Technology-Enabled Transitions of Care in a Collaborative Effort between Clinical Medicine and Public Health: A Population Health Case Report
Background
Patients of low socioeconomic status (SES) are at higher risk than patients of greater means for hospitalization for conditions that can be addressed in the ambulatory setting (Kangovi et al., 2013; 2014). Patients of low SES are twice as likely as those of higher SES to require urgent emergency department (ED) visits, four times more likely to require hospital admission, and more likely to be readmitted post-discharge (Kangovi et al., 2013; 2014; Disano et al., 2010; Shipton, 1996). Furthermore, patients of low SES have been shown to use 45 percent less ambulatory and preventive care than their more affluent counterparts (Kangovi et al., 2013; 2014). This underuse of primary care and overuse of hospital-based or emergency care is costly to the health care system, results in relatively poorer health outcomes for persons with low SES, and exacerbates health disparities (Kangovi et al., 2013; 2014; Gardner et al., 2014).
A related fact is that poorly executed care transitions (care transitions or transitions of care are terms used to describe when a patient moves from the care of one provider to another, such as when leaving the hospital and returning to the community) from the hospital to the community are associated with higher costs, increased avoidable hospitalization, re-hospitalization, and poorer health outcomes (Kangovi et al., 2013; 2014; Gardner et al., 2014; Marcotte et al., 2014). Deficient transitions resulting in the loss of critical clinical patient information increase the risk of medical errors, posing a threat to patient safety (Marcotte et al., 2014; Campion et al., 2013). More importantly, inefficient transitions may fuel patient difficulties in taking care of themselves and may underlie poor post-hospital outcomes among patients of low SES (Kangovi et al., 2013; 2014).
By taking action to reduce avoidable hospitalizations and ED visits among this at-risk population, health systems could take advantage of a substantial opportunity to improve quality and control costs (Kangovi et al., 2013; 2014). Transitions from one entity in a care system to another have significant potential to fulfill this need and may improve health care quality, reduce costs, and promote more equitable care for vulnerable populations. Collaborative, community-based efforts to improve transitions of care have been shown to be highly effective in meeting patient needs and improving population health (Bauer et al., 2014; Bolch et al., 2005; Gardner et al., 2014; Gentles et al., 2010; Santana et al., 2014). Multi-professional care coordination teams and health information technologies supporting transitions of care have been shown to reduce avoidable hospital admissions and readmissions, improve quality and health outcomes, reduce lengths of stay, improve the continuity of care, and reduce geographic barriers in order to ensure equitable delivery (Allen et al., 2013; Bauer et al., 2014; Brock et al., 2013; Campion et al., 2013; Disano et al., 2010; Gray et al., 2012; Markley et al., 2012; Samal et al., 2013; Santana et al., 2014).
The timely communication of patient information during transitions of care aids in critical follow-up processes relating to patient care plans (Markley et al., 2012). Transition-of-care discharge-planning systems—supported by health information technology and utilized by hospital staff and community health service providers—have been shown to improve communication, workflow, and care-transition processes (Bolch et al., 2013). In addition, evidence suggests that automated transition-of-care alert systems help avoid potential workflow errors and human errors involved in data transmission (Campion et al., 2013). Community-wide collaborative efforts can effectively reduce admissions and readmissions to hospitals (Markley et al., 2012).
Description of Initiative: Transitions of Care
Clinical medicine and public health have historically operated somewhat independently, despite having the common goals of supporting the health of individuals and communities. Emerging opportunities for drawing the health care and public health sectors into collaborative efforts aimed at improving population health have revived enthusiasm for integrating clinical medicine and public health (IOM, 2012). Developing strong partnerships between clinical medicine and public health can help improve transitions from clinical to community settings and has tremendous potential to improve health outcomes, reduce health disparities, and advance population health. As the United States undergoes health reform, such partnerships offer the opportunity to reinvent the health care system through emphasizing preventive care and population health (Fried and Thibault, 2015).
