Social Determinants of Health 101 for Health Care: Five Plus Five
Introduction
Social determinants of health (SDoH) is a relatively new term in health care. As defined by the World Health Organization (WHO), SDoH are “the conditions in which people are born, grow, live, work and age. These circumstances are shaped by the distribution of money, power and resources at global, national and local levels” [1]. The social determinants of health also determine access and quality of medical care—sometimes referred to as medical social determinants of health (see Figure 1 for the County Health Rankings model of factors shaping health). Future opportunities may exist in genetics and biological determinants; however, whether modifying these will be as feasible as modifying the social determinants of health is unknown.
Although the SDoH easily resonate for clinicians, given their intuitive recognition that health outcomes are affected by patients’ conditions outside the clinical walls, clinicians may raise several concerns about involvement in the SDoH. First, they realize that this is not their domain of expertise or current accountability. Second, some are worried that health care systems already have enough to address and should not play a role in efforts to mitigate or improve the SDoH. Third, they express concern about the limited evidence of effectiveness of interventions by health care on the SDoH [2]. There is a viewpoint, however, for health care to find its role in population health [3], and some providers believe there is enough science to support integration of SDoH into health care and are pursuing evidence-informed interventions with community partners [4,5].
Lest we think SDoH are the next panacea in health care, let us consider what we know and what we need to learn about SDoH to achieve the national quality strategy of better care, healthy people/healthy communities, and affordable care [6].
Five Things We Know About (Social) Determinants of Health in Health Care
1. As a determinant of health, medical care is insufficient for ensuring better health outcomes.
Medical care is estimated to account for only 10-20 percent of the modifiable contributors to healthy outcomes for a population [7]. The other 80 to 90 percent are sometimes broadly called the SDoH: health-related behaviors, socioeconomic factors, and environmental factors. Although we as a country spend a higher percentage of our gross domestic product on medical care expenditures than other developed countries, it is more difficult to compare spending on the SDoH. We do know that many developed countries proportionately spend more on social services than the United States [8]. Although social services do not correspond directly to the SDoH, this comparison gives one view of proportional expenditures in our country.
Corollary: Despite our significant spending, our outcomes are among the lowest for developed countries, including significant inequities [9]. For health care, the hope is that addressing the more upstream social determinants will improve health outcomes, reduce inequities, and lower costs. What can we learn from other nations’ medical and nonmedical system efforts that are achieving better health outcomes?
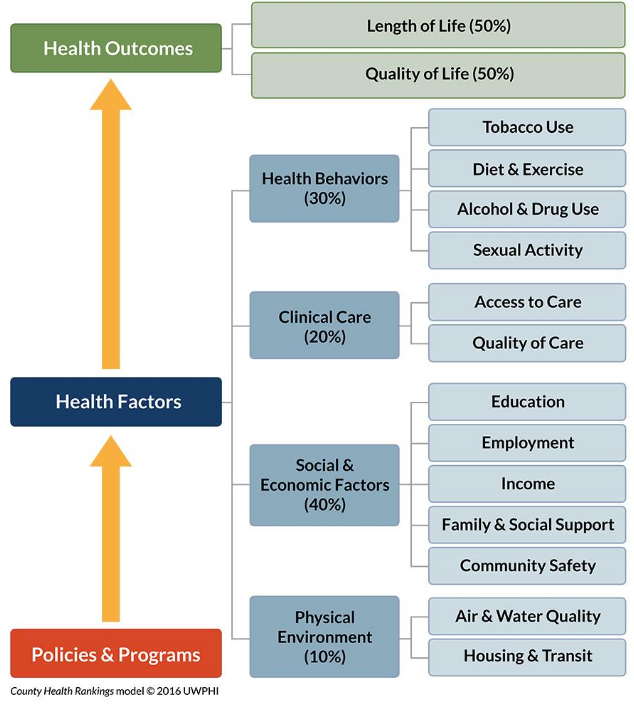
Figure 1 | County Health Rankings & Roadmaps | Source: Reprinted with permission from County Health Rankings & Roadmaps, http://www.countyhealthrankings.org/our-approach (accessed July 18, 2017).
