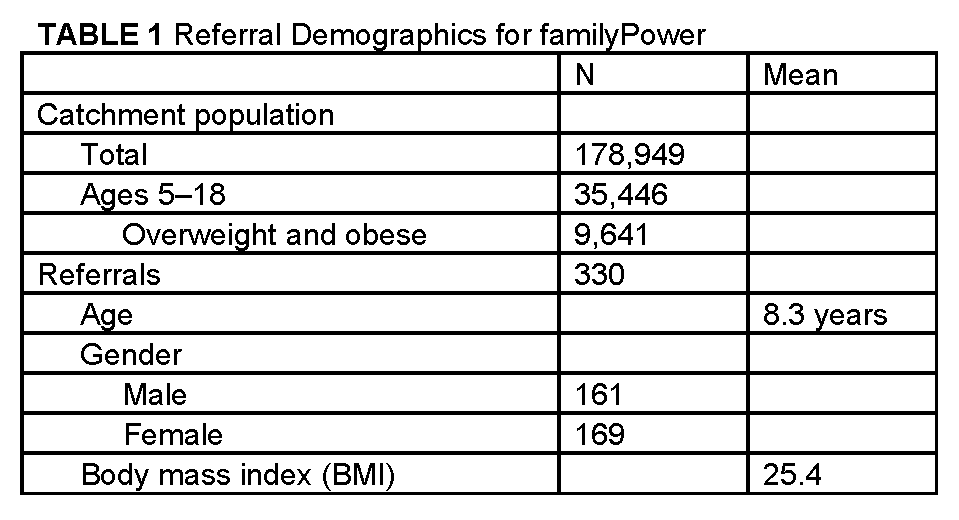
To assess the penetration of familyPower, we assessed total referral volume within the context of the total and pediatric populations in the cities with familyPower referring clinics. According to 2010 Census data, the total population of the six Minnesota cities with familyPower-referring clinics was 178,949, with about 35,446 children aged 5 to 18 years old, roughly 20 percent. Though this pediatric composite includes a broader age range compared to the age criteria for familyPower and does not account for individuals who may access health care in a city different than the one in which they reside, this figure provides a rough estimate of the potential service area for familyPower. Using the statewide prevalence of overweight and obesity among children ages 11 to 17 (27.2 percent), we estimate the total number of eligible individuals for familyPower to be 9,641 (Table 1).
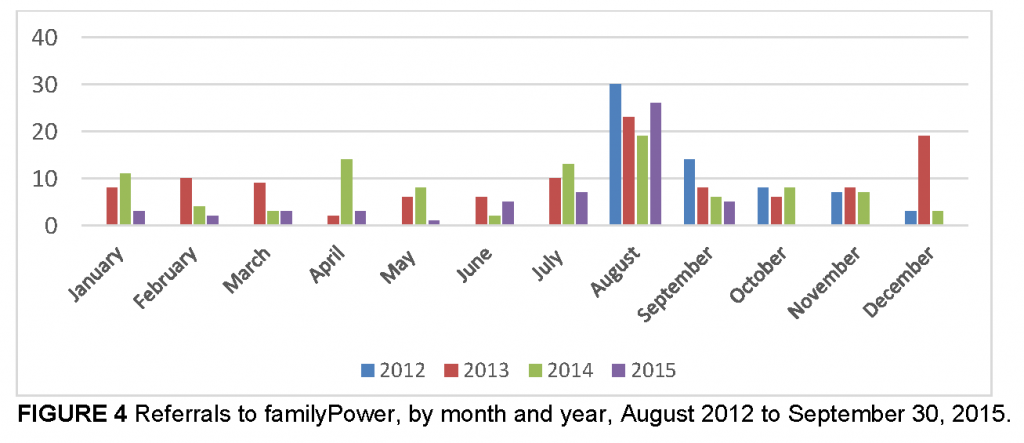
Between August 2012 and September 30, 2015, a total of 330 referrals were made for familyPower, representing 3.42 percent of all overweight and obese children and adolescents 5 to 18 years old in the program’s primary catchment area (Table 1). Referrals peaked in 2013, at 115, the first full year of the program (Figure 3). Referrals then decreased slightly from 2013 to 2014. The mean age of children referred into familyPower was 8.3 years; they had a mean BMI of 25.4; and there were roughly equal numbers of males and females (Table 1).
Referral volume varies considerably by month (Figure 4). The summer months, particularly July and August, are the most common month for familyPower referrals. This clustering of referrals might be explained by the high proportion of well-child visits during this time because school is not in session.
The familyPower program was launched in August 2012 with two original referring clinics, one HealthPartners and the other Allina Health (Figure 5). As the program evolved over the ensuing 3 years, additional clinics were added to the program, and they referred a considerable case volume. These clinics are denoted as Clinics 3 through 8 in Figure 5. Though the program now includes eight total referring clinics, there is considerable variability in size and number of pediatricians across all eight clinics, which influences the referral volume from each. The majority of referrals throughout the life of the program, however, came from the two original clinics, underscoring the importance of building relationships with providers.
Implementation
The familyPower program model was adapted from a previous pilot study by the HealthPartners Institute that tested a primary care-based health coaching intervention for children ages 5 through 10 years of age with a BMI in the 95th percentile or above (Sherwood et al., 2013, 2015). With the input from an advisory panel consisting of pediatricians, clinic managers, behavior change experts, health researchers, and community stakeholders, the program was created as a pilot to try, test, and change program components as needed. The initial design phase lasted approximately 6 months, beginning in March 2012. This included hiring a health coach/program manager, establishing the operating budget, training providers, and collateral material development. The first referral was made in August 2012.
The following components were integral to the program’s design and implementation:
- Creation of the health coach/program manager position, including determining the requisite competencies, writing a job description, hiring, and onboarding. While the position was funded by and managed by both organizations, one acted as the employment agent.
- Determination of the operational budget, including personnel, legal assistance, and technology development.
- Integration of the program into clinic workflows for each organization. This included determining feasible and effective referral processes and feedback mechanisms.
- Development of monitoring and evaluation tools, including the behavior change questionnaire and satisfaction survey.
- Development of an evidence-based health coaching methodology suitable for the specific target population.
- Development of branding and other marketing materials. This was done in collaboration with branding experts within HealthPartners to develop a name and logo for the program, which reflected the psychosocial impact of obesity on children and their families, and drew upon the program’s aim to connect, encourage, and support families in their journey to adopting healthier behaviors. Marketing materials were subsequently developed and distributed to clinic staff.
- Development of program materials including consent form, referral fax form, tracker, and educational documents.