The South East Minnesota Beacon (SEMN Beacon) program, funded by the Office of the National Coordinator of Health Information Technology from 2010 to 2013, supported the development of health information technology infrastructure intended to support collaboration among clinical and community partners (Marchant et al., 2013). This paper describes Transitions of Care, one of several projects initiated under Beacon funding as an example of a successful partnership between clinical medicine and public health. During the SEMN Beacon initiative, Transitions of Care was developed as a pilot project between Mayo Clinic Hospitals and Olmsted County Public Health Services to support care transitions from hospital to other care settings (e.g. home) in a timely manner. Prior to the implementation of this electronic alert system, it had taken several weeks to months for public health personnel to find out if one of their clients had been seen in the ED or been hospitalized. Further details on the informatics infrastructure underlying the Transitions of Care initiative have been documented elsewhere (Marchant et al., 2013).
The initial aim of the Transitions of Care project was to improve the quality of care and to reduce hospital readmissions for public health clients through a health information technology-enabled transition-of-care solution (Marchant et al, 2013). The project required the development of a scalable health information technology architecture with data exchange capabilities across clinical and public health entities. The pilot between Mayo Clinic Rochester and Olmsted County Public Health Services went live in June 2013. The development of real-time connectivity among the Mayo Clinic registration system (Healthquest), the Mayo Clinic G.E. Electronic Medical Record (EMR), and Olmsted County Public Health Services PH-Doc EMR system enabled the following functions: (1) timely alerts to public health case managers each time one of their clients visited the ED, was kept under observation, or was admitted or discharged from the hospital; (2) the management of client consent to share data across entities in real time for public health and inpatient care locations; and (3) timely communications among case managers, inpatient clinicians, and clients to determine care plans, support clinical decisions, utilize community resources, inform follow-up, and reduce the number of readmissions in order to better meet the patient’s health care needs (Marchant et al., 2013. Importantly, this technology infrastructure can be scaled up, can be used with multiple vendors, and adheres to HIPAA and other privacy and security regulations and protocols for exchanging protected health information.
Results
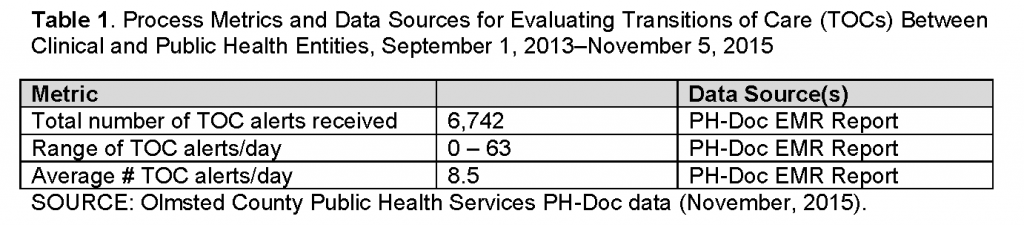
Following an intensive design and development process, the Transitions of Care pilot program successfully demonstrated the capacity to send alerts between clinical and public health settings within minutes of ED visits, hospital admissions, and discharges. Clients served by Olmsted County Public Health Services represent a traditionally disadvantaged group, with 90 percent of them receiving Medicaid coverage for health services. From the initial roll-out of the Transitions of Care initiative in 2013 until mid-year 2015, more than 6,500 alerts were generated, with the number of daily alerts ranging from 1 to 63. Over the same period, more than 1,000 unique public health clients in Olmsted County benefitted from the Transitions of Care tool. Key process metrics are summarized in Table 1. More recently, the Transitions of Care architecture has been expanded to include public health departments in 11 neighboring counties.