2. SDoH Are Influenced by Policies and Programs, and Associated with Better Health Outcomes.
SDoH are greatly influenced by policies, systems, and environments (PSE). A diagram used by County Based Health Rankings and Roadmaps (Figure 1) shows the interaction between health outcomes, the SDoH, and policies and programs. For example, tobacco is a leading determinant of many health outcomes (e.g., mortality, quality of life), and decreasing tobacco use is more influenced by the price of cigarettes and smoke-free environments in the community than by the availability of cessation clinics or quitlines.
Corollary: Community partnerships that synergize medical interventions and PSE changes produce a more comprehensive approach to behavior change. For example, walking prescriptions for patients can be complemented by community changes to increase availability of safe walking spaces. Such partnerships can also allay providers’ concerns about being held responsible for problems outside their clinical domain, and the partnerships can bring expertise, allies, and resources to address complex issues such as tobacco use, physical activity, alcohol use, housing, and so on.
3. New Payment Models Are Prompting Interest in the SDoH.
New value-based payment models such as alternative payment models, accountable care models such as accountable care organizations (ACOs) and patient-centered medical homes, and Medicare Shared Savings are moving toward payment for outcomes rather than process measures, as well as benchmarks for “total cost of care.” Since better results on the SDoH are associated with better health outcomes, will payment models evolve to jointly reward health care organizations and communities for outcomes such as lower tobacco, obesity and/or diabetes prevalence, or improved high school graduation rates?
Corollary: The Population-based Payment Model Workgroup of the Health Care Learning and Action Network (LAN) recently recommended that “Big(ger) Dot” measures increasingly be used in new payment models. For example, measures of cardiac care are ideally outcome measures (e.g., 30-day mortality, health-related quality of life or well-being), not individual process measures (e.g., aspirin at arrival (https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/HospitalQualityInits/downloads/HospitalOverviewOfSpecs200512.pdf)) [10]. However, process measures continue to be important for quality improvement and for some payment programs. New summary measures for population health and well-being for use by health plans and accountable care organizations have been proposed [11,12], and frameworks for rewarding health outcomes are being developed.
4. Frameworks for Integrating SDoH Are Emerging.
Data frameworks have been proposed for integrating SDoH into primary care and capturing SDoH domains in electronic health records (EHRs). One framework includes community-driven and individual data for use in primary care, recognizing that there are still questions about the effect on outcomes [13]. The framework, however, does not include how the data might be used with community partnerships to expand the effect of collecting the data.
Screening tools have been developed, e.g., for an accountable health community initiative [14], and one for a pediatric emergency department with a low-income population [15]. Models are emerging for how to follow up screening data, e.g., “clinic-to-community treatment models” for children living in food-insecure households [16].
For the EHR, the Institute of Medicine (IOM) has recommended that social and behavioral health domains be captured [17]. The incentive, training, and privacy barriers for feasibility of incorporating SDoH into EHRs have been discussed [18]. Interestingly, electronic screening produced higher rates of self-disclosure of some sensitive determinants (violence and substance abuse) than in-person screening [15]. Most recently, the feasibility, reliability, and validity of the IOM-recommended domains (except for income) were evaluated, and clinical trials were recommended [19, 20].
Corollary: Integrating the SDoH into health care should not fall primarily on primary care clinicians. Although front-line clinicians can see patterns of key determinants for populations, leadership within health care organizations must advance this work by alignment with strategic directions, board support for community partnerships, adopting a culture that values the SDoH in addition to quality and affordable health care, measurement/evaluation, role clarification, creation of new skill sets, and realignment of resources [21], i.e., building a system approach to integration. These leadership actions allow front-line clinicians to be natural champions for the SDoH within the organization and the community without being responsible for all the necessary components of a systems approach.
