Alternatives to Antibiotics: Why and How
The antibiotic resistance problem is caused by the evolution and transfer of genes that confer resistance to medically important antibiotics into human pathogens. The acquisition of such resistance genes by pathogens complicates disease treatment, increases health care costs, and increases morbidity and mortality in humans and animals. As antibiotic resistance continues to evolve, antibiotics of so-called last resort become even more precious. Reducing or preventing the dissemination of antibiotic resistance genes into human pathogens is currently of high international importance.
The complex factors that have led to the antibiotic resistance problem are revealed when examining potential solutions to reduce or prevent this problem. First, more than 70 years of antibiotic use have already selected for diverse and highly mobile antibiotic resistance genes in human pathogens and related bacteria. These resistant bacteria spread in the environment via water, air, wildlife, and humans, so targeted mitigation strategies are needed to decrease the environmental dissemination of antibiotic-resistant bacteria from “hot spots” of potential resistance development. Second, highly mobile resistance genes can be horizontally transferred from one bacterium to another. Resistance gene transfer events can be stimulated by antibiotics themselves. Therefore, prudent use of antibiotics is one potential mitigation strategy to slow the spread of resistance genes among bacteria. Finally, novel resistance genes that are not yet clinically relevant can emerge from the vast reservoirs of environmental and commensal bacteria due to selective pressure. Compared to anthropogenically selected resistance genes, these resistance genes are not commonly found on mobile genetic elements (MGEs), and so they face a multistep path of selection onto MGEs—such as integrons, transposons, and plasmids—before they will arrive in a human pathogen [1]. One example of this is the emergence of the clinically relevant and plasmid-borne CTX-M-5 extended-spectrum beta-lactamases from the chromosome of the commensal bacterium Kluyvera ascorbata [2]. Antibiotic prudency is also important to decrease the selective pressure for the eventual emergence of as yet unknown antibiotic-resistance genes.
Antibiotic prudency is the use of antibiotics only when they are expressly needed and at the most appropriate dose for disease treatment. This is a nebulous concept that is difficult to define—particularly in cases of human health when the health of the individual, not the population, is of immediate importance. Nonetheless, central to executing antibiotic prudency is the availability of efficacious alternatives to antibiotics. The use of antibiotic alternatives to promote health and reduce disease will decrease antibiotic use, thereby decreasing selective pressure for the emergence and transmission of antibiotic-resistance genes.
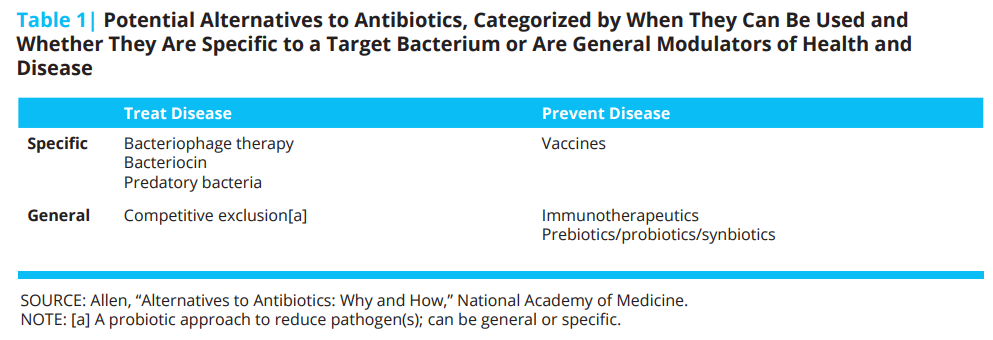
Antibiotics are used for disease treatment and prevention in both humans and animals. Historically, antibiotics have also been used for improving growth promotion in food-producing animals, although this practice is no longer allowed in the United States. These multiple uses can be attended to by various alternatives, some of which are presented in Table 1 [3].