The Transitions of Care alerts contain simple, useful information, including client name, clinical contact information (e.g., ED visit, hospital admission, or hospital discharge), source of alert (e.g., ED or specific hospital), and the date and time of clinical contact. Alerts generated by Mayo Clinic hospitals are delivered to one of the Olmsted County Public Health Services PHDoc sites and are configured to be delivered to the user as either an email or a text alert (or both), with the detailed information being accessible inside the PH-Doc application. When PHDoc receives an alert, the system reviews the client settings to determine and verify all associated PH-Doc users. The associated users then receive a pop-up message on their screens, and an alert is added to the upper right corner of each user’s PH-Doc screen with the associated message included in the drop down menu. This process ensures that all relevant public health personnel are alerted. The alert contains just enough information to let public health nurses or social workers know if one of their clients has had a significant clinical contact and when and where the contact occurred, thus prompting them to then take appropriate action. With this accurate and concise information, public health nurses and social workers are able to respond quickly to support their clients. Responses vary according to such factors as the health status of the client, the public health services currently received by the client, and the extent to which other community providers are involved.
Public health nurses and social workers use Transitions of Care alerts in their work with older adults and clients who are disabled, helping them coordinate appropriate services in a timely fashion. Nurses and social workers respond to hospital-admission Transitions of Care alerts for their clients with phone calls to the client or family or to the nursing station to better understand the client’s health status and discern client needs in order to support transition on discharge. They also request medical records electronically in order to learn about the admitting diagnoses, medication changes, and the plan of care for follow-up appointments from the continuity-of-care documents. With this timely and accurate information, the nurses and social workers are able to tailor their client services, adjusting the amount or type of services needed. Because public health nurses and social workers assess their clients where they live, they have a good understanding of a client’s living environment and types of social supports. Sometimes emergency department visits or hospital admissions do not require a change in services. In such cases, follow-up phone calls become opportunities for the nurses or social workers to further connect with their clients and, in some cases, to learn new information that may be critical to their ongoing care.
TOC alerts also inform the practice of maternal and child health (MCH) nurses. These public health nurses follow clients through pregnancy, the post-partum period, and parenting. With Transitions of Care alerts, the nurses are alerted if their clients are admitted for preterm labor, when their clients deliver their babies, and if their clients experience post-partum complications. Having early knowledge of these events allows nurses to offer support and services to help patients follow through with the prescribed bed rest to prevent preterm delivery, to offer newborn support services, or to assist clients with post-partum needs, as appropriate. The Transitions of Care tool also helps ensure continued support for new parents through alerts to indicate if special-needs children experience exacerbations of their conditions. The Transitions of Care tool allows MCH nurses to maintain a greater awareness of critical events in their clients’ health. For example, one nurse was preparing for a visit to a newly pregnant client when she received an alert that the client had been in the emergency department. The nurse requested electronic documents and learned that the client had experienced a miscarriage. This provided the nurse with the information she needed to appropriately adjust her visit plan, understanding in advance that she would be addressing this client’s loss rather than a new pregnancy. The MCH nurses have come to rely on Transitions of Care alerts to know when their clients have delivered their babies, allowing them to schedule new baby visits closer to their hospital discharge, thus giving more timely support during a critical time.
The health information exchange technology underlying the Transitions of Care alert tool makes possible early intervention, more robust communication, and greater continuity of care. Nurses and social workers from across the partnering public health agencies have used the Transitions of Care alerts to address emerging issues for their clients and to support adherence to follow-up care. Public health nurses and social workers have integrated Transitions of Care alerts into their practice, relying upon them as a cue to contact clients and their families and be more responsive to their clients’ needs.