5. Experiments Are Occurring at the Local and Federal Level.
State innovation models are exploring connections among health care, social services, and some SDoH [22]. ACOs are responding to nonmedical needs of patients such as transportation, housing, and food with the assumption that outcomes and cost will improve [4]. One randomized pediatric intervention of in-person navigation services in two safety-net hospitals to address families’ social needs demonstrated a decrease in the families’ report of social needs and better reported children’s overall health status [23], and the authors recommend more experiments to determine investments in interventions. The Centers for Medicare & Medicaid Services (CMS) launched accountable health communities (ACH)—the first innovation-center model to test matching the needs of a population (i.e., CMS beneficiaries) with community resources [24,25]. With a robust evaluation plan, the five-year ACH model tests two tracks: assistance track – provide community service navigation assistance, and alignment track – encourage partner alignment to ensure services are available and responsive. These experiments will provide more evidence about effectiveness in achieving better outcomes, better experience, and lower costs.
Five Things We Need to Learn about Social Determinants of Health in Health Care
1. How do we prioritize SDoH for individual patients and for communities?
Prioritization requires an assessment of readiness to address proven or testable interventions, and return on investment. Which patients will benefit the most from addressing their SDoH, and which SDoH? Which patients are most ready for these interventions? Which interventions will decrease per capita spending? From a community perspective, which SDoH are of most concern to community stakeholders, and which SDoH will have the greatest effect on total population health and well-being, health equity, and health care expenditures?
2. How do we intervene without medicalizing SDoH?
There is a danger that a medical approach to these nonmedical factors will lead to more health care versus more cost-effective and community-based interventions. For example, a social worker sees a patient with schizophrenia once a week in northern Minnesota, but she says, “What this patient needs is a friend.” How do we avoid “re-creating the wheel” inside health care and increasing costs? How do we listen to communities, identify and delineate health care’s role, and collaborate appropriately with existing community resources and increase capacity? As health care professionals, we need huge doses of humility and openness to authentically address SDoH and form or join community partnerships. A recent infographic illustrates an emerging path for community collaboration—from the “aha moments” to feedback and course correction to new dialogue with the community [34].
Corollary: We often speak of the SDoH, but what are the “social determinants of well-being”? Well-being is “the sense of life satisfaction of the individual” as introduced by Evans and Stoddart in their classic paper on the determinants of health, in which they postulate that well-being is the ultimate objective of health policy [35]. Advancing “social determinants of well-being” versus health does not have the automatic association with hospitals, clinics, visits, tests, procedures, and medication that the term health has. This concept is promoted by Kottke, Stiefel, and Pronk who suggest we engage others and avoid medicalizing by focusing on “well-being in all policies” rather than health in all policies [36,37].
3. What (new) data are needed?
A third question is what SDoH data should be collected—for what purpose, and by whom? Recently, HealthDoers, a Robert Wood Johnson Foundation–funded network with the Network for Regional Healthcare Improvement, held a Peer-to-Peer (P2P) event focused on the intersection of clinical, multisector, and SDoH data. Nial Brennan, former Chief Data Officer at CMS, asked how SDoH data fared on four key questions he says he always asks about collecting new data [27]:
- “How much will it cost to collect? Is the juice worth the squeeze?
- “How good [are] the data? Is it standardized?
- “How comprehensive [are] the data? Are we getting it for 5%, 10%, 50%, 100%of people?
- “What level of granularity does the data need to be at?”
These questions lead us back to issues of prioritization, the opportunity index, and effective interventions.
With so many unknowns about the use of SDoH in clinical care, having data for measurement and evaluation of interventions is essential. Monitoring for unintended consequences of well-designed and/or well-intentioned programs and policies is important, especially to ensure that disparities do not worsen.