Since the program began, these core implementation components have remained constant, with small modifications at various points to improve the program’s effectiveness. First, the eligibility criteria changed in two ways based on feedback from participating pediatricians; the age range expanded to include 12-year-olds, and the BMI threshold was reduced from the 95th percentile to the 85th percentile. Additional program offerings such as group-based coaching, healthy living tips for families with young children via text, and cooking demonstrations were also incorporated.
Participation
Of the 330 total referrals, 117 yielded an initial in-home meeting, representing a conversion rate of 33.8 percent (Figure 6). A total of 675 coaching encounters (i.e., engagements) occurred with the 117 enrolled families, for a mean of almost 6 coaching encounters per enrolled family. The number of coaching encounters ranged between 1 and 34, and 26 families received 10 or more coaching encounters.
Effectiveness
To assess familyPower’s effectiveness as a pediatric obesity lifestyle modification intervention, we analyzed health behavior data for 26 families. These data were collected at regular intervals during the program: enrollment, 6 months, 12 months, and 6 months after program completion. Of the 117 total families who enrolled in familyPower at some point between August 2012 and September 2015, we only included families with two or more completed questionnaires to analyze temporal changes (n=26). We also assessed changes in voluntary, self-reported weight status during the program, and contextualized these changes with EMR-based BMI data at the time of enrollment and current BMI. Changes in weight status was determined using a subset of the program (n=13).
Of the 26 families, 17 (65 percent) reported having tried to lose weight in the past. The mean BMI of participants was 25.8 at enrollment. Families tried a variety of strategies to lose weight, including increased leisure-time physical activity; incorporating more fruits and vegetables; dining out less; reducing screen time; and replacing high-sugar foods and beverages with healthier alternatives.
During the course of the 1-year program, the largest number of families reported improvements in daily fruit and vegetable consumption, daily sugar-sweetened beverage (SSB) consumption, enjoyment of physical activity, and self-efficacy (Figure 7a–d). Between enrollment and 6 months, the mean number of daily servings of fruits and vegetables consumed increased from 2.8 servings to 3.5 servings, and half of all families reported an increase in fruit and vegetable consumption during the program. Likewise, rating of perceived enjoyment of physical activity increased among 38 percent of families. On a scale of zero to 10 (with 10 being the highest), mean rating of perceived enjoyment of physical activity increased from 7.1 to 7.9. Previous research among children has shown physical activity enjoyment to be a key predictor of physical activity (DiLorenzo et al., 1998). Mean daily SSB consumption decreased by 50 percent from 0.8 servings per day to 0.4 servings per day, with 11 of 26 families (42 percent) reporting a decrease in consumption during the program.
Most apparent, however, was the notable increase in self-efficacy reported by families after the program. At the end of the program almost 60 percent of families indicated a greater level of confidence in their ability to make lifestyle changes to improve their health. The mean rating of self-efficacy on a scale of zero to 10 (with 10 being the highest) increased 15 percent from 7.2 to 8.3 between the time families enrolled to program completion.
Lastly, changes in weight status were inconsistent. Of the original sample of 26 families, 13 reported weight status at enrollment and at 6 months and 12 months during the program. Within this subset, seven children experienced an increase in BMI, three experienced a decrease, and three experienced no change (Figure 8a). Using EMRs to compare current BMI and BMI at the time of referral, BMI decreased in 6 individuals (25 percent), increased in 15 individuals (63 percent), and remained the same in 3 individuals (Figure 8b). Two individuals lacked complete data and were excluded from this comparison.
Challenges and Considerations for Future Programming
The familyPower program offers an effective intervention model to promote key health behaviors, such as limiting consumption of SSBs, eating more fruits and vegetables, and building self-efficacy among children and their parents. A considerable research base has identified SSBs and fruit and vegetable consumption as closely tied with obesity and a variety of related chronic diseases, such as type 2 diabetes and cardiovascular disease.
Self-efficacy has also been a well-understood prerequisite for behavior change, particularly for those influencing health. A well-known theoretical framework for self-efficacy and behavior is Bandura’s Social Learning Theory, which suggests behavior change and maintenance to be a function of two variables: (1) the individual’s expectations about their ability to engage in or execute the behavior (i.e., self-efficacy); and (2) expectations about the resulting outcome from engaging in the particular behavior (Strecher et al., 1986). In other words, one must believe a given behavior will lead to a given outcome and believe the given behavior is attainable. A 2015 systematic review of 35 studies that examined self-regulation mediators and successful behavior change in obesity interventions found higher autonomous motivation, self-efficacy, and self-regulation skills best predicted beneficial weight and physical activity outcomes in adults (Teixeira et al., 2015). An earlier 2005 review of factors associated with weight loss maintenance for at least 6 months identified a number of psychosocial factors as being critical, including social support, superior coping strategies, being able to handle life stress, autonomy, assuming responsibility, and self-efficacy (Elfhag and Rössner, 2005).
Other studies point to the critical role of self-monitoring in behavior change and weight loss interventions. A 2009 meta-regression study of effective behavior change techniques to promote healthy eating and physical activity found self-monitoring to be the distinguishing factor among effective interventions compared to ineffective interventions (Michie et al., 2009).
However, to date, the majority of research on behavior change and obesity prevention and treatment has focused on adult populations.
A number of challenges arose during the more than 3 years of implementing familyPower. Such challenges provide important considerations for other clinical- and coaching-based pediatric obesity prevention and treatment interventions and collaborations across health care systems.
Workflow Considerations
Increasing Demands of Providers
Though also a major advantage, using a referral-based mechanism to enroll clients into familyPower puts significant responsibility on pediatricians and health care providers. Initiation of the health coaching component of familyPower relies heavily on the interpersonal skills of providers to effectively communicate with families about overweight and obesity. Though improving, primary care providers have not historically received adequate training in lifestyle interventions to prevent or treat chronic conditions and obesity. For example, in 2009, only 27 percent of U.S. medical schools provided 25 hours or more of nutrition instruction as recommended by the National Academy of Sciences (Adams et al., 2010). European (Chung et al., 2014) and Japanese (Orimo et al., 2013) medical schools are comparable. In many cases, curriculum guidelines exist for nutrition education, yet they often lack mandatory enforcement (Crowley et al., 2015). Current nutrition education predominantly focuses on basic nutrition principles, nutrition assessment, the role of nutrition in health, interdisciplinary teamwork, and the provision of nutrition counseling (Crowley et al., 2015). As a result, fewer than 50 percent of primary care providers in 2011 reported providing specific guidance to patients on diet, physical activity, or weight control (Smith et al., 2011).