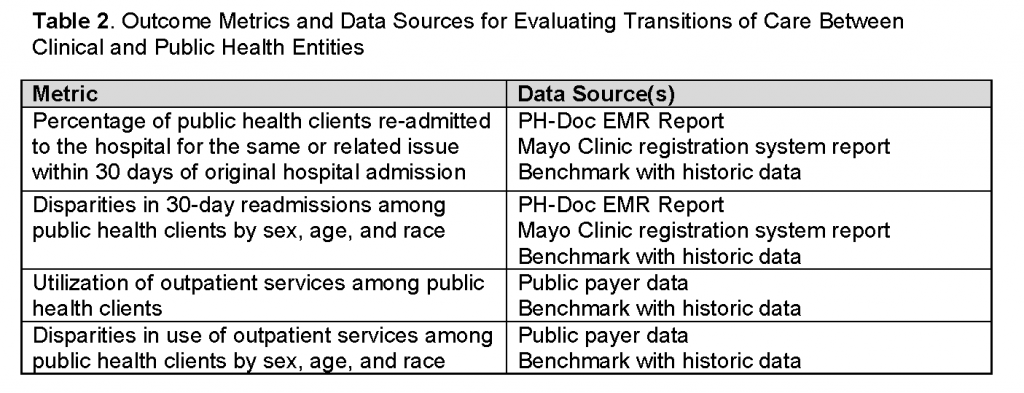
Work is currently underway to track process and outcome measures in order to evaluate the impact of the Transitions of Care tool. Key process measures include the number of alerts dispatched, the type of alert dispatched (ED visit, hospital admission, hospital discharge), the number of unique individuals initiating alerts, the number of false alerts, and the number of failed alerts. Key impact and outcome measures of interest include subsequent health care utilization, hospital readmissions, and the analysis of alerts and outcomes by key demographic variables including sex, age, and race. The primary metrics for the impact and outcome measures are summarized in Table 2.
Discussion
The Transitions of Care tool aims to support care transitions for highly vulnerable populations, including low-income, uninsured, and underinsured groups. The current use of the Transitions of Care tool, described in this case report, supports the feasibility of health information technology-enabled systems for improving communication and data exchange between public health and clinical entities in order to enable greater continuity of care for traditionally underserved populations. Ongoing use of the Transitions of Care tool beyond the initial funding period for its development and a recent expansion of the tool to neighboring counties speak to the tool’s sustainability and scalability. Furthermore, the development of shared infrastructure resonates with one of the principles for successful integration of public health and clinical medicine laid out by the Institute of Medicine Committee on Integrating Primary Care and Public Health, which describes “the establishment of a shared infrastructure and building for enduring value and impact” as key to sustainability (IOM, 2012, p. 6).
This collaborative effort between clinical and public health entities aligns with present-day health reform efforts that call for projects aimed at closing the gap between clinical care for the patient and the health of the population (Marcotte et al, 2014). Emerging capabilities in health information technology may serve as fertile ground for future collaborative efforts between clinical medicine and public health, provide for sustainable and scalable infrastructures to support ongoing integration, and support collaborative efforts to improve individual and population health, reduce costs, and improve the care experience.
References
- Allen, J., G. Ottmann, and G. Roberts. 2013. Multi-professional communication for older people in transitional care: A review of the literature. International Journal of Older People Nursing 8(4):253–269. https://doi.org/10.1111/j.1748-3743.2012.00314.x
- Bauer, A. M., S. M. Thielke, W. Katon, J. Unützer, and P. Areán. 2014. Aligning health information technologies with effective service delivery models to improve chronic disease care. Preventive Medicine 66:167–172. https://doi.org/10.1016/j.ypmed.2014.06.017
- Bolch, D., J. B. Johnston, L. C. Giles, C. Whitehead, P. Phillips, and M. Crotty. 2005. Hospital to home: An integrated approach to discharge planning in a rural South Australian town. The Australian Journal of Rural Health 13(2):91–96. https://doi.org/10.1111/j.1440-1854.2005.00660.x
- Brock, J., J. Mitchell, K. Irby, B. Stevens, T. Archibald, A. Goroski, and J. Lynn, for the Care Transitions Project Team. 2013. Association between quality improvement for care transitions in communities and rehospitalizations among Medicare beneficiaries. JAMA 309(4):381–391. https://doi.org/10.1001/jama.2012.216607
- Campion, T. R., Jr., J. R. Vest, J. S. Ancker, R. Kaushal, and the HITEC Investigators. 2013. Patient encounters and care transitions in one community supported by automated query-based health information exchange. AMIA Annual Symposium Proceedings 2013:175–184. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3900171/ (accessed July 17, 2020).