4. How do we build multisector partnerships?
What partnerships should be built to address the SDoH for individuals and for communities? What sectors need to be involved to achieve the desired outcomes? What are the roles of people and organizations in these different partnerships? Building these multisector partnerships requires trust for not only sharing data but also for sharing resources and money. What factors are most important for building trust between health care organizations and community partners, where there is often a power differential? A recent workshop from the National Academies of Sciences, Engineering, and Medicine (NASEM) explores the infrastructure of successful multisector partnerships, including examples of health sector and community collaboration [38]. For example, a leader from Bellin Health identified five “domains of transformation”: (1) understand the system, (2) social change, (3) critical conversations, (4) co-creation, and (5) spread and scale.
Corollary: What level of integration (e.g., in continuity of care, responsibility for quality and costs for a population, hospital affiliation, etc.) between health care organizations and service organizations is needed or not needed to successfully address SDoH with community partners? Does it depend on the SDoH being addressed? Fraze and colleagues [4] describe a typology of ACOs regarding the integration of patients’ non-medical needs with medical care—from noncoordinated to fully integrated—with most ACOs being in the noncoordinated quadrant (“neither services nor organizations were integrated”). More importantly, what specific system components (e.g., global budgets, board leadership, quality improvement culture, data systems, care managers or community health workers, experience with community partnerships) are needed to create effective interventions?
5. What else?
The last question is “What else?” For example, discussions about population health and its measurement often center on the leading causes of death and not well-being or the “leading causes of life,” such as purpose, connection, agency, blessing, and hope [39]. In addition, health care mental models are frequently built from a deficit perspective—addressing what is wrong with an individual and/or a community. How do we focus on assets, starting with what is right with patients, families, and/or communities so we can build on strengths? Building on strengths and working with multisector collaborations are two ways to minimize any unintended consequences of screening for the SDoH in clinical settings [40].
Conclusion
This paper articulates five things we know and five things health care organizations need to learn to address SDoH for the national quality strategy [6]. Critics are right to question how we address yet another issue in health care. However, organizations can define (and circumscribe) their roles [41], and join or form new community partnerships to prioritize, develop, and implement proven and/or testable interventions. With the failure of our current health care system to deliver better health and well-being at an affordable cost, exploring opportunities in the other determinants of health seems wise, if not imperative.
Join the conversation!
![]() Tweet this! 5 things we know & 5 things health care organizations need to learn to address #SDoH: http://bit.ly/2xjnk0s #PopHealthRT
Tweet this! 5 things we know & 5 things health care organizations need to learn to address #SDoH: http://bit.ly/2xjnk0s #PopHealthRT
![]() Tweet this! Exploring opportunities to address #SDoH in health care settings is imperative for pts. What we know: http://bit.ly/2xjnk0s #PopHealthRT
Tweet this! Exploring opportunities to address #SDoH in health care settings is imperative for pts. What we know: http://bit.ly/2xjnk0s #PopHealthRT
![]() Tweet this! Frameworks are emerging for integrating #SDoH into primary care. What we need to learn to make this a reality: http://bit.ly/2xjnk0s
Tweet this! Frameworks are emerging for integrating #SDoH into primary care. What we need to learn to make this a reality: http://bit.ly/2xjnk0s
Download this graphic and share it on social media!
References
- WHO (World Health Organization). 2012. What are the social determinants of health? Available at: http://www.who.int/social_determinants/sdh_definition/en/ (accessed June 8, 2017).