Over the past several years medical schools have slowly begun to integrate lifestyle medicine into their curricula, especially in the areas of diet and nutrition. As one example, Tulane University School of Medicine launched a culinary program to teach medical students, residents, doctors, and other care providers about cooking and the role of food in preventing and managing chronic conditions, including obesity (Brannon, 2014; Shanker, 2015). Professional organizations have also stepped up to provide training and other continuing education resources for physicians, such as the American College of Sports Medicine’s Exercise is Medicine initiative (http://www.exerciseismedicine.org/) and the STOP Obesity Alliance’s Why Weight toolkit. (http://www.whyweightguide.org/about-why-weight.php) Further efforts are underway to improve medical school education to better integrate nutrition, physical activity, and other lifestyle factors that strongly influence the current disease burden and major drivers of health care costs in the United States. Launched in 2013, the Lifestyle Medicine Education Collaborative is one such example. It engages medical school deans, medical students, content experts, and representatives of professional associations, government agencies, accreditation agencies, and national assessment boards to integrate “lifestyle medicine,” or the ability of a health care provider to “effectively and efficiently counsel their patients toward adopting and sustaining healthier behaviors” (Polak et al., 2015).
Mental Health, Pyschosocial, and Parenting Considerations
The relationship between mental and physical health is complex and bidirectional. Diagnosed mental disorders, such as depression, anxiety, or ADHD can influence other health behaviors, such as eating habits or physical activity levels, while these same health behaviors can in turn influence the advancement of some mental disorders (Bellisle, 2004). Considerable evidence exists among adult populations; however, more research has been focused on pediatric and adolescent populations (Stavrakakis et al., 2012). A 2013 review, for example, found a small but significant overall effect for physical activity on depression among children and adolescents (Brown et al., 2012). Regular physical activity has also been known to reduce symptoms of anxiety independent of age and health status (Petruzzello et al., 1991) and effectively manage attention disorders, such as ADHD (Reeves and Bailey, 2014).
Likewise, family dynamics and family systems play an important, though often overlooked, role in pediatric obesity risk. A number of studies have linked parenting style with obesity. A recent 2015 study by Kakinami and colleagues (2015) found that preschool- and school-age children with authoritarian (not responsive but demanding) parents were 35 percent more likely to be obese compared to children from authoritative (responsive and demanding) households. A 2011 review supported the relationship between authoritative parenting and healthy behaviors among children, finding that children living in authoritative households tended to eat healthier, were more physically active, and had lower BMI levels compared to children raised with other parenting styles (Sleddens et al., 2011).
When it comes to health coaching, parenting and mental health issues are complex, difficult issues to navigate. Language, word choice, and framing of challenges and solutions all must be considered with care and sensitivity. Adopting an accusatory tone or message or placing blame (whether real or perceived) can quickly create resistance to behavior change on the part of the parent or child.
Though familyPower takes a broad and personalized approach to improving key behaviors related to obesity, related mental or psychosocial issues are at play, but often fall outside the scope of the program. The relationship between health behaviors and mental health was considered during the original development of the program. As such, health coaches with expertise in public health and psychology were sought out.
User Fees and Retention
Though familyPower has been successful in converting referrals into program participants, retention is an ongoing challenge. Only a small percentage have taken advantage of the full year of free health coaching that is offered. A more common scenario is the family that enrolls in the program, but is lost to follow-up after several coaching encounters. One possible explanation could be that familyPower is offered free of charge, subsidized by both Allina Health and HealthPartners. As such, there is no financial commitment for families to use the service, and no perceived downside to discontinuing or dropping out.
Health care user fees have long been debated among health economists. Such debates have focused particularly on low-income populations and the extent to which user fees create additional barriers to health care service utilization. Some argue that removal of such fees (i.e., offering subsidized services) improves service coverage and access, particularly among low socioeconomic populations (McPake et al., 2011). A considerable research base exists involving populations in low- and middle-income countries. A 2011 review by Lagarde and Palmer, for example, found that the introduction of or increase in user fees generally resulted in decreased preventative and curative health care service utilization (Lagarde and Palmer, 2011). However, removal of user fees was found to have no immediate impact on preventive service utilization.
Recent behavioral economics studies, however, suggest financial incentives can play a significant role in changing behavior and achieving health goals. An experiment by John et al. (2011) found that when there was a financial stake for participants to achieve weight loss goals, they were more successful. This draws on broader behavioral economics research by Tversky and Kahnehman (1991) demonstrating the phenomena of loss aversion, which shows losses and disadvantages influence preferences to a greater degree than do gains and advantages. With the goal of losing 24 pounds in 24 weeks, participants in the intervention arm of the study could contribute $0–$3.00 of their own funds to a deposit contract. Throughout the duration of the study, participants whose weight remained the same or decreased received a reward equal to their original daily deposit plus a 1:1 match from the researchers (i.e., participants could earn $84 net per month by making a maximum $3.00 daily deposit).
Systematic reviews of financial incentives (both reward and punitive based) support their short-term efficacy in modifying behavior and achieving weight loss. A systematic review by Purnell et al. (2014) of financial incentives for dietary behavior change found a positive association between the two. Substantial evidence supports the short-term efficacy of financial incentives (both reward and punitive based). However, financial incentives to adopt healthy behaviors often fail to result in sustained behavior change over the long term. A systematic review of financial incentives in treatments for overweight and obesity by Paul‐Ebhohimhen and Avenell (2008) found no significant weight loss or maintenance beyond 12 months. Further, separate research on using financial incentives for discouraging unhealthy behaviors, such as smoking, among children and adolescents show similar limitations (Johnston et al., 2012).
Communication and the Role of Technology
The nature of communication is radically shifting. Current norms, expectations, and preferences regarding communications are dramatically different today than just a decade ago. Technology, including the Internet, email, social media, and smartphones, has shifted how children, teens, and adults communicate and consume information. As of 2014, 90 percent of American adults own a cell phone, 66 percent own a smartphone, and 87 percent use the Internet, and threequarters of these use social networking sites (Pew Research Center, 2014).
The centrality of technology in everyday life is even more prominent among children and teens. Ninety-five percent use the Internet; 80 percent own a cell phone; 80 percent own a desktop or laptop computer; 25 percent own a tablet; and more than 80 percent use social media sites, a roughly 20 percentage point increase from only 6 years ago (Pew Research Center, 2014). For teens, text messaging has become the predominant form of daily communication, more prevalent than phone calling, face-to-face socializing, social network site messaging, and emailing (Lenhart, 2012). A recent study by Kabali et al. (2015), found technology use to be ubiquitous among children as young as 6 months to 4 years old. They found that 97 percent of those they surveyed had used a mobile device, and nearly half of children under the age of 1 year used a mobile device on a daily basis. Mobile device use increased considerably with age, and one-third of 2-year olds did not require any help navigating a mobile device.