- Disano, J., J. Goulet, N. Muhajarine, C. Neudorf, and J. Harvey. 2010. Social-economic status and rates of hospital admission for chronic disease in urban Canada. The Canadian Nurse 106(1):24–29. Available at: https://europepmc.org/article/med/20175317 (accessed July 17, 2020).
- Fried, L. P. and G. E. Thibault. 2015. Reinventing public health education for the 21st century. American Journal of Public Health 105(Suppl 1):S4. https://doi.org/10.2105/AJPH.2014.302544
- Gardner, R., Q. Li, R. R. Baier, K., Butterfield, E. A. Coleman, and S. Gravenstein. 2014. Is implementation of the care transitions intervention associated with cost avoidance after hospital discharge? Journal of General Internal Medicine 29(6):878–884. https://doi.org/10.1007/s11606-014-2814-0
- Gentles, S. J., C. Lokker, and K. A. McKibbon. 2010. Health information technology to facilitate communication involving health care providers, caregivers, and pediatric patients: A scoping review. Journal of Medical Internet Research 12(2):e22. https://doi.org/10.2196/jmir.1390
- Gray, L. C., N. M. Peel, M. Crotty, S. E. Kurrle, L. C. Giles, and I. D. Cameron. 2012. How effective are programs at managing transition from hospital to home? A case study of the Australian Transition Care Program. BMC Geriatrics 12:6. https://doi.org/10.1186/1471-2318-12-6
- Institute of Medicine. 2012. Primary Care and Public Health: Exploring Integration to Improve Population Health. Washington, DC: The National Academies Press. https://doi.org/10.17226/13381
- Kangovi, S., F. K. Barg, T. Carter, J. A. Long, R. Shannon, and D. Grande. 2013. Understanding why patients of low socioeconomic status prefer hospitals over ambulatory care. Health Affairs 32(7):1196–1203. https://doi.org/10.1377/hlthaff.2012.0825
- Kangovi, S., F. K. Barg, T. Carter, K. Levy, J. Sellman, J. A. Long, and D. Grande. 2014. Challenges faced by patients with low socioeconomic status during the post-hospital transition. Journal of General Internal Medicine 29(2):283–289. https://doi.org/10.1007/s11606-013-2571-5
- Marcotte, L., J. Kirtane, J. Lynn, and A. McKethan. 2014. Integrating health information technology to achieve seamless care transitions. Journal of Patient Safety 11(4):185–190. https://doi.org/10.1097/PTS.0000000000000077
- Marchant, K., D. Jensen, D. Costellanos, D. Eid, and A. Alexander. 2013. Public health based transitions of care: ADT alerts to reduce readmissions in public health patients. Southeast Minnesota Beacon Program, Rochester, MN. Unpublished White Paper.
- Markley, J., K. Sabharwal, Z. Wang, C. Bigbee, and L. Whitmire. 2012. A community-wide quality improvement project on patient care transitions reduces 30-day hospital readmissions from home health agencies. Home Health Care Nurse 30(3):E1–E11. https://doi.org/10.1097/NHH.0b013e318246d540
- Samal, L., P. C. Dykes, J. Greenberg, O. Hasan, A. K. Venkatesh, L. A. Volk, and D. W. Bates. 2013. The current capabilities of health information technology to support care transitions. AMIA Annual Symposium Proceedings 2013:1231. Available at: https://europepmc.org/article/med/24551404 (accessed July 17, 2020).
- Santana, M. J., J. Holroyd-Leduc, W. W. Flemons, M. O’Beirne, D. White, N. Clayden, A. J. Forster, and W. A. Ghali. 2014. The seamless transfer of care: A pilot study assessing the usability of an electronic transfer of care communication tool. American Journal of Medical Quality 29(6):476–483. https://doi.org/10.1177/1062860613503982
- Shipton, S. 1996. Risk factors associated with multiple hospital readmissions. Home Care Provider 1(2):83–85. https://doi.org/10.1016/s1084-628x(96)90234-8