Numerous alternatives to antibiotics exist for treating specific diseases, including bacteriophage therapy [4], predatory bacteria [5], bacteriocins [6], and competitive exclusion of pathogens [7]. Unfortunately, none have consistently demonstrated efficacy comparable to antibiotic treatment. The advantage to these approaches, however, is that only the disease-causing bacterium is targeted by the treatment, and not the other members of the host’s commensal, beneficial microbial communities. This is in contrast to most antibiotics, which generally have collateral effects on commensal bacteria in addition to the pathogenic target. Further development of these specific approaches for disease treatment is warranted to improve deliverability, potency, and reliability as antibiotic alternatives.
Bacteriophage, or phage, therapy is among the most heavily researched of the alternatives to antibiotics for disease treatment. Phage viruses infect bacteria, and the use of phages to treat bacterial diseases has been investigated for over a century. Several phage therapeutic products are available and in use in Eastern Europe, but variable efficacy tends to prevent phage therapeutic products from the market in the United States [8]. Advantages of phage therapy include specificity for a target bacterial population and efficacy on topical or mucosal infections. Among the disadvantages: the therapy requires knowledge of the target bacterium and sufficiently high populations of the target bacterium, and resistance can develop. So the therapeutic phage would need to be updated.
Although disease treatment is the most obvious use of antibiotics, a great deal of antibiotics are used for disease prevention. In swine, roughly half of all antibiotic usage is for disease prevention [9, 10]. Disease prevention in both humans and animals has been advanced by contemporary knowledge of sanitation and nutrition. Continued improvements in sanitation and nutrition, particularly in animal husbandry, will contribute to decreased antibiotic use. In addition to these seemingly primitive interventions, molecular developments such as vaccination have been instrumental in reducing primary and secondary bacterial infections that would have necessitated antibiotic use. Vaccines continue to be one of the most important ways to prevent infections.
Another promising intervention is the use of immunotherapeutics, which are molecules that boost the host immune system to generally prevent disease at infection-prone times. One successful immunotherapeutic in human health is pegfilgrastim, a granulocyte colony-stimulating factor (G-CSF) that is used to induce neutrophil production in chemotherapeutic patients with low neutrophil counts [11]. Maintaining appropriate neutrophil numbers in the blood helps the immune system to prevent infections. Immunotherapeutics have also been exploited for agricultural purposes with pegbovigrastim, a bovine G-CSF that is administered to cattle prior to parturition to boost the immune system and decrease the incidence of mastitis. The advantage of these immunotherapeutics is that they generally boost the immune system to prevent infectious disease. The disadvantage is that the timing of delivery needs to be precise, which is a potential challenge for on-farm applications.
Finally, the use of pro-, pre-, or synbiotics to modulate the gut microbial community toward health has demonstrated inconsistent efficacy [12]. Probiotics are living organisms that are intentionally fed to a host and are typically known as “good” bacteria, prebiotics are molecular precursors to expand the presence of the existing “good” gut microbiota of a host, and synbiotics are a combination of both. All of these “-biotics” are designed to affect the gut microbiota in a way that improves health. However, the gut microbial community of mammals is a complex consortium of more than 500 different bacterial species, and researchers currently lack knowledge of the precise mechanism of how each member contributes to host health. This lack of understanding likely contributes to the variable results with modulating the gut microbial community as an alternative to antibiotics. Investigations of how gut bacteria interact with each other and with their animal hosts is currently an active area of research worldwide.
In summary, solutions to the antibiotic-resistance problem are multifaceted and include reducing the use of antibiotics via the use of alternative products. No one alternative will replace all uses of antibiotics, because a variety of specific and general methods are needed to both prevent and treat disease. Immunotherapeutics, vaccines, and gut microbiota modulation could be among the most promising approaches.
Join the conversation!