Health care providers and public health are trying to keep pace, though they face challenges in doing so. Federal and state laws exist to protect an individual’s health information and govern how health care providers can communicate with their patients. This influenced the original design of familyPower and its communication channels. After primarily relying on in-person and telephone-based communication with families during the first 3 years of the program, other channels, such as secure email, are now being tested. A study conducted by Kaiser Permanente in 2015 found that exchanging secure email messages with a health care provider improved patient experience and reduced potential future costs of care among individuals with chronic conditions (Raths, 2015). Thirty-two percent of patients surveyed said that exchanging email messages with their health care provider improved their overall health, and among patients who had emailed their health care provider, 42 percent reported a reduction in subsequent phone contacts and 36 percent said it reduced in-person visits.
Health care and public health behavior change interventions must continue exploring how to incorporate these changing realities into their communication strategies (CDC, 2015).
This is particularly salient for obesity prevention interventions that focus on screen time. Digital media may be the most effective communication channel to influence behavior, but it also represents a potential risk factor when consumed in excess. Further, children and adolescents increasingly turn to digital media for education, connection, and meaning. As such, any intervention focused on screen time must take this into account, which is reflected in the recently updated American Academy of Pediatrics guidelines on screen time (Brown et al., 2015). Instead of its hardline stance, particularly for children under the age of 2 years, the new guidelines recommend families cultivate a healthy relationship with digital media and screens, recognizing their potential positive contributions, while also setting appropriate boundaries on its use.
Weight Loss or Healthy Behaviors?
An intense focus on weight can be a double-edged sword. On one hand, weight is often used as a proxy for health and related chronic disease risk, such as heart disease and type 2 diabetes. Using this assumption, weight warrants close monitoring. In addition, weight is a convenient and practical feedback metric for individuals seeking to change associated health behaviors, such as diet or physical activity. Weight is routinely measured in the clinical setting, but individuals can also easily track their weight on their own. As such, weight is regarded as an important outcome measure for primary care-based pediatric obesity prevention and treatment interventions (Seburg et al., 2015).
However, too much focus on weight can produce important negative psychosocial consequences, particularly among children and adolescents (Birch and Fisher, 1998). A 2015 study of almost 2,000 adolescents and young adults found that a high amount of self-weighing was associated with decreased body satisfaction and self-esteem (Pacanowski et al., 2015). Previous studies by Killen et al. (1994) and Rosen et al. (1987) found restrained adolescent eaters, such as those trying to lose weight, also exhibited high levels of body dissatisfaction, low self-worth, fear of weight gain, and anxiety. Psychosocial issues, such as body dissatisfaction, can be strong predictors of obesity risk among adolescents (Roberts and Duong, 2015).
Further, positive healthy lifestyle messages tend to resonate the most with parents, whereas weight-based messaging can imply restrictiveness, thereby triggering defensiveness and opposition to behavior change. An overemphasis on weight or BMI can mislead parents about the importance of healthy growth, including muscle mass, and thereby imply the need for a restrictive diet (Lobstein et al., 2015). A diverse diet, on the other hand, has been shown to be optimal for healthy growth in younger children (Lobstein et al., 2015). A study of public perceptions of obesity-related public health media campaigns found that positive message framing, such as encouraging more fruit and vegetable consumption, were most favorable (Puhl et al., 2012). Messages that stigmatized and referenced body weight were least favorable.
Cultivating the Home Environment: Taking a Family-Based Approach
Home-based health promotion and treatment interventions have been found to be effective across a range of ages, including for addressing obesity among pediatric populations. For example, a randomized controlled trial published in 2012 found a home-based intervention to promote healthy feeding practices during pregnancy and 2 years postnatal to be effective in reducing BMI among 2-year-olds (Wen et al., 2007, 2012). However, research on home-based obesity interventions is limited. A 2013 comparative effectiveness review and meta-analysis of childhood obesity prevention interventions conducted by the Agency for Healthcare Research and Quality found few studies focused on home-based interventions (only four studies were identified) and insufficient evidence to support their efficacy (Showell et al., 2013; Wang et al., 2013).
Yet considerable research exists demonstrating the close relationship between parental and child behaviors. Modeled behavior by parents strongly influences subsequent behaviors by their children, particularly around health. For example, a study conducted by Brown and Ogden (2004) of children 9–13 years old and their parents found that modeled parental behaviors related to healthy eating subsequently improved the child’s diet. A review on the topic of social modeling found similar conclusions across more than 60 other experimental studies, supporting an important relationship between modeling and food choice and food intake (Cruwys et al., 2015). Further, other home environment factors have been found to influence diet quality among children and adolescents, including involvement in food preparation at home; eating meals as a family; availability of healthy or unhealthy food options; parenting; family norms, structure, and dynamics; and social modeling (Reicks et al., 2015).
While the home environment is an important influence on childhood development and health, other environments, such as schools, also play a complementary role to shape healthy behaviors. While school is in session, children spend about 40 percent of their waking hours there. This does not account for after-school programming, sports, or other extracurricular activities. Significant improvements have been made within the school setting to promote healthier choices, in part, due to public policy and regulatory efforts related to nutritional standards for school meals (Turner and Chaloupka, 2015), limitations on competitive foods (Taber et al., 2012), and curtailing unhealthy food marketing.
When to Intervene to Promote a Healthy Weight
The link between childhood weight status and subsequent adult weight status and disease risk has been well established. However, childhood weight status is influenced by a variety of factors before, during, and after pregnancy, and throughout early childhood. The “programming” for a child’s risk of overweight and obesity, therefore, may occur well before 5 years of age, the minimum age criteria for familyPower. Parental weight status, rapid weight gain during pregnancy, maternal smoking during pregnancy, and cesarean section have all been linked to subsequent overweight and obesity risk during childhood (Li et al., 2013; Ludwig et al., 2013; Von Kries et al., 2002; Yu et al., 2013). Maternal dietary patterns during pregnancy have also been shown to strongly influence subsequent food preferences by the child, and prenatal undernutrition and overnutrition have both been linked to childhood obesity risk (Anzman et al., 2010; Gluckman and Hanson, 2008). Early infant feeding practices, including breastfeeding, initiation of complementary feeding, and transition to an “adult” diet all can influence subsequent obesity risk (Anzman et al., 2010; Arenz et al., 2004).