- Solberg, L. I. 2016. Theory vs practice: Should primary care practice take on social determinants of health now? No. Annals of Family Medicine 14:102-103. https://doi.org/10.1370/afm.1918
- Eggleston, E. M., and J. A. Finkelstein. 2014. Finding the role of health care in population health. JAMA 311(8):797-798. https://doi.org/10.1001/jama.2014.163
- Fraze, T., V. A. Lewis, H. P. Rodriquez, and E. S. Fisher. 2016. Housing, transportation, and food: How ACOs seek to improve population health by addressing nonmedical needs of patients. Health Affairs (Millwood) 35(11):2109-2115. https://doi.org/10.1377/hlthaff.2016.0727
- Baciu, A., and J. M. Sharfstein. 2016. Population health case reports from clinic to community. JAMA 315(24):2663-2664. https://doi.org/10.1001/jama.2016.4932
- Agency for Healthcare Research and Quality (AHRQ). 2017. About the National Quality Strategy. Content last reviewed March 2017. Agency for Healthcare Research and Quality, Rockville, MD. Available at: http://www.ahrq.gov/workingforquality/about/index.html (accessed June 11, 2017).
- Hood, C. M., K. P. Gennuso, G. R. Swain, and B. B. Catlin. 2016. County health rankings: Relationships between determinant factors and health outcomes. American Journal of Preventive Medicine 50(2):129-135. https://doi.org/10.1016/j.amepre.2015.08.024
- Bradley, E. H., B. R. Elkins, J. Herrin, and B. Elbel. 2011. Health and social services expenditures: Associations with health outcomes. BMJ Quality and Safety in Health Care 20(10):826-831. https://doi.org/10.1136/bmjqs.2010.048363
- Schneider, E. C., D. O. Sarnak, D. Squires, A. Shah, and M. M. Doty. 2017. Mirror, mirror 2017: International comparison reflects flaws and opportunities for better U.S. health care. The Commonwealth Fund, July 2017. Available at: http://www.commonwealthfund.org/publications/fund-reports/2017/jul/mirror-mirror-international-comparisons-2017 (accessed July 29, 2017).
- Health Care Payment Learning and Action Network (LAN). 2016. Population-based Payment Work Group. Accelerating and aligning population-based payment models: performance measurement. Available at: http://hcp-lan.org/workproducts/pm-whitepaper-final.pdf (accessed June 8, 2017).
- Kottke, T. E., J. M. Gallagher, S. Rauri , J. O. Tillema, N. P. Pronk, and S. M. Knudson. 2016. New summary measures of population health and well-being for implementation by health plans and accountable care organizations. Preventing Chronic Diseases 13:160224. Available at: https://www.cdc.gov/pcd/issues/2016/16_0224.htm (accessed June 11, 2017).
- Kottke, T. E., J. M. Gallagher, S. Rauri, J. O. Tillema, N. P. Pronk and S. M. Knudson. 2016. New Summary Measures of Population Health and Well-being for Implementation by Health Plans and Accountable Care Organizations. NAM Perspectives. Discussion Paper, National Academy of Medicine, Washington, DC. https://doi.org/10.31478/201607b
- DeVoe, J. E., A. W. Bazemore, E. K. Cottrell, S. Likumahuwa-Ackman , J. Grandmont, N. Spach, and R. Gold. 2016. Perspectives in primary care: A conceptual framework and path for integrating social determinants of health into primary care practice. Annals of Family Medicine 14(2):104-108. https://doi.org/10.1370/afm.1903
- Billioux, A., K. Verlander, S. Anthony, and D. Alley. 2017. Standardized Screening for Health-Related Social Needs in Clinical Settings: The Accountable Health Communities Screening Tool. NAM Perspectives. Discussion Paper, National Academy of Medicine, Washington, DC. https://doi.org/10.31478/201705b
- Gottlieb, L., D. Hessler, D. Long , A. Amaya, and N. Adler. 2014. A randomized trial on screening for social determinants of health: The iScreen study. Pediatrics 134(6):e1611-e1618. Available at: www.pediatrics.org/cgi/doi/10.1542/peds.2014-1439.