![]() Tweet this! As antibiotic resistance continues to evolve, solutions are more important than ever. A look at alternatives: http://bit.ly/2uAHzZ7
Tweet this! As antibiotic resistance continues to evolve, solutions are more important than ever. A look at alternatives: http://bit.ly/2uAHzZ7
![]() Tweet this! No one alternative will replace all uses of antibiotics to reduce antibiotic resistance. Here are some options: http://bit.ly/2uAHzZ7
Tweet this! No one alternative will replace all uses of antibiotics to reduce antibiotic resistance. Here are some options: http://bit.ly/2uAHzZ7
![]() Tweet this! New paper from @theNAMedicine identifies several alternatives to antibiotics in treating/preventing diseases: http://bit.ly/2uAHzZ7
Tweet this! New paper from @theNAMedicine identifies several alternatives to antibiotics in treating/preventing diseases: http://bit.ly/2uAHzZ7
Download the graphic below and share it on social media!
References
- Stokes, H. W., and M. R. Gillings. 2011. Gene flow, mobile genetic elements and the recruitment of antibiotic resistance genes into gram‐negative pathogens. FEMS Microbiology Reviews 35(5):790-819. https://doi.org/10.1111/j.1574-6976.2011.00273.x
- Humeniuk, C., G. Arlet, V. Gautier, P. Grimont, R. Labia, and A. Philippon. 2002. ß-lactamases of Kluyvera ascorbata, probable progenitors of some plasmid-encoded CTX-M types. Antimicrobial Agents and Chemotherapy 46(9):3045-3049. https://doi.org/10.1128/AAC.46.9.3045-3049.2002
- Allen, H. K., U. Y. Levine, T. Looft, M. Bandrick, and T. A. Casey. 2013. Treatment, promotion, commotion: Antibiotic alternatives in food-producing animals. Trends in Microbiology 21(3):114-119. https://doi.org/10.1016/j.tim.2012.11.001
- Chan, B. K., S. T. Abedon, and C. Loc-Carrillo. 2013. Phage cocktails and the future of phage therapy. Future Microbiology 8(6):769-783. https://doi.org/10.2217/fmb.13.47
- Kadouri, D. E., K. To, R. M. Q. Shanks, and Y. Doi. 2013. Predatory bacteria: A potential ally against multidrug-resistant gram-negative pathogens. PLoS One 8(5):e63397. https://doi.org/10.1371/journal.pone.0063397
- Cotter, P. D., R. P. Ross, and C. Hill. 2013. Bacteriocins—a viable alternative to antibiotics? Nature Reviews Microbiology 11:95-105. https://doi.org/10.1038/nrmicro2937
- Schneitz, C. 2005. Competitive exclusion in poultry––30 years of research. Food Control 16(8):657-667. https://doi.org/10.1016/j.foodcont.2004.06.002
- Abedon, S. T., S. J. Kuhl, B. G. Blasdel, and E. M. Kutter. 2011. Phage treatment of human infections. Bacteriophage 1(2):66-85. https://doi.org/10.4161/bact.1.2.15845
- Apley, M. D., E. J. Bush, R. B. Morrison, R. S. Singer, and H. Snelson. 2012. Use estimates of in-feed antimicrobials in swine production in the United States. Foodborne Pathogens and Disease 9(3):272-279. Available at: http://singerepidemiology.org/publication/use-estimates-of-in-feed-antimicrobials-in-swine-production-in-the-united-states/ (accessed August 31, 2020).
- National Animal Health Monitoring System. 2015. Swine 2012: Part II: Reference of swine health and health management in the United States, 2012. Fort Collins, CO: US Department of Agriculture. Available at: https://www.aphis.usda.gov/animal_health/nahms/swine/downloads/swine2012/Swine2012_dr_PartII.pdf (accessed January 27, 2017).
- Molineux, G. 2004. The design and development of pegfilgrastim (PEG-rmetHuG-CSF, Neulasta®). Current Pharmaceutical Design 10(11):1235-1244. https://doi.org/10.2174/1381612043452613
- Gaggia, F., P. Mattarelli, and B. Biavati. 2010. Probiotics and prebiotics in animal feeding for safe food production. International Journal of Food Microbiology 141:S15-S28. https://doi.org/10.1016/j.ijfoodmicro.2010.02.031