This mounting evidence demonstrating the strong influence of pregnancy and early childhood on subsequent obesity risk suggests a potential role for health care providers. Proactive intervention before age 5 targeting the mother, child, or both could alter subsequent obesity risk. Given the limited efficacy and resource requirements for weight loss interventions later in life, a greater focus on pregnant women and early childhood could prove influential in changing the course of childhood obesity. Such benefits were observed in a recent study of low-income, preschool-aged children, which found statistically significant downward trends in obesity prevalence from 2008 to 2011 in 18 states and the U.S. Virgin Islands, in part due to nutritional standard improvements in the Special Supplemental Nutrition Program for Women, Infants and Children (WIC) and population-level increases in breastfeeding (CDC, 2013).
Conclusion
Overweight and obesity, particularly among children and adolescents, represent a serious threat to population health, the health care system, our community and societal health, and our national and global economy. Many believe them to be the primary drivers for why the current generation of children in the United States will have a shorter life expectancy than their parents. The familyPower program is an example of a referral-based, family-based health coaching program designed to address the determinants of overweight and obesity among children and a means to promote a necessary precondition for behavior modification that is starting to generate success. It also represents a model for how competing health care organizations can collaborate to achieve the Triple Aim, and it illuminates a number of implementation challenges other health care organizations might consider as they explore a strengthened clinic–community connection and their role in helping solve the obesity crisis.
Download the graphic below and share it on social media!
References
- Adams, K. M., M. Kohlmeier, and S. H. Zeisel. 2010. Nutrition education in US medical schools: Latest update of a national survey. Academic Medicine: Journal of the Association of American Medical Colleges 85(9):1537. https://doi.org/10.1097/ACM.0b013e3181eab71b
- Anzman, S. L., B. Y. Rollins, and L. L. Birch. 2010. Parental influence on children’s early eating environments and obesity risk: Implications for prevention. International Journal of Obesity 34(7):1116-1124. https://doi.org/10.1038/ijo.2010.43
- Arenz, S., R. Rückerl, B. Koletzko, and R. von Kries. 2004. Breast-feeding and childhood obesity—A systematic review. International Journal of Obesity 28(10):1247-1256. https://doi.org/10.1038/sj.ijo.0802758
- Bandura, A. 2001. Social cognitive theory: An agentic perspective. Annual Review of Psychology 52(1):1-26. https://doi.org/10.1146/annurev.psych.52.1.1
- Barlow, S. E. 2007. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: Summary report. Pediatrics 120(Suppl 4):S164-S192. https://doi.org/10.1542/peds.2007-2329C
- Bellisle, F. 2004. Effects of diet on behaviour and cognition in children. British Journal of Nutrition 92(S2):S227-S232. https://doi.org/10.1079/BJN20041171
- Birch, L. L., and J. O. Fisher. 1998. Development of eating behaviors among children and adolescents. Pediatrics 101(Supplement 2):539-549. Available at: https://pubmed.ncbi.nlm.nih.gov/12224660/ (accessed July 20, 2020).
- Brannon, K. 2014. Tulanes’ new teaching kitchen cooks up lessons in ‘culinary medicine’. Available at: http://tulane.edu/news/releases/tulane-teaching-kitchen-cooks-up-lessons-in-culinarymedicine.cfm (accessed April 26, 2016).
- Brown, A., D. L. Shifrin, and D. L. Hill. 2015. Beyond ‘turn it off’: How to advise families on media use. AAP News 36(10):54-54. https://doi.org/10.1542/AAPNEWS.20153610-54
- Brown, H., N. Pearson, R. Braithwaite, W. Brown, and S. Biddle. 2012. Physical activity interventions and depression in children and adolescents: A systematic review and meta-analysis. Journal of Science and Medicine in Sport 15:S343. https://doi.org/10.1016/j.jsams.2012.11.834
- Brown, R., and J. Ogden. 2004. Children’s eating attitudes and behaviour: A study of the modelling and control theories of parental influence. Health Education Research 19(3):261-271. https://doi.org/10.1093/her/cyg040
- Burke, L. E., L. J. Ewing, L. Ye, M. Styn, Y. Zheng, E. Music, J. Mancino, C. C. Imes, L. Hu, and R. Goode. 2015. The SELF trial: A self‐efficacy‐based behavioral intervention trial for weight loss maintenance. Obesity 23(11):2175-2182. https://doi.org/10.1002/oby.21238
- Byrne, S., D. Barry, and N. M. Petry. 2012. Predictors of weight loss success. Exercise vs. dietary self-efficacy and treatment attendance. Appetite 58(2):695-698. https://doi.org/10.1016/j.appet.2012.01.005
- C. S. Mott Children’s Hospital. 2015. Top 10 child health problems. National Poll on Children’s Health 24(3). Available at: https://mottpoll.org/reports-surveys/top-10-child-health-problems-more-concern-sexting-internet-safety (accessed July 20, 2020).
- Cawley, J., and C. Meyerhoefer. 2012. The medical care costs of obesity: An instrumental variables approach. Journal of Health Economics 31(1):219-230. https://doi.org/10.1016/j.jhealeco.2011.10.003
- CDC (Centers for Disease Control and Prevention). 2013. Vital signs: Obesity among low-income, preschool-aged children—United States, 2008-2011. Morbidity and Mortality Weekly Report 62(31):629. Available at https://www.cdc.gov/mmwr/preview/mmwrhtml/mm6231a4.htm (accessed July 20, 2020).
- CDC. 2015. Quickstats: Percentage of U.S. adults who looked up health information on the Internet in the past year, by type of locality— National Health Interview Survey, 2012–2014. Morbidity and Mortality Weekly Report 64(49):1367. Available at: https://www.cdc.gov/mmwr/preview/mmwrhtml/mm6449a5.htm?s_cid=mm6449a5_w (accessed July 20, 2020).