- Barnidge, E., S. Stenmark, and H. Seligman. 2017. Clinic-to-community models to address food insecurity. Journal of the American Medical Association Pediatrics 171(6):507-508. https://doi.org/10.1001/jamapediatrics.2017.0067
- Institute of Medicine. 2014. Capturing Social and Behavioral Domains and Measures in Electronic Health Records: Phase 2. Washington, DC: The National Academies Press. https://doi.org/10.17226/18951
- Gottlieb, L. M., K. J. Tirozzi, R. Manchanda, A. R. Burns, and M. T. Sandel. 2015. Moving electronic medical records upstream: Incorporating social determinants of health. American Journal of Preventive Medicine 48(2):215-218. https://doi.org/10.1016/j.amepre.2014.07.009
- Giuse, N. B., T. Y. Koonce, S. V. Kusnoor, A. A. Prather, L. M. Gottlieb, L. Huang, S. E. Phillips, Y. Shyr, N. E. Adler, and W. W. Stead. 2017. Institute of Medicine measures of social and behavioral determinants of health: A feasibility study. American Journal of Preventive Medicine 52(2):199-206. https://doi.org/10.1016/j.amepre.2016.07.033
- Prather, A. A., L. M. Gottlieb, N. B. Giuse, T. Y. Koonce, S. V. Kusnoor, W. W. Stead, and N. E. Adler. 2017. National Academy of Medicine social and behavioral measures: Associations with self-reported health. American Journal of Preventive Medicine Mar 21. pii: S0749-3797(17)30157-5. https://doi.org/10.1016/j.amepre.2017.02.010.
- Institute for Clinical Systems Improvement (ICSI). 2015. Going beyond clinical walls: Lessons learned: Leaders stepping out to transform health and health care. Available at: https://www.icsi.org/_asset/pvr9ot/lessonslearned.pdf (accessed June 8, 2017).
- Hester, J. A., J. Auerbach, D. I. Chang, S. Magnan, and J. Monroe. 2015. Opportunity Knocks Again for Population Health: Round Two in State Innovation Models. NAM Perspectives. Discussion Paper, National Academy of Medicine, Washington, DC. https://doi.org/10.31478/201504i
- Gottlieb, L. M., D. Hessler, D. Long, E. Laves, A. R. Burns, A. Amaya, P. Sweeney, C. Schudel, and N. E. Adler. 2016. Effects of social needs screening and in-person service navigation on child health: A randomized clinical trial. Journal of the American Medical Association Pediatrics 170(11):e162521. https://doi.org/10.1001/jamapediatrics.2016.2521
- Alley, D. E., C. N. Asomugha, P. H. Conway, D. M. Sanghavi. 2016. Accountable health communities—addressing social needs through Medicare and Medicaid. New England Journal of Medicine 374(1):8-11. https://doi.org/10.1056/NEJMp1512532
- Centers for Medicare & Medicaid Services (CMS). 2017. Available at: https://innovation.cms.gov/initiatives/ahcm/ (accessed June 8, 2017).
- Lee, V. S., K. Kawamoto, R. Hess, C. Park, J. Young, C. Hunter, S. Johnson, S. Gulbransen, C. E. Pelt, D. J. Horton, K. K. Graves, T. H. Greene, Y. Anzai, and R. C. Pendleton. 2016. Implementation of a value-driven outcomes program to identify high variability in clinical costs and outcomes and association with reduced cost and improved quality. JAMA 316(10):1061-1072. https://doi.org/10.1001/jama.2016.12226
- HealthDoers Network. HealthDoers network peer-to-peer summary: The intersection of clinical data, claims and the social determinants of health: integrating multi-sector data to create health out of health care. 2017. Available at: http://www.nrhi.org/uploads/hdpeer-to-peer-event_jan17_summary_final.pdf; https://vimeo.com/201783081 (accessed June 8, 2017).
- Centers for Disease Control and Prevention (CDC). A practical guide to working with health-care systems on tobacco-use treatment. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health. Available at: https://www.cdc.gov/tobacco/quit_smoking/cessation/pdfs/practical_guide.pdf (accessed June 11, 2017).