- Chung, M., V. van Buul, E. Wilms, N. Nellessen, and F. Brouns. 2014. Nutrition education in European medical schools: Results of an international survey. European Journal of Clinical Nutrition 68(7):844-846. https://doi.org/10.1038/ejcn.2014.75
- Crowley, J., L. Ball, C. Laur, C. Wall, B. Arroll, P. Poole, and S. Ray. 2015. Nutrition guidelines for undergraduate medical curricula: A six-country comparison. Advances in Medical Education and Practice 6:127. https://doi.org/10.2147/AMEP.S73711
- Cruwys, T., K. E. Bevelander, and R. C. Hermans. 2015. Social modeling of eating: A review of when and why social influence affects food intake and choice. Appetite 86:3-18. https://doi.org/10.1016/j.appet.2014.08.035
- Daniels, S. R., S. G. Hassink, S. A. Abrams, M. R. Corkins, S. D. de Ferranti, N. H. Golden, S. N. Magge, and S. J. Schwarzenberg. 2015. The role of the pediatrician in primary prevention of obesity. Pediatrics 136(1):e275-e292. https://doi.org/10.1542/peds.2015-1558
- Dietz, W. H., L. S. Solomon, N. Pronk, S. K. Ziegenhorn, M. Standish, M. M. Longjohn, D. D. Fukuzawa, I. U. Eneli, L. Loy, N. D. Muth, E. J. Sanchez, J. Bogard, and D. W. Bradley. 2015. An integrated framework for the prevention and treatment of obesity and its related chronic diseases. Health Affairs (Millwood) 34(9):1456-1463. https://doi.org/10.1377/hlthaff.2015.0371
- DiLorenzo, T. M., R. C. Stucky-Ropp, J. S. Vander Wal, and H. J. Gotham. 1998. Determinants of exercise among children. II. A longitudinal analysis. Preventive Medicine 27(3):470-477. https://doi.org/10.1006/pmed.1998.0307
- Elfhag, K., and S. Rössner. 2005. Who succeeds in maintaining weight loss? A conceptual review of factors associated with weight loss maintenance and weight regain. Obesity Reviews 6(1):67-85. https://doi.org/10.1111/j.1467-789X.2005.00170.x
- Fryar, C. D., M. D. Carroll, and C. L. Ogden. 2014. Prevalence of overweight and obesity among children and adolescents: United States, 1963–1965 through 2011–2012. National Center for Health Statistics. Available at: http://www.cdc.gov/nchs/data/hestat/obesity_child_11_12/obesity_child_11_12.htm (accessed April 25, 2016).
- Gluckman, P., and M. Hanson. 2008. Developmental and epigenetic pathways to obesity: An evolutionary-developmental perspective. International Journal of Obesity 32:S62-S71. https://doi.org/10.1038/ijo.2008.240
- Hesse, B. W., D. E. Nelson, G. L. Kreps, R. T. Croyle, N. K. Arora, B. K. Rimer, and K. Viswanath. 2005. Trust and sources of health information: The impact of the Internet and its implications for health care providers: Findings from the first health information national trends survey. Archives of Internal Medicine 165(22):2618-2624. https://doi.org/10.1001/archinte.165.22.2618
- John, L. K., G. Loewenstein, A. B. Troxel, L. Norton, J. E. Fassbender, and K. G. Volpp. 2011. Financial incentives for extended weight loss: A randomized, controlled trial. Journal of General Internal Medicine 26(6):621-626. https://doi.org/10.1007/s11606-010-1628-y
- Johnston, V., S. Liberato, and D. Thomas. 2012. Incentives for preventing smoking in children and adolescents. Cochrane Database of Systematic Reviews 10. https://doi.org/10.1002/14651858.CD008645.pub2
- Jordan, M., R. Q. Wolever, K. Lawson, and M. Moore. 2015. National training and education standards for health and wellness coaching: The path to national certification. Global Advances in Health and Medicine 4(3):46-56. https://doi.org/10.7453/gahmj.2015.039
- Kabali, H. K., M. M. Irigoyen, R. Nunez-Davis, J. G. Budacki, S. H. Mohanty, K.P. Leister, and R. L. Bonner. 2015. Exposure and use of mobile media devices by young children. Pediatrics peds-2015. https://doi.org/10.1542/peds.2015-2151
- Kakinami, L., T. A. Barnett, L. Séguin, and G. Paradis. 2015. Parenting style and obesity risk in children. Preventive Medicine 75:18-22. https://doi.org/10.1016/j.ypmed.2015.03.005
- Killen, J. D., C. B. Taylor, C. Hayward, D. M. Wilson, K. F. Haydel, L. D. Hammer, B. Simmonds, T. N. Robinson, I. Litt, and A. Varady. 1994. Pursuit of thinness and onset of eating disorder symptoms in a community sample of adolescent girls: A three‐year prospective analysis. International Journal of Eating Disorders 16(3):227-238. https://doi.org/10.1002/1098-108x(199411)16:3<227::aid-eat2260160303>3.0.co;2-l
- Lagarde, M., and N. Palmer. 2011. The impact of user fees on access to health services in low and middle-income countries. Cochrane Database of Systematic Reviews 4(1). https://doi.org/10.1002/14651858.CD009094
- Lenhart, A. 2012. Teens, smartphones and texting. Washington, DC: Pew Research Center. Available at: https://www.pewresearch.org/internet/2012/03/19/teens-smartphones-texting/ (accessed July 20, 2020).
- Li, H., Y. Zhou, and J. Liu. 2013. The impact of cesarean section on offspring overweight and obesity: A systematic review and meta-analysis. International Journal of Obesity 37(7):893-899. https://doi.org/10.1038/ijo.2012.195
- Linde, J. A., A. J. Rothman, A. S. Baldwin, and R. W. Jeffery. 2006. The impact of self-efficacy on behavior change and weight change among overweight participants in a weight loss trial. Health Psychology 25(3):282. https://doi.org/10.1037/0278-6133.25.3.282
- Lobstein, T., R. Jackson-Leach, M. L. Moodie, K. D. Hall, S. L. Gortmaker, B. A. Swinburn, W. P. T. James, Y. Wang, and K. McPherson. 2015. Child and adolescent obesity: Part of a bigger picture. Lancet 385(9986):2510-2520. https://doi.org/10.1016/S0140-6736(14)61746-3
- Ludwig, D. S., H. L. Rouse, and J. Currie. 2013. Pregnancy weight gain and childhood body weight: A within-family comparison. PLoS Medicine 10(10):e1001521. https://doi.org/10.1371/journal.pmed.1001521
- McPake, B., N. Brikci, G. Cometto, A. Schmidt, and E. Araujo. 2011. Removing user fees: Learning from international experience to support the process. Health Policy and Planning 26(Suppl 2):ii104-ii117. https://doi.org/10.1093/heapol/czr064
- Michie, S., C. Abraham, C. Whittington, J. McAteer, and S. Gupta. 2009. Effective techniques in healthy eating and physical activity interventions: A meta-regression. Health Psychology 28(6):690. https://doi.org/10.1037/a0016136
- Minnesota Departments of Education, Health, Human Services, and Public Safety. n.d. Minnesota student survey: 1992-2013 trends. Available at: http://www.health.state.mn.us/divs/chs/mss/trendreports/msstrendreport2013.pdf
(accessed April 25, 2016). - Minnesota Department of Health and Healthy Minnesota Partnership. 2012. The health of Minnesota: Statewide health assessment. Available at: http://www.health.state.mn.us/statewidehealthassessment/ (accessed April 25, 2016).
- Minnesota Student Survey Interagency Team. 2013a. 2013 Minnesota Student Survey statewide tables. Available at: http://www.health.state.mn.us/divs/chs/mss/statewidetables/ (accessed April 25, 2016)
- Minnesota Student Survey Interagency Team. 2013b. 2013 Minnesota Student Survey county tables (Anoka County). Available at: http://www.health.state.mn.us/divs/chs/mss/countytables/anoka13.pdf (accessed February 18, 2016).
- Ogden, C. L., M. D. Carroll, B. K. Kit, and K. M. Flegal. 2014. Prevalence of childhood and adult obesity in the United States, 2011-2012. JAMA 311(8):806-814. https://doi.org/10.1001/jama.2014.732
- Orimo, H., T. Ueno, H. Yoshida, H. Sone, A. Tanaka, and H. Itakura. 2013. Nutrition education in Japanese medical schools: A follow-up survey. Asia Pacific Journal of Clinical Nutrition 22(1):144. https://doi.org/10.6133/apjcn.2013.22.1.13
- Pacanowski, C. R., K. A. Loth, P. J. Hannan, J. A. Linde, and D. R. Neumark-Sztainer. 2015. Self-weighing throughout adolescence and young adulthood: Implications for well-being. Journal of Nutrition Education and Behavior 47(6):506-515. e501. https://doi.org/10.1016/j.jneb.2015.08.008
- Park, H., and N. Kim. 2008. Predicting factors of physical activity in adolescents: A systematic review. Asian Nursing Research 2(2):113-128. https://doi.org/10.1016/S1976-1317(08)60035-3
- Paul‐Ebhohimhen, V., and A. Avenell. 2008. Systematic review of the use of financial incentives in treatments for obesity and overweight. Obesity Reviews 9(4):355-367. https://doi.org/10.1111/j.1467-789X.2007.00409.x
- Peitz, G. W., J. Troyer, A. E. Jones, N. I. Shapiro, R. D. Nelson, J. Hernandez, and J. A. Kline. 2014. Association of body mass index with increased cost of care and length of stay for emergency department patients with chest pain and dyspnea. Circulation: Cardiovascular Quality and Outcomes 7(2):292-298. https://doi.org/10.1161/CIRCOUTCOMES.113.000702
- Petruzzello, S. J., D. M. Landers, B. D. Hatfield, K. A. Kubitz, and W. Salazar. 1991. A meta-analysis on the anxiety-reducing effects of acute and chronic exercise. Sports Medicine 11(3):143-182. https://doi.org/10.2165/00007256-199111030-00002
- Pew Research Center. 2014. Cell phone and smartphone ownership demographics. Available at: http://www.pewinternet.org/data-trend/mobile/cell-phone-and-smartphone-ownershipdemographics/ (accessed February 4, 2016).
- Polak, R., R. M. Pojednic, and E. M. Phillips. 2015. Lifestyle medicine education. American Journal of Lifestyle Medicine 9(5):361-367. https://doi.org/10.1177/1559827615580307
- Pronk, N. P. 2003. Designing and evaluating health promotion programs. Disease Management & Health Outcomes 11(3):149-157. Available at: https://insights.ovid.com/disease-management-health-outcomes/dmaho/2003/11/030/designing-evaluating-health-promotion-programs/2/00115677 (accessed July 20, 2020).
- Pronk, N. P., T. E. Kottke, and G. J. Isham. 2013. Leveraging lifestyle medicine and social policy to extend the Triple Aim from the clinic into the community. American Journal of Lifestyle Medicine 7(6):360-366. Available at: https://www.healthpartners.com/knowledgeexchange/display/document-rn18228 (accessed July 20, 2020).
- Puhl, R., J. Peterson, and J. Luedicke. 2012. Fighting obesity or obese persons? Public perceptions of obesity-related health messages. International Journal of Obesity 1:9. https://doi.org/10.1038/ijo.2012.156
- Purnell, J. Q., R. Gernes, R. Stein, M. S. Sherraden, and A. Knoblock-Hahn. 2014. A systematic review of financial incentives for dietary behavior change. Journal of the Academy of Nutrition and Dietetics 114(7):1023-1035. https://doi.org/10.1016/j.jand.2014.03.011
- Raths, D. 2015. Kaiser survey links portal use with improved perceptions of health. Healthcare Informatics. Available at: http://www.healthcare-informatics.com/article/kaiser-survey-links-portal-useimproved-perceptions-health (accessed April 26, 2016).
- Reeves, M. J., and R. P. Bailey. 2014. The effects of physical activity on children diagnosed with attention deficit hyperactivity disorder: A review. Education 3-13:1-13. https://doi.org/10.1080/03004279.2014.918160
- Reicks, M., J. Banna, M. Cluskey, C. Gunther, N. Hongu, R. Richards, G. Topham, and S. S. Wong. 2015. Influence of parenting practices on eating behaviors of early adolescents during independent eating occasions: Implications for obesity prevention. Nutrients 7(10):8783-8801. https://doi.org/10.3390/nu7105431
- Roberts, R. E., and H. T. Duong. 2015. Does major depression affect risk for adolescent obesity? Journal of Affective Disorders 186:162-167. https://doi.org/10.1016/j.jad.2015.06.030
- Rosen, J. C., J. Gross, and L. Vara. 1987. Psychological adjustment of adolescents attempting to lose or gain weight. Journal of Consulting and Clinical Psychology 55(5):742. https://doi.org/10.1037/0022-006X.55.5.742
- Ryan, R. M. and E. L. Deci. 2000. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. American Psychologist 55(1):68-78. Available at: https://selfdeterminationtheory.org/SDT/documents/2000_RyanDeci_SDT.pdf (accessed July 20, 2020).
- Seburg, E. M., B. A. Olson-Bullis, D. M. Bredeson, M. G. Hayes, and N. E. Sherwood. 2015. A review of primary care-based childhood obesity prevention and treatment interventions. Current Obesity Reports 4(2):157-173. https://doi.org/10.1007/s13679-015-0160-0
- Secretary’s Advisory Committee on Health Promotion and Disease Prevention Objectives for 2020. 2010. Healthy people 2020: An opportunity to address societal determinants of health in the United States.
Available at: http://www.healthypeople.gov/2010/hp2020/advisory/SocietalDeterminantsHealth.htm (accessed April 25, 2016) - Shanker, D. 2015. The future of medicine is food. Quartz. Available at: http://qz.com/545110/the-future-of-medicine-is-food/ (accessed April 25, 2016).