- National Collaborative on Childhood Obesity Research (NCCO). 2015. Evaluating community-clinical engagement to address childhood obesity: Implications and recommendations for the field. Available at: http://nccor.org/downloads/NCCOR-Community-Engagement-Workshop-Summary.pdf (accessed June 11, 2017).
- Larimer, M. E., D. K. Malone, M. D. Garner, D. C. Atkins, B. Burlingham, H. S. Lonczak, K. Tanzer, J. Ginzler, S. L. Clifasefi, W. G. Hobson, and G. A. Marlatt. 2009. Health care and public service use and costs before and after provision of housing for chronically homeless persons with severe alcohol problems. JAMA 301(13):1349-1357. https://doi.org/10.1001/jama.2009.414
- Sandberg, S. F., C. Erikson, R. Owen, K. D. Vickery, S. T. Shimotsu, M. Linzer, N. A. Garrett, K. A. Johnsrud, D. M. Soderlund, and J. DeCubellis. 2014. Hennepin Health: A safety-net accountable care organization for the expanded Medicaid population. Health Affairs (Millwood) 33(11):1975–1984. https://doi.org/10.1377/hlthaff.2014.0648
- Taylor, L. A., A. X. Tan, C. E. Coyle, C. Ndumele, E. Rogan, M. Canavan, L. A. Curry, and E. H. Bradley. 2016. Leveraging the social determinants of health: What works? PLoS One 11(8):e0160217. Available at: http://journals.plos.org/plosone/article?id=10.1371/journal.pone.0160217 (accessed June 8, 2017).
- Bickerdike, L., A. Booth, P. M. Wilson, K. Farley, and K. Wright. 2017. Social prescribing: Less rhetoric and more reality. A systematic review of the evidence. BMJ Open 2017;7:e013384. https://doi.org/10.1136/bmjopen-2016-013384
- Institute for Clinical Systems Improvement (ICSI). 2015. Going beyond clinical walls: Pioneering lessons: An emerging health care path for community collaborations. Available at: https://www.icsi.org/_asset/w7vd0v/pathinfographicweb.pdf (accessed June 8, 2017).
- Evans, R. G., and G. L. Stoddart. 1990. Producing health, consuming health care. Social Science & Medicine 31(12):1347-1363. https://doi.org/10.1016/0277-9536(90)90074-3
- Kottke, T. E., M. Stiefel, and N. P. Pronk. 2016. “Well-being in all policies”: Promoting cross-sectoral collaboration to improve people’s lives. Preventing Chronic Diseases 13:160155. Available at: https://www.cdc.gov/pcd/issues/2016/16_0155.htm (accessed June 8, 2017).
- Kottke, T. E., M. Stiefel, and N. P. Pronk. 2016. “Well-Being in All Policies”: Promoting Cross-Sectoral Collaboration to Improve People’s Lives. NAM Perspectives. Discussion Paper, National Academy of Medicine, Washington, DC. https://doi.org/10.31478/201604c
- National Academies of Sciences, Engineering, and Medicine. 2018. Exploring Equity in Multisector Community Health Partnerships: Proceedings of a Workshop. Washington, DC: The National Academies Press. https://doi.org/10.17226/24786
- Gundersen, G., and L. Pray. 2009. Leading causes of life: Five fundamentals to change the way you live your life. Abingdon Press, Nashville, TN.
- Garg, A., R. Boynton-Jarrett, and P. H. Dworkin. 2016. Avoiding the unintended consequences of screening for social determinants of health. JAMA 316(8):813-814. Available at: https://fhop.ucsf.edu/sites/fhop.ucsf.edu/files/custom_download/Unintended%20consequences%20of%20screening%20for%20social%20determinants.pdf (accessed August 31, 2020).
- Isham, G. J., D. J. Zimmerman, D. A. Kindig, and G. W. Hornseth. 2013. HealthPartners adopts community business model to deepen focus on nonclinical factors of health outcomes. Health Affairs (Millwood) 32(8):1446-1452. https://doi.org/10.1377/hlthaff.2011.0567