- Sherwood, N. E., R. L. Levy, S. L. Langer, M. M. Senso, A. L. Crain, M. G. Hayes, J. D. Anderson, E. M. Seburg, and R. W. Jeffery. 2013. Healthy homes/healthy kids: A randomized trial of a pediatric primary care-based obesity prevention intervention for at-risk 5–10 year olds. Contemporary Clinical Trials 36(1):228-243. https://doi.org/10.1016/j.cct.2013.06.017
- Sherwood, N. E., M. M. JaKa, A. L. Crain, B. C. Martinson, M. G. Hayes, and J. D. Anderson. 2015. Pediatric primary care–based obesity prevention for parents of preschool children: A pilot study. Childhood Obesity 11(6):674-682. https://doi.org/10.1089/chi.2015.0009
- Showell, N. N., O. Fawole, J. Segal, R. F. Wilson, L. J. Cheskin, S. N. Bleich, Y. Wu, B. Lau, and Y. Wang. 2013. A systematic review of home-based childhood obesity prevention studies. Pediatrics 132(1):e193-e200. https://doi.org/10.1542/peds.2013-0786
- Sleddens, S. F., S. M. Gerards, C. Thijs, N. K. De Vries, and S. P. Kremers. 2011. General parenting, childhood overweight and obesity-inducing behaviors: A review. International Journal of Pediatric Obesity 6(Supp 3):e12-e27. https://doi.org/10.3109/17477166.2011.566339
- Slomski, A. 2014. Overweight preschoolers headed for cardiometabolic problems. JAMA 312(12):1184. https://doi.org/10.1001/jama.2014.12511
- Smith, A. W., L. A. Borowski, B. Liu, D. A. Galuska, C. Signore, C. Klabunde, T. T.-K. Huang, S. M. Krebs-Smith, E. Frank, and N. Pronk. 2011. US primary care physicians’ diet, physical activity, and weight-related care of adult patients. American Journal of Preventive Medicine 41(1):33-42. https://doi.org/10.1016/j.amepre.2011.03.017
- Stavrakakis, N., P. de Jonge, J. Ormel, and A. J. Oldehinkel. 2012. Bidirectional prospective associations between physical activity and depressive symptoms. The TRAILS study. Journal of Adolescent Health 50(5):503-508. https://doi.org/10.1016/j.jadohealth.2011.09.004
- Strecher, V. J., B. M. DeVellis, M. H. Becker, and I. M. Rosenstock. 1986. The role of self-efficacy in achieving health behavior change. Health Education & Behavior 13(1):73-92. https://doi.org/10.1177/109019818601300108
- Sung‐Chan, P., Y. Sung, X. Zhao, and R. Brownson. 2013. Family‐based models for childhood‐ obesity intervention: A systematic review of randomized controlled trials. Obesity Reviews 14(4):265-278. https://doi.org/10.1111/obr.12000
- Taber, D. R., J. F. Chriqui, F. M. Perna, L. M. Powell, and F. J. Chaloupka. 2012. Weight status among adolescents in states that govern competitive food nutrition content. Pediatrics 130(3):437-444. https://doi.org/10.1542/peds.2011-3353
- Teixeira, P. J., E. V. Carraca, M. M. Marques, H. Rutter, J. M. Oppert, I. De Bourdeaudhuij, J. Lakerveld, and J. Brug. 2015. Successful behavior change in obesity interventions in adults: A systematic review of self-regulation mediators. BMC Medicine 13:84. https://doi.org/10.1186/s12916-015-0323-6
- Trust for America’s Health. 2015. State of obesity. Available at: http://stateofobesity.org/files/stateofobesity2015.pdf (accessed April 25, 2016).
- Turner, L., and F. Chaloupka. 2015. Improvements in school lunches result in healthier options for millions of U.S. Children: Results from public elementary schools between 2006-7 and 2013-14. Chicago, IL: Bridging the Gap Program, Health Policy Center, Institute for Health Research and Policy, University of Illinois at Chicago.
- Tversky, A., and D. Kahneman. 1991. Loss aversion in riskless choice: A reference-dependent model. Quarterly Journal of Economics 106(4):1039-1061. https://doi.org/10.2307/2937956
- U.S. Preventative Services Task Force. 2010. Screening for obesity in children and adolescents: U.S. Preventative Services Task Force recommendation statement. Pediatrics 125(2):361-367. Available at: https://www.uspreventiveservicestaskforce.org/uspstf/document/RecommendationStatementFinal/obesity-in-children-and-adolescents-screening (accessed July 20, 2020).
- Viner, R. M., E. M. Ozer, S. Denny, M. Marmot, M. Resnick, A. Fatusi, and C. Currie. 2012. Adolescence and the social determinants of health. Lancet 379(9826):1641-1652. https://doi.org/10.1016/S0140-6736(12)60149-4
- Von Kries, R., A. M. Toschke, B. Koletzko, and W. Slikker. 2002. Maternal smoking during pregnancy and childhood obesity. American Journal of Epidemiology 156(10):954-961. https://doi.org/10.1093/aje/kwf128
- Wang, Y., Y. Wu, R. F. Wilson, S. Bleich, L. Cheskin, C. Weston, N. Showell, O. Fawole, B. Lau, and J. Segal. 2013. Childhood obesity prevention programs: Comparative effectiveness review and meta-analysis. AHRQ Publication No. 13-EHC081-EF. Rockville, MD: Agency for Healthcare Research and Quality. Available at: http://www.ncbi.nlm.nih.gov/books/NBK148737/ (accessed April 26, 2016).
- Wen, L. M., L. A. Baur, C. Rissel, K. Wardle, G. Alperstein, and J. M. Simpson. 2007. Early intervention of multiple home visits to prevent childhood obesity in a disadvantaged population: A home-based randomised controlled trial (Healthy Beginnings trial). BMC Public Health 7(1):1. https://doi.org/10.1186/1471-2458-7-76
- Wen, L. M., L. A. Baur, J. M. Simpson, C. Rissel, K. Wardle, and V. M. Flood. 2012. Effectiveness of home-based early intervention on children’s BMI at age 2: Randomised controlled trial. BMJ 344:e3732.https://doi.org/10.1136/bmj.e3732
- Yu, Z., S. Han, J. Zhu, X. Sun, C. Ji, and X. Guo. 2013. Pre-pregnancy body mass index in relation to infant birth weight and offspring overweight/obesity: A systematic review and meta-analysis. PloS One 8(4):e61627. https://doi.org/10.1371/journal.pone.0061627
- Yun, L., R. E. Boles, M. A. Haemer, S. Knierim, L. M. Dickinson, H. Mancinas, S. J. Hambidge, and A. J. Davidson. 2015. A randomized, home-based, childhood obesity intervention delivered by patient navigators. BMC Public Health 15(1):1. https://doi.org/10.1186/s12889-015-1833-z